The importance of prosthetics
The main reason for refusals to install dentures is associated with the erroneous opinion of old-school dentists about the mandatory depulpation (removal of the nerve) of teeth before prosthetics. Before dispelling this myth, it is necessary to recall the importance of timely prosthetics.
Without an adequate prosthesis, neighboring healthy teeth begin to carry an unusual load, which leads to their increased wear, mobility and early loss. In addition, in the absence of even one tooth, speech defects appear, chewing functions are disrupted, bite pathologies occur, and even facial proportions are distorted.
Removal of the tooth nerve: indications for the procedure
The most common reason that can lead to the need to remove the nerve of a tooth is pulpitis. This is an inflammation of the dental pulp, which occurs as a result of advanced caries. In healthy teeth, the pulp is protected by tooth enamel, but with carious lesions, it is exposed and begins to become inflamed from any influence. As a result, the patient feels acute pain, which can only be eliminated by removing the damaged nerve of the tooth.
Other indications for depulpation include:
- The need to grind tooth enamel when installing a crown;
- Mechanical damage to the tooth - the presence of chipped enamel;
- The presence of deep carious lesions, for the prevention of pulpitis in the future.
In the situations listed above, the dentist may decide to remove the pulp, especially if the tooth is causing pain and discomfort to the patient.
Causes of frequent depulpations
Why do orthopedists so often remove pulp from teeth? The main reason lies in the desire of doctors to play it safe and avoid complications after prosthetics. The fact is that teeth have a porous structure. Pores are dentinal canals that run from the enamel to the pulp of the tooth. During grinding of teeth for a crown, mechanical irritation of the pulp may occur through these dentinal canals.
And at the last stage of fixing the prosthesis, there is a toxic effect of cement. And as a result - infection and death of the pulp. However, this does not allow us to consider depulpation as a prevention of complications, since this procedure is inevitably associated with the risk of developing periodontal pathologies. After all, no one suggests removing the appendicitis for preventive purposes. Living teeth retain their stability much longer.
Whereas teeth subjected to depulpation become extremely fragile and are more susceptible to destruction, losing their shock-absorbing function.
Technique for installing a crown on a living tooth
The procedure is performed in several stages (Fig. 1). First of all, an initial examination and diagnosis will be carried out. At this appointment, a treatment plan will be developed. The dentist will advise you to perform hygienic cleaning of the mouth in order to most accurately select the color of the crown. Treatment of caries and pulpitis is mandatory. The doctor will not deal with prosthetics for a diseased tooth.
At the next appointment, the specialist will prepare the tooth to give it the desired shape. He will remove enamel equal to the thickness of the crown. The procedure is quite painful, so it is performed under anesthesia.
Rice. 1. The process of installing a crown on a living tooth
To make a crown, the doctor will take an impression, from which a plaster model is first made, and then a full-fledged prosthesis is poured. During the manufacturing period, a temporary crown is placed on the tooth. Trying it on will show how accurately it is made. Next, the crown is fixed with dental cement and treated with antiseptic agents.
Knowledge and experience of orthopedists
Of great importance in the issue of prosthetics without depulpation is the knowledge of orthopedic doctors about the safety zones of the crown parts of teeth. Safety zones are those areas of the tooth within which you can safely grind the tooth tissue without damaging the pulp.
The canines have slightly more such tissue than the lateral incisors. The age of the patient is also important: the older the person, the less likely the pulp is to be damaged.
Contact our clinic for a consultation on prosthetics without depulpation, and we will definitely find the right solution for you!
Dental prosthetics in our clinic. Types of dental crowns and methods of their manufacture
Do I need to depulp my teeth before installing crowns or bridges?
Short answer: in 99% of cases, when the tooth is correctly positioned in the dentition, this is not necessary. Very rarely (if there is a significant tilt or protrusion of the tooth, when the artificial crown does not repeat the previous shape, but corrects it) it is necessary to remove the pulp.
This issue in developed countries was resolved in the last century. However, in Russia the opinion still prevails among doctors and patients that depulpation under the crown is always necessary, or at least in most cases. Many articles on the Internet popularly explain why this is practiced. Let's look at the arguments of dentists who support depulpation, point by point.
1. A living tooth may then become ill under the crown at the most inopportune moment.
The funniest argument ever. But a living tooth with a filling can’t get sick later? Maybe. Then it is necessary to depulpate it too to prevent future pain. But just a living tooth, completely intact, can also become infected with caries in a couple of years and get sick. According to this logic, all healthy teeth should be preventively depulped. By the way, you don’t have to stop at your teeth - your leg, kidney, or head can also get sick in the future, and also at the most inopportune moment. Would patients agree to have these organs amputated now to avoid potential pain in the future? But for some reason they agree to remove the tooth pulp...
2. If the vital tooth under the crown hurts, the crown will have to be sawed, not only treatment will be required, but also re-prosthetics. This is financially expensive and aggravates the conflict situation with the patient.
Firstly, it is not at all necessary to redo the crown. A hole is carefully drilled on the chewing or lingual (near the front teeth), the canals are treated, then the endodontic access is also carefully filled with filling material. There is no significant reduction in the mechanical strength of the crown. Aesthetically, some dissonance may arise, but for others it will not be noticeable at all. In the current age of implantation, half of the crowns on implants are fixed with a screw fixation, which ends with the same filling in the middle of the ceramic crown. This does not bother patients, and orthopedic dentists initially plan for such a “leaky” crown. Secondly, the probability of a preventively pulpless tooth getting sick under a crown is no lower, even higher. And it will be much more difficult or simply impossible to treat it later (it will all end with tooth extraction). The reason is that it is often necessary to reinforce the tooth after depulpation with pins or core inlays. But getting them is far from easy, and as a result of such extraction, so little healthy tissue may remain from the tooth that it will not be possible to save it.
3. Under the crown (most often a metal-ceramic crown appears) it is necessary to grind off a lot of enamel and dentin - the pulp located in the center of the tooth will be damaged and inflamed.
There is no need to over-prepare the teeth, leaving only matchsticks - and the problem will disappear. The less hard tooth tissue is removed, the more qualified the doctor and dental technician are. The best specialists are able to perform excellent work with a thickness of 0.5 - 1 mm. Crowns 1-1.5 mm thick are also an acceptable option that does not require depulpation. But if you remove 2 mm or more from each side of the tooth, then, of course, you will catch the pulp and it is better to get rid of it in advance.
4. Even if the pulp is not damaged directly during grinding, due to a thermal burn (occurring during tooth preparation), it will still suffer, become necrotic, and sooner or later the tooth will hurt/a cyst will grow.
If you operate without water cooling or with insufficient cooling, there is a risk of thermal burns. Some doctors do not like working with a water spray: splashes fly in all directions and visualization deteriorates. However, this is a violation of the orthopedic treatment protocol. It is recommended for use in the same way as compliance with sanitary requirements. If this is observed, overheating of the pulp will not occur. However, a 2002 study by American authors found that even in the absence of water cooling, the failure rate among living teeth prepared without water cooling in the 1970s was 2.19%, and in the 1980s - 0.66%. That is, the problem of the risk of thermal burn of the pulp is clearly exaggerated. https://www.ncbi.nlm.nih.gov/pubmed/12473995
5. During preparation, dentinal tubules are exposed - through them, bacteria will make their way to the pulp and cause its inflammation.
This will happen if bacteria are given this opportunity. If the crown is made precisely, the distance between it and the dentin of the tooth is minimal, and it is also filled with a decent cement material - the chances of microbes will be as small as when placing a filling. No one depulps teeth before filling as a preventive measure, although more dentinal tubules may be exposed there than during crowning. Yes, and it is mandatory to make and cement a temporary crown immediately after preparation and impression taking. To completely prevent bacterial invasion, some qualified dentists seal the dentinal tubules with special preparations.
6. Crowns are rarely placed on completely healthy teeth. If the tooth already had a large filling or there was deep caries, then the pulp is no longer healthy. Grinding under a crown is an additional stress for it; the risk of inflammation and necrosis in such teeth is high, so depulpation is completely justified.
In fact, with a significant size of the carious cavity, the pulp of a living tooth, resisting bacterial toxins, builds replacement dentin inside its pulp chamber. Thereby obliterating the dentinal tubules and reducing the strength of external negative influences, one of which is indeed tooth preparation. That is, the risk of mechanical or thermal damage to the pulp is reduced. But the likelihood of unsuccessful endodontic treatment in such teeth, on the contrary, increases. Since obliterated canals are more difficult to process and expand, denticles may form in the tooth, which also complicates root canal treatment.
7. Theoretically, there is no need to depulp teeth, but my experience and the long-term experience of my colleagues shows that problems arise more often with living teeth.
Let's see what scientific research says about this.
An analysis carried out by Scottish colleagues revealed that in pre-pulpless teeth before prosthetics, signs of periradicular problems were identified in 50.8% of cases, in vital teeth - only in 19%. https://www.ncbi.nlm.nih.gov/pubmed/9744239
Another study by Norwegian authors recorded a 92% success rate for wearing crowns on living teeth 10 years after their installation and 83% after 25 years. https://www.ncbi.nlm.nih.gov/pubmed/9105139
But an analysis by researchers from Hong Kong showed slightly less favorable results. The survival rate of the vital pulp under single metal-ceramic crowns after 10 years is 84.4%, after 15 years - 81.2%. The survival rate of pulp under bridges is 70.8% after 10 years, 66.2% after 15 years. https://www.ncbi.nlm.nih.gov/pubmed/16011770
Based on these data, it can be assumed that the result of successful prosthetics of vital teeth depends not least on the qualifications of dentists. Therefore, doctors who refer to their own negative experiences and the experiences of other colleagues can be completely honest. The Russian dental school and the average level of training of domestic specialists is inferior to the level of Hong Kong. But we also have doctors who meet the highest world standards. For them, preventive depulpation of teeth under a crown is the same nonsense as prescribing Corvalol for a cardiologist or Oscillococcinum for a phthisiatrician.
Thus, the recommendation to remove the pulp of teeth before prosthetics is a frank recognition by the dentist of the level of his qualifications. A fairly simple and convenient hint for a patient looking for a good dentist. A much more accurate selection criterion than academic degrees, titles and diplomas gathering dust on the wall or sparkling on Internet pages.
Is it necessary to remove the tooth nerve for a crown?
Some time ago, the possibility of installing a prosthesis on a vital (living) organ was not even considered by dentists: specialists trained in the old school performed pulp removal without fail. Thus, doctors played it safe and ruled out the possibility of inflammation of the nerves under the crown. What to do if the tooth under the crown hurts when pressed?
Before installing the prosthesis, the surface must be ground, removing from 1.4 to 2.2 mm of tissue (depending on the material from which the crown will be made). The thickness of the tooth walls becomes thinner. In addition, excessive heat is transferred to the pulp during processing, which could theoretically lead to pain or the formation of granulomas.
To avoid burning the pulp when turning the tooth, it is first removed
If a tooth under a denture begins to bother the patient, the structure must be removed in order to eliminate the source of discomfort and then reinstalled. This process involves not only a lot of time, but also an investment of money. To avoid these troubles, dentists prefer to protect the patient in advance.
However, Western specialists have long abandoned this practice, because the appearance of pain does not always occur. At the same time, depulpation is guaranteed to reduce the further life of the organ, which is also not a plus for the patient. The possibility of losing a tooth completely is more dangerous than the possible risk of having the crown removed. Pulpitis in children: 7 obvious symptoms with photos
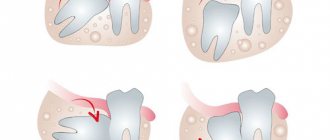
Indications for depulpation
Despite all the disadvantages of tooth depulpation, in some cases it is impossible to do without this procedure. Indications for nerve removal may include:
- advanced caries affecting the deep tissues of the tooth;
- the appearance of caries on one or more roots;
- incorrect anatomical position of the tooth;
- low landing of crowns;
- inability to prepare a tooth without opening the pulp chamber;
- inflammation of the pulp or periodontium;
- uncharacteristic anatomical features of the organ (for example, significant tilt of the tooth axis or large size of the pulp chamber).
If the dentist identifies at least one of the listed reasons in the patient, depulpation will be justified.
If caries or pulpitis is present, depulpation is necessary
Why cover a pulpless tooth with a crown?
When a patient who came to just get a filling hears from the dentist that it is recommended to cover the tooth with a crown, he is overcome with horror! After all, a crown is already an adult thing, it is no longer just a filling or restoration, in its essence it is already a prosthesis. And what kind of prosthetics can we talk about if “I just came to get a filling”? And sometimes the patient decides to consult with another doctor who offers the same thing, and then with another, and another, and another, in the hope of hearing that the tooth can simply be treated without a crown.
But things are not so simple here. If the doctor recommends covering a tooth with a crown, there are definitely indications for this. In this article we will not consider all cases. Let us touch upon only one of the most common cases - covering a pulpless tooth with a crown.
A pulpless tooth is a tooth in which the pulp (nerve) has been removed. Such a tooth is also called dead (devitalized). In addition to the nerve, the pulp also includes blood and lymphatic vessels and connective tissue. It is through the pulp that the tooth receives nutrients that provide its regenerative abilities, which a pulpless tooth does not possess at all.
The lack of regenerative abilities significantly reduces the life of a tooth. Without internal nutrition through the pulp, the tooth becomes extremely fragile. For clarity, a pulpless tooth can be compared to a dry tree - outwardly, both can have a very solid and impressive appearance, but be hollow and brittle inside.
The main risk associated with such tooth fragility is fracture or chipping. And in the case of a tooth deprived of nutrition (internal support), such chips are, as a rule, very deep, often extending under the gum. And in the case when the fracture line or chip of the tooth goes deep under the gum, it is no longer possible to restore such a tooth reliably and for a long time either with a filling or with a crown. And this is with a favorable outcome, if the tooth can, in principle, be saved after such a fracture.
But a pulpless tooth is not a death sentence at all! Yes, theoretically it can be a time bomb, but with the right approach, a pulpless tooth can last a very long time.
A competent approach in the case of a pulpless tooth includes 2 aspects:
- thoroughly treated and sealed root canals;
- mandatory (!) covering of a pulpless tooth with a crown.
The crown will protect the entire structure of the tooth (roots and remains of its coronal part) from further chipping and destruction, thereby maximizing its life, despite the actual non-viability of the pulpless tooth.
Therefore, if it so happens that you have to deal with the removal of nerves in a tooth, be sure to listen to your dentist’s recommendations regarding covering it with a crown. This is not a whim at all, but a mandatory condition for maintaining the integrity of the dentition.
Modern dentistry offers a lot of options for crowns: from the most popular metal-ceramic to the most highly aesthetic ceramic ones, the many varieties of which we will definitely talk about in one of the following articles.
Take care of your teeth and be healthy!
0
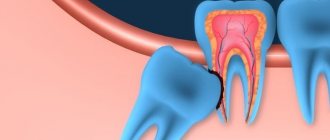
What is a nerve and how many are there in a tooth?
A tooth consists of several parts. Enamel is the top, most durable layer. It protects the underlying tissue - fairly dense but porous dentin. The infection slowly destroys it and spreads beyond the crown of the tooth, into the root canals. The first thing on the way is pulp. This is a neurovascular bundle consisting of a different number (from 1 to 3) of nerve endings and blood vessels. They are the ones who nourish the tooth, maintain its strong structure and vital functions. In addition, the pulp protects the connective tissues of the periodontium from infection and immediately reports it through pain and temperature sensitivity. When the nerve is removed, the tooth is left without nutrition and protection, and therefore becomes more fragile and susceptible to chipping. It is considered dead, although it retains its functionality.
How to remove a nerve from a tooth
A couple of decades ago, the only way to remove a nerve from a tooth was with arsenic.
After treating the caries, it was applied to the exposed area of the pulp and a temporary filling was placed. You had to walk with arsenic paste on your tooth for several days for the nerve to die. The danger was that arsenic is a poison that affects the health of the entire body. And with prolonged contact with the tooth, it could be completely destroyed. Modern methods of treating pulpitis and removing the nerve are harmless.
The doctor makes an accurate diagnosis and determines the area of inflammation in the tooth. Then he injects an anesthetic to make the procedure painless. The specialist thoroughly cleans the root canals and removes affected tissue to prevent re-inflammation. If necessary, he applies arsenic-free medicine under a temporary filling, and then replaces it with a permanent one and takes a control photograph. Most often, tooth nerve removal takes place in one session, with a permanent filling immediately installed. It is impossible to carry out treatment without complete removal of the pulp (in adults), since its damage is an irreversible process.
Why does a tooth hurt under a crown and what to do about it?
In addition, the harmful effects on the tooth are enhanced when using low-quality instruments: dull burs, poorly centered tips, insufficient water cooling which leads to nerve burns, overheating of the tooth during polymerization of the adhesive, etc.
Another equally common cause of tooth sensitivity is medical errors and violations of the technology of tooth preparation and fixation of restorations. For example, excessively deep tooth preparation, when the doctor grinds off more dental tissue than necessary, coming too close to the dental nerve. In this case, traumatization of the nerve occurs, to which the tooth responds not with short-term, quickly passing sensitivity, but with long-term aching, severe pain - pulpitis.
If you experience pain under a crown or veneer of this nature, this means inflammation of the dental nerve. The only salvation in such a situation will be depulpation of the tooth, and it would be good if this does not require removing and redoing the restoration, but it will be possible to get through it.
Another trouble that can lead to pain in a living tooth under a crown or veneer is caries that was not completely cleaned out during tooth preparation and continued its victorious march after fixing the structure.
Another example of medical error is damage to the gums either with a bur during tooth preparation, or with a retraction thread placed in the gingival sulcus to obtain a clear preparation boundary.
Since such injuries heal quite quickly in the oral cavity, they cause inconvenience for a fairly short time, although sometimes they require treatment.
Another thing is chronic gum injury caused by improperly made crowns or veneers.
This refers to either the edge of the restoration going too deep under the gum, or the edge being too thick, overhanging the margin of the preparation.
In both cases, compression of the gums by ceramics occurs, which means impaired blood circulation in this area, chronic inflammation of the gums - gingivitis and periodontitis - with all the ensuing consequences: cyanosis, bleeding, etc.
Another problem that causes pain in a tooth under a crown or veneer is tooth mobility that appears after the structure is fixed.
As a rule, this is also a consequence of an error, which consists in overestimating the bite, which leads to overload of the tissues that hold the tooth in the bone - the periodontium and periodontal tissue. As a result, the tooth becomes mobile and becomes painful when biting and chewing food, and sometimes even when simply closing the mouth.
Another danger of overbite is the so-called “aseptic periodontitis”. The essence of this phenomenon is that overloading a tooth does not cause its mobility, but the death of the nerve and the transition of the pathological process to the bone, in which a focus of inflammation is formed - cystogranuloma, and then a cyst.
And since the cause is not infection, but overload, this process is called aseptic.
It must be said that this kind of mobility and development of cysts can occur both in living teeth and in pulpless ones, even very carefully treated and with perfectly sealed canals.
Well, now let's talk about pulpless teeth.
In addition to the problems common to living teeth, they have their own characteristics.
First of all, we must talk about errors associated with poor diagnostics.
Very often, it is impossible to see a cystogranuloma or dental cyst on simple dental or panoramic photographs. This leads to the fact that the doctor makes decisions about making a crown or veneer without having all the necessary information about the condition of the tooth and surrounding tissues.
This means that a restoration can be made for a tooth that is already involved in a pathological process, which simply has not yet manifested itself properly.
Under the influence of medical manipulations and the changed load on the tooth, periodontitis begins to progress, pain appears and, as a rule, such a tooth is removed.
That is why we pay such serious attention to the diagnosis of dental diseases and always use the most modern type of dental diagnostics - computed tomography - during the initial examination of the patient.
Another common cause of pain in a pulpless tooth under the crown is a crack in the root of the tooth or a chipping of any of the walls of the crown part, that is, mechanical damage to the tooth.
If a root crack most often occurs in pulpless teeth restored with root pins or stump pin inlays, then wall spalling occurs in teeth without pins, with thin walls and large fillings. When the wall breaks off, the broken part seems to “hang” on the gum, causing pain with each vibration.
With a root crack, the pain sensations are similar to those with periodontitis.
How long does a tooth hurt after nerve removal?
As already mentioned, the depulpation procedure is performed using local anesthesia, so pain directly during nerve removal is excluded. However, after the anesthetic wears off, the patient may feel discomfort at the treatment site.
After removal of the nerve, it is possible to use painkillers, but before using them you must consult with your dentist. This will help reduce pain if it causes severe discomfort. It is also recommended that during the healing period, stick to soft foods in the diet that will not create additional stress when chewing food. Another way to reduce pain can be preventive rinses and oral baths.
To accurately answer the question of how long a tooth hurts after nerve removal, you need to understand that these are all individual characteristics of each patient. However, on average the healing process takes 2-3 days. Do not self-medicate or ignore pain. If the pain does not go away at the end of this period, this is a reason to consult a dentist.