Inflammation of the female external genitalia, manifested by itching, burning, copious discharge, swelling and redness of the genitals, pain after urination. The inflammatory process will not go away on its own if its cause is not eliminated. When the first symptoms of vulvitis appear, come to the Alfa Health Center clinic in Moscow. Our gynecologists will diagnose and prescribe adequate therapy.
What are the main signs of vulvitis in women and treatment methods - we will consider in detail in this article.
Etiology of vulvitis
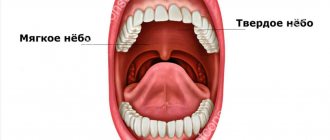
The vulva is a thin and sensitive epithelial lining of the labia majora. Folds of tissue surround the clitoris and extend to the hymen. On the surface of the membrane there is a healthy vaginal microflora, a natural acidic environment is formed, which provides local immunity. Infectious agents, once on the mucous membrane, die under the influence of acids or are inhibited by lactobacilli.
In childhood, the environment of the epithelial membrane is closer to the alkaline spectrum. There are no lactobacilli in girls yet. There is also no hormonal protection against infections, since estrogen production is still at a minimum level. During this period, the genitals are vulnerable to pathogenic microbes. The infection does not encounter natural barriers on its way and actively develops on the mucous membranes, moving further and further.
The risk of inflammation also increases during menopause. The female body produces less estrogen during menopause. The secretion of the internal genital organs decreases, the mucous membranes become dry, and part of the beneficial microflora dies. If an infectious agent enters, acute vulvitis can quickly develop with further transition to a chronic form.
general characteristics
Pain in the labia area is most often observed in acute and chronic specific and nonspecific infectious diseases. Other possible causes are degenerative and atrophic changes, allergic reactions. With local inflammatory processes, there is a danger of upward spread of infection with damage to the vagina, cervix and body of the uterus, ovaries and fallopian tubes. Exogenous factors contributing to the development of this group of pathologies are:
- neglect of hygiene;
- mechanical injuries to the labia during sexual intercourse, using pads for too long, wearing rough and tight clothing;
- chemical irritation and skin damage due to the use of inappropriate hygiene products or attempts at self-medication;
- abuse of antibiotics, irrational use of hormonal contraceptives, radiation therapy.
Endogenous disorders that create favorable conditions for the occurrence of inflammatory and atrophic processes in this area include:
- metabolic and hormonal disorders: decreased estrogen levels, diabetes, obesity, deficiency of vitamins and minerals;
- urethro-vaginal, vesicovaginal and rectovaginal fistulas;
- skin diseases: psoriasis, perineal eczema;
- helminthic infestations, intestinal dysbiosis.
Forms and causes of vulvitis
Inflammation occurs both in adulthood and in girls under 10 years of age against the background of frequent acute respiratory viral infections, reduced immunity, pinworm infection and antibiotic use. At risk are pregnant girls, women with menopausal syndrome, whose mucous membranes become thinner due to decreased estrogen production. Symptoms of vulvitis appear from infection with pathogenic microorganisms (Trichomonas, chlamydia) or from an increase in one’s own opportunistic flora (fungi, herpes viruses, E. coli).
There are vulvitis:
- primary – an independent disease;
- secondary – a consequence of other diseases.
The main causes of primary vulvitis:
- genital injuries;
- intestinal dysbiosis;
- tight, synthetic underwear;
- using sanitary pads without changing for a long time;
- insufficient personal hygiene.
Secondary vulvitis occurs against the background of:
- infections, inflammations of the genitourinary system – colpitis, vaginitis, cervicitis and others;
- changes in the vaginal microflora due to long-term self-medication with antibiotics;
- disruptions in the functioning of the endocrine system (diabetes mellitus, adrenal gland diseases);
- infection with worms and other parasites (symptoms worsen at night when roundworms or pinworms emerge from the anus);
- vitamin deficiency;
- immunodeficiency.
Depending on the main provoking factor, several forms of the disease are distinguished:
- Bacterial vulvitis. The cause of inflammation is opportunistic microorganisms or infections. There is a distinction between nonspecific vulvitis, caused by an imbalance of microflora, and a specific form, which develops when infected with an infection from a sexual partner. Among the most aggressive pathogens are gonococci, chlamydia, trichomonas;
- Allergic vulvitis. Inflammation is caused by contact with an allergen, for example, when particles of washing powder are not completely rinsed out of the laundry, or a gel with fragrances is used for intimate hygiene;
- Candidiasis (fungal) vulvitis. The causative agent of the disease is fungi of the genus Candida. Candidiasis vulvitis more often than others becomes chronic. An exacerbation can be triggered by any factors: from stress to a cold. Candidiasis (fungal vulvitis) is also classified as nonspecific inflammation;
- Atrophic vulvitis. The disease develops during natural changes in the tissues of the internal genital organs during menopause. Atrophic processes can begin after removal of the ovaries.
Vulvitis occurs acutely and chronically. In the acute form, the symptoms of the disease appear suddenly and quickly intensify, increasing over 2-3 days. During this period, it is important to consult a doctor, undergo a diagnosis of vulvitis and receive quality treatment. The risk of relapse will be minimal.
If acute vulvitis is treated incorrectly or if the doctor’s recommendations are not followed, the inflammation will become chronic. Symptoms will subside and reappear, reducing quality of life. Even a young girl can become a regular gynecology patient if she ignores the signs of the disease.
There is also subacute vulvitis - a transitional form of inflammation.
Why do the labia become inflamed?
1. Sexual infections, STDs, dysbacteriosis.
2. Cyst of the vulva, vagina and/or labia.
3. Ingrown hairs as a result of shaving or depilation.
4. Yeast infection. Typical symptoms of thrush include vaginal discharge, irritation, inflammation, redness and tenderness. You will also experience severe itching at the entrance and inside the vagina, pain during sexual intercourse, and burning when urinating.
5. Genital warts. Pimples on the labia, like “bumps” on the vagina, can be condylomas. Formed as a result of infection caused by the human papillomavirus (HPV). It is the most common sexually transmitted disease (STD); They may also appear on the cervix, clitoris, urethra, or inside or outside the anus. Genital warts look like growths or tubercles, are usually painless, and flesh-colored. They may be accompanied by itching, discharge, and burning.
Condylomas are removed by surgical procedures, including and combining options:
- Removal by radio wave method,
- Electrocoagulation or “burning”
- Cryodestruction or “freezing”,
- Laser therapy,
- Cutting off warts
- Interferon injections.
Untreated condylomas can lead to serious complications. The HPV that causes them is the leading cause of cervical cancer and can also cause vulvar cancer.
6. Genital herpes (HSV type 2). The labia become itchy and swollen due to a herpetic infection. It can be transmitted sexually. Painful red bumps or blisters appear, which can be localized on the genitals and nearby areas. In women, herpes rashes appear near the vagina, on the vulva, hymen, and the mucous membrane of the labia minora and labia majora.
7. Lichen sclerosus of the vulva. This is a rare skin condition that mainly affects women after menopause. It often appears on the vulva and around the anus as bumps or blisters. Having this condition poses a slightly higher risk of developing vulvar cancer. Common symptoms of lichen sclerosus include:
- Blisters that may be filled with blood
- White spots that look like wrinkled patches of skin
- Fragile, thin, shiny skin,
- Bruising and bleeding
- Pain during sexual intercourse or during urination.
8. The tumor process may begin with swelling and inflammation of the genital organs and the formation of small “warts” on the labia minora. The tumor can be in the form of a dense formation of small size. In the future, painful ulcers with rounded edges, filled with purulent or bloody contents, may appear on the labia. The lip may become large and have an unpleasant odor. In this situation, it is necessary to urgently contact a gynecologist for advice and to conduct a series of diagnostic tests. Inflammation of the labia in women and cancer of the external genitalia are very similar in their clinical picture. And it is sometimes possible to keep the fine line between these diseases only after the results of a biopsy. However, cancer of the external genitalia is rare and usually occurs in older patients.
9. Uncomfortable underwear. Due to the synthetic material of the panties, the skin in the intimate area does not breathe and begins to sweat, as a result the skin becomes dry, which subsequently leads to itching of the labia, they swell and begin to itch.
10. Long-term wearing of pads. If you wear pads for a long time and forget to change them, this causes irritation of the labia minora and itching and internal burning appear in the vagina and clitoris area.
11. Vulvitis. If the labia are swollen, but in addition there is painful urination and unpleasant, foul-smelling greenish-yellow discharge, and the skin itches, this may indicate inflammation of the external genitalia.
Vulvovaginitis can also develop as a result of active, rough, skin-damaging masturbation. This mainly occurs in teenagers, as well as girls who practice some forms of extreme sex, for example, BDSM. Wearing dirty panties and failure to follow basic rules of intimate hygiene also contribute to infection.
SWELLING LABIA IS NORMAL, NO TREATMENT IS NEEDED!
IMPORTANT NUANCE: Nature initially dictates that women’s labia minora swell during sexual fantasies, direct mechanical stimulation of a woman’s reproductive external genitalia, or in the case of direct sexual contact - and this is absolutely normal. After the end of sexual intercourse or the cessation of sexual stimulation, arousal gradually subsides and the genitals return to their original size. This natural physiological process usually takes an hour or two after peak arousal, sometimes such regression drags on for four to twelve hours. Moreover, it has been noted that if after sex the labia are swollen and the woman does not have an orgasm, the outflow of blood is much slower, which can ultimately contribute to the development of a number of gynecological problems.
Also, the blood supply to the reproductive organs changes cyclically, depending on the phase of the menstrual cycle.
ANALYSIS AND DIAGNOSTICS
Inflammation in the intimate area in women, especially in the presence of purulent or other unpleasant vaginal discharge, requires an immediate visit to a gynecologist for a comprehensive diagnosis. First of all, you need to take tests to find out the reasons why the labia are itching, skin folds are swollen, and discomfort has appeared in this delicate area. The necessary examination in this case will be the following.
Minimum: Gynecological examination, smear for flora, PCR analysis for “hidden” infections, tank culture for flora, general urine test.
According to indications: Colposcopy, oncocytology of the cervix, blood tests (hormones, allergens, biochemical, general analysis), ultrasound of the pelvic organs.
Inflammation of the gland on the labia
Painful inflammation in the labia (on one or both sides) can cause bartholinitis, inflammation of the large gland of the vestibule of the vagina. It is a paired organ and is located deep in the subcutaneous tissue at the base of the labia majora. Its main function is to produce a viscous mucous secretion and moisturize the intimate area during sexual intercourse. The inflammatory process in the gland of the labia is most often caused by gonococci, staphylococci, less often by streptococci, E. coli, Trichomonas and other microorganisms that penetrate the excretory duct of the gland from the vagina or urethra. Risk factors also lie in non-compliance with the rules of intimate hygiene, weakening of the body, impaired microflora and weakened immunity.
Symptoms of vulvitis in women
During the acute phase of inflammation the following are observed:
- swelling and redness of the external genitalia;
- itching, burning;
- painful sensations when urinating, walking, sexual intercourse;
- mucous plaque mixed with pus;
- enlarged inguinal lymph nodes;
- temperature increase;
- general weakness, fatigue.
Signs of vulvitis in chronic form are the same symptoms, but in a less pronounced form. As the pathology develops, ulcers of the mucous membrane and scars appear that deform the surface.
Swelling of the penis and testicles.
Swelling of the genital organs can be caused by both completely harmless factors (passionate sex, tight underwear, allergies, poor hygiene) and serious reasons. Therefore, if the swelling does not subside within a day or additional symptoms appear (itching, burning, redness, discharge, rash, inability to open the foreskin), you should consult a specialist.
Why does the penis and/or testicles swell?
Various reasons can cause swelling of the penis and testicles:
Balanitis, posthitis, balanoposthitis.
Balanitis (inflammatory disease of the head of the penis) and posthitis (inflammatory process of the foreskin) are usually inseparable, which is why they are combined under the common term “balanoposthitis.” In a man, erosions form on the head of the penis and in the area of the foreskin, pain, swelling, and hardening of the inguinal lymph nodes are possible.
Cavernite.
Pathological processes in the cavernous bodies cause swelling of the shaft of the penis.
Phimosis.
Due to the narrowing of the foreskin, the head of the penis is not fully released, which leads to inflammation and swelling.
Paraphimosis.
Pinching the head of the penis by the foreskin causes redness and swelling of the organ, and pain when urinating. In the absence of timely medical care, tissue necrosis is possible.
Thrombophlebitis.
As a result of inflammation of the dorsal vein, the penis swells and the temperature rises sharply. Physical activity and movement cause pain.
Allergy.
Itching and swelling of the penis can be caused by synthetic underwear, poor-quality lubricants, condoms, and long-term use of antibiotics.
Microtraumas.
The slightest bruise can provoke swelling of the penis and the appearance of a hematoma, which is explained by the increased sensitivity of the organ. Sometimes the cause of microtrauma can be a strong impact on the penis during sexual intercourse or masturbation, or wearing too tight underwear.
Infections.
Sexually transmitted diseases (trichomoniasis, chlamydia, gonorrhea, syphilis) often cause swelling of the genital organs. With syphilis, a growing compaction also becomes noticeable, and the general condition worsens. Swelling of the penis is also possible with systemic infections (tuberculosis).
Tumor.
The cause of swelling can be a malignant neoplasm, but swelling of the entire trunk is extremely rare.
How to treat vulvitis in women
The gynecologist will answer this question after making a diagnosis. The pathology is detected during a gynecological examination, the cause is determined after additional examinations.
Treatment for vulvitis includes:
- Intravaginal irrigations and baths to alleviate the patient’s condition;
- Drug therapy - antibacterial, hormonal, homeopathic, immunostimulating, antifungal, anthelmintic drugs, depending on the causes of the disease. Medicines are prescribed in the form of tablets, ointments, suppositories;
- A diet excluding sweet, salty, spicy and alcohol.
Vulvitis during menopause requires careful selection of hormonal medications. It is necessary to compensate for the deficiency of estrogen in the body with pills in order to relieve a woman of vaginal dryness and other unpleasant symptoms.
In some cases, gynecologists decide how to treat vulvitis, together with an infectious disease specialist, nephrologist, urologist and other doctors of related specialties.
Expert opinion
Often women hesitate to visit a doctor and try to cope with vulvitis on their own. They find folk remedies on the Internet or learn from friends, buy and take medications on their own. You can suppress the symptoms, but you cannot completely cure the inflammation. An integrated approach is needed.
Moreover, taking pills for vulvitis without a doctor’s prescription can complicate the course of the disease. Pathogenic microflora becomes resistant to drugs. It is extremely difficult to treat such patients in the future. If to this is added a burn to the mucous membrane, an allergy, or other “surprises” from folk remedies, then a whole consultation has to be involved in drawing up a treatment regimen.
There is no need to be embarrassed by the symptoms and waste time. The doctor will help you get rid of the disease in just a few days if you start treatment at an early stage.
Complications of vulvitis
Treatment of vulvitis in girls and women must be supervised by an experienced doctor. There is a mistaken ease in relation to the disease, which will go into the chronic stage after 7-10 days. Chronic vulvitis is characterized by disturbing symptoms and constant relapses of exacerbations. Inflammation is also dangerous for girls. It is fraught with deformation of the external genital organs, anorgasmia, infertility and miscarriages if the process spreads to the vagina, uterus, and ovaries.
As inflammation develops, purulent processes occur. The woman cannot have a full sex life, experiences pain, and has a high fever. Ulcers appear on the mucous membranes. Purulent vulvitis threatens sepsis. This is a serious complication with a high risk of death.
Vulvitis during pregnancy is no less dangerous. Ascending inflammation spreads to internal organs: uterus, ovaries. There is a risk of intrauterine infection of the fetus, spontaneous abortion, perinatal or neonatal death.
If you go to the clinic in a timely manner, vulvitis responds well to treatment.