Preparation for implantation always begins with the first consultation, where a panoramic image and computed tomography are taken, and then a treatment plan is developed - based on the images, the doctor will tell you in great detail about all possible treatment options in your case.
Each patient at the Smile-at-Once clinic is assigned an individual manager who accompanies them at every stage of treatment. We are in touch with you 24 hours a day, 7 days a week - you can ask any important questions and get answers to them!
If you decide to undergo implantation on the day of the first consultation, a detailed treatment plan is drawn up together with the doctor and manager, an agreement is concluded, and a date for tests is set (if they cannot be carried out on the same day). If you need to think and weigh everything, after making a decision, you can contact your manager or clinic administrator - we will give full recommendations on the further stages of treatment.
How is diagnostics carried out?
At the first stage, a computed tomography (abbreviated as CT) is performed. This is a study that allows you to obtain a three-dimensional image of the patient’s entire jaw system. Based on these data, the volume and quality of bone tissue, the position of the nerves and sinuses are assessed. The doctor will determine whether there are any pathologies of the jaw system that may become an obstacle to implantation (cysts, granulomas, foci of chronic periodontitis, etc.).
As a rule, we perform CT scans using our own diagnostic equipment.
Tomographs for dentists and specialized centers differ primarily in their resolution. Accordingly, the higher the magnetic field strength of the device, the more detailed the images will be and the more informative the research itself will be.
In most situations, the dental apparatus is more than enough: the teeth and jaw system are not kidneys or the brain, where a special configuration of sections and high resolution are required. But in difficult situations, if the doctor has to work not only with the jaw system, but also use other bones of the skull (in particular, the zygomatic bone), a more detailed and high-quality image is needed, and this can only be obtained with professional and more expensive diagnostic equipment. Therefore, in such situations, we refer the patient to a specialized diagnostic center to conduct CT and even MSCT (multispiral computed tomography).
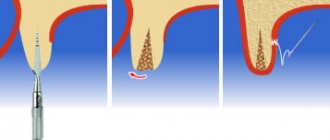
Osteoplasty
If the volume of bone tissue is insufficient to install an implant, they resort to osteoplasty - bone augmentation. The bone graft will provide the necessary foundation for the artificial root. There are different methods:
- sinus lift (only for the upper jaw);
- guided bone regeneration; splitting of the alveolar ridge;
- replantation of bone blocks.
Each of them has indications for use. Implants can be placed at the same time as bone reconstruction. But more often they wait 4-6 months between operations. The implantologist decides which method to choose based on X-ray data.
Osteoplasty can be avoided when the patient is missing more than 3 consecutive teeth. The doctor has the opportunity to install implants in the basal and cortical layers of the jaw, which do not atrophy.
Why take tests before dental implantation?
Our patients undergo blood tests and, in some cases, urine tests before dental implantation. They allow you to assess the patient’s current health status, clarify blood clotting readings, the presence or absence of viral or bacterial infections in the acute period.
After the tests, we are unlikely to refuse you dental implantation - when planning treatment, you already fill out a questionnaire that allows us to draw conclusions about the state of your health. But the tests will allow us to understand whether implantation can be carried out right now or whether it makes sense to postpone it for a while and put chronic diseases into remission.
We especially insist on testing for women over 50 years of age: an expanded complex is provided for them, since during this period it is necessary to take into account that some body functions work slightly differently. You can read more about the specifics of implantation in women in our special article.
An expanded list of tests is also provided if the patient plans to undergo implantation under general anesthesia or sedation.
Primary preparation
This is a set of measures that will prepare the oral cavity for future intervention. They are as follows:
- Initial examination. The doctor asks questions about your general health and examines your mouth. Based on the results of the examination, he issues referrals for laboratory tests and examinations, and refers to related specialists if necessary. The data is sent to the general practitioner, who draws up a report on the state of health.
- Actually tests before dental implantation and general examinations. This is necessary in order to exclude possible contraindications. Based on the diagnostic results, the therapist issues a conclusion and recommendations for surgery. If relative contraindications were identified during diagnostic measures, treatment is prescribed - the operation is performed only after the body has been restored.
- Diagnosis of the condition of the dental system: x-ray, computed tomography, orthopantomogram. The pre-dental implant examination is critical in planning and performing the procedure. Images of the jaws in three planes provide the specialist with information about the condition of the bone tissue, features of the maxillary sinuses, nerve canals, and mandibular joints. Knowledge about the parameters of bone tissue allows you to make the right decision - to assess whether its volume is sufficient. Based on the results of the examination, the doctor decides whether implantation can be performed or whether preliminary measures should be taken - for example, bone grafting (sinus lift, etc.).
Should I see a therapist or other doctor?
We strongly ask our patients to approach filling out the health questionnaire responsibly - it is important for us to know how your body may behave during the operation to install implants and to provide for all the nuances. Therefore, you must tell your doctor in advance that you are registered with a specialized specialist, especially if you have diabetes and pathologies of the cardiovascular system. In this case, we will need a doctor's opinion on what stage the disease is at. You may also have to do an ECG, ultrasound of the thyroid gland, take allergy tests - everything is individual.
We perform implantation in cases of diabetes mellitus and problems with blood pressure or the cardiovascular system in general. But it is important that the disease is in the stage of compensation and remission. In addition, you definitely need to be in touch with your endocrinologist or cardiologist and know what medications you need to take before and after surgery.”
Namdakov Nikolay Vladimirovich, maxillofacial surgeon, implantologist, orthopedist with more than 18 years of experience make an appointment
Consultation with an implant surgeon
Before installing implants, you need to visit an implantologist at least twice. To obtain primary data about the clinical situation, the doctor:
- interviews and examines the patient;
- collects anamnesis (information about the person himself and the development of the disease);
- Refers the patient for x-ray and laboratory diagnostics.
At the initial consultation, the proposed implantation technique and duration of treatment are determined. The exact timing of implantation and cost can only be found out after a complete examination.
Why is photometry needed and what is condylography?
Photometry is the taking of photo parameters, simply - photographing with an open and closed mouth, with and without a smile, frontal and profile. Photographs are needed not only to evaluate the result before and after, but also to develop an individual denture.
When developing a prosthetic model, we use the principles of the “golden ratio” - the rules for dividing the face into segments. Thanks to prosthetics and implantation, you can restore your bite, get rid of wrinkles, and change the lower third of your face. That is, to make you more attractive.
Condylography is the measurement of parameters of occlusion (closing of the jaws) and the functioning of the temporomandibular joint; in fact, it is a functional diagnosis. Our clinic uses a HIP plane analyzer, a facebow and an articulator. Together, they allow you to assess how the entire jaw system will work after the installation of a denture, how you need to correct your bite and straighten the position of the two jaws relative to each other in order to relieve the load on the temporomandibular joint and allow you to chew without discomfort.
Of course, such a procedure is primarily necessary when a large number of teeth are complete or missing. With single restorations or if there are no malocclusions, such a diagnosis makes no sense.
Such parameters are taken twice – at the stage of preparation for dental implantation, and also after taking impressions before installing the prosthesis. In case of complete absence of teeth, as well as after their partial removal and fixation of implants, the bite changes slightly - this must be taken into account so that the prosthesis is comfortable throughout its entire service life.
The task of our doctors is to make not only beautiful dentures, but also to restore the function of the teeth. So that you can chew any food without pain and with pleasure.
List of tests if there are obstacles to implantation
- general urine and blood;
- blood for sugar;
- hormonal studies;
- blood group and Rh factor;
- hemostasiogram;
- biochemical blood test (bilirubin, ESR, creatinine, amylase and other indicators).
Women are also required to undergo hormone tests (TSH, T3, T4, estradiol, parathyroid hormone). Indicators outside the normal range are relative contraindications for implantation, requiring correction and treatment.
In our Center, in preparation for surgery, you can take tests without leaving the clinic. The staff anesthesiologist will perform a cardiogram. The collection of material for other studies is carried out by a nurse; the work is carried out by employees of the INVITRO laboratory under a contract. Results are provided within a day or every other day.
Process planning and 3D modeling
After a CT scan and recording of all bite parameters, the patient goes home to prepare for implantation - this stage goes unnoticed for you. Meanwhile, one of the most difficult, but at the same time interesting periods begins for the doctor - visual modeling of the treatment process. All received data is loaded into a computer program, in which the implantologist recreates a model of the jaw system and parts of the patient’s cranial bones, carefully measures the locations for implants, determines their number, and even creates a prototype of the future prosthesis.
The key feature of our center is that in addition to computer visualization, we work out details on individual models. In complex cases, we print lithographic models on a 3D printer - in fact, these are copies of jaws and parts of the skull created from special plastic. Such “artificial bones” replicate the density of natural ones - the doctor implants the implants, evaluates their progress and deviation during positioning. Due to this, he takes into account all such nuances in advance, and not during the actual operation.
All of our implant surgeons have knowledge of orthopedics - it is impossible to carry out implantation in any other way, because the implants must be installed so that they are suitable for subsequent prosthetics. However, already at this stage, an orthopedic gnathologist must be involved - this is a doctor who creates prostheses, simultaneously correcting and restoring the functioning of the jaw joint.
Contraindications that exclude implantation
There are a number of absolute contraindications to dental implantation, including:
- Blood pathologies that cause clotting disorders;
- Autoimmune diseases;
- Alcohol and drug addiction;
- Allergic reaction to anesthetics;
- Diseases of the skeletal system;
- Oncological diseases.
If such contraindications are identified, implantation is impossible and you will most likely be offered alternative methods for restoring lost teeth. In addition to absolute contraindications, implantation also has time restrictions.
Thus, the implantation of dental implants is not carried out during pregnancy and lactation, in case of untreated caries, pulpitis, periodontitis and periodontal disease, general infectious diseases of the body, sexually transmitted diseases, and poor condition of the immune system. In order to be able to perform implantation, you need to eliminate all these conditions, re-take the tests and then plan the operation to implant the implants.
IMPORTANT: Previously, diabetes mellitus, periodontitis, periodontal disease, and tobacco addiction were considered absolute contraindications to dental implantation. But implantation technologies are constantly being improved and now patients with these diseases, as well as smokers, can easily restore their teeth with implantation; it’s just that performing surgery on patients at risk requires the correct selection of techniques and detailed planning.
How is the oral cavity prepared?
Before dental implantation, regardless of how many teeth are planned to be restored, it is necessary to prepare the entire oral cavity. It is very important to eliminate any inflammatory processes, since their development is provoked by microbes and bacteria that can get into the hole and thereby cause inflammation of the tissues around the implant. That is why the oral cavity should be as sterile as possible.
Treatment of caries, pulpitis
All inflammatory processes of periodontal tissues, dental diseases (caries, pulpitis, periodontitis) and even ordinary deposits on the enamel are nothing more than bacteria. This means that during implantation, they can get inside the wound and cause tissue inflammation. The risk of developing peri-implantitis and rejection of the structure increases. Therefore, it is very important to treat the teeth that are directly adjacent to the defect area, as well as on the opposite jaw, so that the surgical area is sterile. If a large number of teeth are destroyed, then, of course, it is advisable to cure them all.
Removing dental plaque
Cleaning before implantation is also a mandatory preparation step. As with tooth decay, plaque and tartar can cause inflammation. The cleaning is carried out deep, that is, deposits are necessarily removed from under the gums. Therefore, if there is a need, gum curettage is prescribed instead of the traditional hygiene complex.
At what point do you agree on the timing of treatment?
Treatment periods can range from three months to several years, depending on the complexity of the clinical case. Of course, if a patient comes to our clinic with a request to restore his tooth in one day, we can do it. But only if the patient’s clinical condition allows it. Otherwise, rejection may occur.
Also, the time of dental implantation depends on the process of bone tissue restoration and the presence of concomitant diseases. I knew examples where the engraftment process lasted longer in young people than, for example, in older patients. So everything is individual.
Do I need to remove teeth before getting dental implants?
This is a very painful and pressing question that many patients ask. It is relevant only for those situations where most of the dentition is missing - for example, chewing teeth on both sides, and the front ones are preserved in fairly good condition (according to the patient himself). Of course, you don’t want to lose them, but placing implants in the area of the lateral teeth, especially against the background of an inflammatory process, is completely pointless - there is a high risk of their rejection due to inflammation and increased mobility.
Remember! It is not the patient who evaluates the condition of the teeth, but the attending physician! You may not see micromobility, you may not know that you have an average or even advanced stage of periodontitis. You think your teeth look good, but they will be much more trouble than real benefit.
Remember that teeth are a source of infection. It is on them, on their porous surface, that a huge number of pathogenic microorganisms accumulate. That is why, if periodontitis exists, it is impossible to get rid of it - you can only slow down its development.
What do you RISK if you DO NOT remove living teeth?
What do you RISK if you DO NOT remove living teeth?
| Bad breath | It will not go away, because inflammation persists, even if it is transferred to the stage of relative remission. |
| Risk of implant rejection | The risk of developing peri-implantitis increases, both in the short and long term. Inflammation can spread to the tissue around the implants, leading to their rejection. |
| Bone loss and again implant rejection | Periodontitis has no cure, so bone loss in the area of living teeth will progress. Yes, this process can be long, and right now there are no signs of trouble, only “the roots are a little exposed,” patients say. But this means that the bone is already shrinking and losing its density. Our jaw system is designed so that all teeth support each other. As soon as at least one tooth loses its fixation, this affects the neighbors. By installing implants near moving teeth, the implantologist in advance dooms the structure to problems in the future. The chewing load will be distributed incorrectly and displacement of the implants may occur. The bone will also decrease around adjacent implants, which will lead to exposure of their tops. Likewise, if the teeth were previously treated and if there was a cyst, in such situations there is already little bone initially and the loss will increase. |
| Development of gastrointestinal problems | When there is a source of infection in the oral cavity (even if it is just plaque or stone), all pathogenic bacteria certainly enter the stomach along with food. Take care of yourself: if you have problems with your teeth, how does your digestive tract react to this? There is probably pain, discomfort, bloating, and increased gas formation. |
| Development of pyelonephritis | Some bacteria that cause periodontitis contain antigens that are similar to kidney and heart tissue cells. Therefore, as soon as our immunity begins to fight inflammation, it automatically affects the kidney tissue and destroys them... This is why the connection between the presence of inflammation in the oral cavity and the development of both pyelonephritis and pathologies of the cardiovascular system has been proven. Even if the disease is in a sluggish form. |
By preserving living teeth with periodontitis, we risk losing the entire structure on implants!
Contraindications that exclude implantation
There are a number of absolute contraindications to dental implantation, including:
- Blood pathologies that cause clotting disorders;
- Autoimmune diseases;
- Alcohol and drug addiction;
- Allergic reaction to anesthetics;
- Diseases of the skeletal system;
- Oncological diseases.
If such contraindications are identified, implantation is impossible and you will most likely be offered alternative methods for restoring lost teeth. In addition to absolute contraindications, implantation also has time restrictions.
Thus, the implantation of dental implants is not carried out during pregnancy and lactation, in case of untreated caries, pulpitis, periodontitis and periodontal disease, general infectious diseases of the body, sexually transmitted diseases, and poor condition of the immune system. In order to be able to perform implantation, you need to eliminate all these conditions, re-take the tests and then plan the operation to implant the implants.
IMPORTANT: Previously, diabetes mellitus, periodontitis, periodontal disease, and tobacco addiction were considered absolute contraindications to dental implantation. But implantation technologies are constantly being improved and now patients with these diseases, as well as smokers, can easily restore their teeth with implantation; it’s just that performing surgery on patients at risk requires the correct selection of techniques and detailed planning.
Is it possible to restore teeth on only one jaw?
It is possible, but the doctors at the Smile-at-Once clinic do not practice this. Yes, we can restore only one jaw, but the teeth will not have antagonists, that is, support. And it's not just that you won't be able to chew. The problem is much more serious - we will not have the conditions to create a fully functioning and properly functioning jaw system.
Firstly, if a tooth is missing on the opposite jaw, the living teeth can literally shift and even fall out of the socket. Indeed, over time, due to the lack of chewing pressure on them, blood circulation deteriorates, and the bone tissue, along with the periodontal ligaments, weakens. It’s the same with implants - they have no support, the crowns of the prosthesis have nothing to come into contact with unless the antagonists are restored. Nutrition of bone cells, which is so important for implant healing, is difficult due to impaired blood circulation.
Secondly, if you left some of your teeth, then with a 99% probability they have changed their original position - due to periodontitis, due to malocclusion, due to loss of bone tissue. That is, they moved sideways and definitely became shorter/longer (this is individual). In such a situation, we again cannot always restore the correct position of the two jaws relative to each other.
We need an integrated approach! If you are currently only ready to undergo implantation on one jaw, do not ignore the second. For a while, we can install a removable or conditionally removable denture - this will allow us to straighten the bite, ensure normal functioning of the jaw joint - you will be able to chew and enjoy your new teeth. Otherwise, you will understand that after implantation almost nothing has changed - only the smile has become beautiful, but the problems continue.
How is the first consultation with the patient before implantation?
In my opinion, at the first consultation it is very important to establish contact with the patient. At the same time, I never start a conversation with the question: “What are you complaining about?”, but follow an algorithm that implies a certain order of actions:
- finding out the reason for the patient’s visit;
- determining the degree of his awareness of the problem;
- bringing him up to speed;
- clarification of the patient’s wishes regarding the final result of treatment;
- awareness of its temporary capabilities;
- interest in the patient's readiness to begin treatment;
- taking photographs of the oral cavity;
- invitation to a consultation with other specialists (orthopedist, orthodontist) to identify all existing problems;
- carrying out complex treatment before implantation.
Recommendations for the patient: what to do before the operation to install implants
So, all the stages of preparation and planning have been completed, the date for installing the implants has been set, all that’s left to do is sleep, eat and get ready for the speedy completion of the treatment, after which you will find a beautiful smile and will finally be able to eat without pain. And those products that you really want, and not just can chew.
Please charge your phone fully so that after surgery you can contact your loved ones and stay in touch with your doctor. You can also leave your phone at the reception desk - after the operation it will be completely ready for communication.
It is advisable to arrive at the clinic 20-30 minutes before the start of the operation. Please do not be late, especially if general anesthesia or sedation is planned. We may have several operations on one day, and between them we need to have time to prepare the operating rooms.
What can you eat
- 2-3 days before surgery, it is advisable to follow a “light” diet - remove fatty, salty, fried, and rich foods from the diet. It is better to give preference to chicken, vegetables and fruits (apples, pears), fish, dairy products,
- do not drink coffee, tea, or alcohol for 2-3 days, as they provoke sudden changes in blood pressure - this can lead to bleeding after surgery,
- eat 4 hours before surgery. DO NOT overeat! Light but filling lunch/breakfast. This could be eggs, a small piece of meat and steamed vegetables, various cereals. Eat complex carbohydrates as they keep you full for a longer period of time.
- Before the operation, you can only drink water - stop taking it 2 hours before.
How to dress
- Wear light clothing that does not restrict movement. You can take with you a warm jacket with a zipper or buttons in the front so that you can simply take it off (not over your head) or throw it on if it gets cold,
- It is advisable that clothing be sleeveless, since installing implants is a surgical operation and although protective aprons are used, clothing can become dirty,
- It is advisable for women not to wear makeup or to wash it off at the clinic. You especially need to give up lipstick. During installation of the implants, a protective balm will be used to prevent dry lips,
- You should not paint or extend your nails, since special infrared sensors placed on the fingers are used to monitor the respiratory function and the patient’s condition during implantation. Varnish, acrylic and gel coatings can impede data transfer. Moreover, anesthesiologists monitor the effect of anesthesia and the patient's condition by observing the nail plates.
How to perform hygiene
- immediately before the operation, brush your teeth well with a brush and toothpaste, use an irrigator,
- immediately before leaving the house, that is, after eating, rinse your mouth with a solution of Chlorhexidine, Miramistin or any other antiseptic.
Do I need to take medications?
- necessary if they were prescribed to you by your attending physician,
- It is important that blood pressure readings are within normal limits. If you know that your blood pressure will rise as soon as you cross the threshold of a clinic or implantologist’s office, discuss this with your doctor in advance: together you will choose the optimal dose of the drug and determine how long before surgery it is best to take it,
- We also recommend that patients with panic fear breathe xenon before surgery - this is a useful medical gas that will relax, lift your spirits, and improve the general condition of the body. Read more about xenon therapy here.
- it is also necessary to maintain normal blood sugar levels - take all prescribed medications as prescribed by the endocrinologist,
- prohibited: anticoagulants, aspirin and drugs based on it, non-steroidal anti-inflammatory drugs and blood thinners. All of them increase the risk of postoperative bleeding,
- During preparation for implantation, you cannot undergo intensive therapy for the treatment of other diseases (hepatitis, cancer, tumors) associated with taking a large number of medications or radiation.
WHAT SHOULD BE IN YOUR HOME from medicines
When you return home, you will feel weak and have difficulty concentrating. Therefore, we strongly recommend that you prepare in advance - check out our useful reminder so you don’t forget to buy anything in advance.
- at the pharmacy: buy all the tablets and solutions for oral baths in advance - especially for painkillers. All recommendations will be given to you by the attending physician even before the operation. Also in your first aid kit you should have a thermometer to measure and control body temperature, a sterile bandage or napkin to apply to the wound area and stop bleeding,
- There should be a supply of ice in the freezer to reduce the risk of swelling. If swelling occurs, ice will help reduce its spread.
WHAT SHOULD BE FOOD AT HOME
- what to buy in the store: soft cottage cheese, various yoghurts, you can buy baby food in jars - give preference to meat products and vegetables. In the first 2 days, if you do not receive dentures immediately, your diet will consist exclusively of liquid and puree foods,
- What to cook at home: make your own broth. This can also be a regular soup, but it is better to use a blender before using it. On the first day, you can also afford mashed boiled vegetables and soft baby food. IMPORTANT! All food should be warm - neither hot nor cold,
- what you can drink: water is a priority, but you can indulge in warm herbal tea, especially one that has a sedative effect on the nervous system. Be sure to buy a straw - if you need stitches, you're better off eating this way.
Prepare a sleeping place in advance, stock up on interesting films or favorite music - they will help distract you on the first day after surgery and not focus on every sensation. The body has suffered stress and the tissues begin to rehabilitate – discomfort is normal. You will find a more detailed list of how to care for your oral cavity, how to eat, which symptoms are normal, and which should see a doctor in our post-implantation leaflet.
Checklist: check yourself!
| What to buy at the pharmacy | What to buy in the supermarket | What to cook at home |
|
|
|
We have quite a lot of recommendations on how to prepare for dental implantation. But we tried to take into account as much as possible so that you don’t forget anything. You can download our checklist and check yourself so that when you return after surgery, you have everything you need not only in stock, but also at hand. And remember, dental implantation is an operation that is sometimes even easier than complex tooth extraction. The main thing is a positive attitude and compliance with the instructions!
Examination of jaw tissue before implantation
The examination before implantation gives a detailed picture of the condition of the bone tissue: structure, thickness - whether its volume is sufficient for the introduction of an artificial root. The information obtained helps the doctor decide on the need for preliminary osteoplastic surgery or treatment, for example, if periodontitis or a tooth root cyst is detected.
An X-ray is required before dental implantation. In some cases, an orthopantomogram is required - a panoramic image of the jaw.
However, in order to model the future dentition and clearly show what result awaits the patient after implantation, an extensive examination will be required.
CT before dental implantation differs from x-rays and orthopantomograms in that it makes it possible to obtain a three-dimensional image of the jaw. This approach allows you to evaluate all the necessary parameters, including studying the location of the maxillary sinuses, diagnosing inflammatory processes and tissue formations.