How does an infection in a tooth cause the lining of the maxillary sinus to thicken?
The apices of the roots of the teeth are located under the Schneiderian membrane, that is, under the mucous membrane that lines the bottom of the maxillary sinus.
This is the normal anatomical structure of the sinus - when the tops of the teeth are located in it. Some people have the tops of the fourth, fifth, sixth, seventh there. Some people only have the sixth. Some have sixth and fifth. But, one way or another, they are almost always there.
When a tooth is affected by caries, the infection penetrates through the dentinal tubules into the pulp chamber. Through it, the infection slowly progresses further through the blood and lymphatic vessels into the periodontium of the tooth.
Pulp microvessels emerge from the periodontium directly under the mucous membrane of the sinus, and over time it begins to react with inflammation.
Immune system cells responsible for protecting against infection initiate chronic inflammation. And the mucous membrane gradually thickens. This irritation happens all the time.
Infection from the carious process, which is thus restrained by immunocytes, causes a gradual degeneration of the structure of the sinus lining in the form of polyps and cysts.
Causes of sinusitis
Predisposing factors to the occurrence of sinusitis are:
- deviated nasal septum;
- existing foci of chronic infection in the oral cavity or nasopharynx (chronic rhinitis, pharyngitis, tonsillitis);
- allergic reactions in the body;
- proliferation of polyps, adenoids;
- weakened immunity;
- long-term course of colds, flu, ARVI;
- uncontrolled use of vasoconstrictor nasal drops;
- insufficient oral hygiene, lack of dental sanitation;
- traumatic injury to the nose, paranasal area or cavity walls.
Can a dentist diagnose sinusitis?
In case of pulpitis, the patient finally comes to the dentist. The doctor fills the canals, removes the nerve, but part of the infection still remains in the apical delta - after all, it has penetrated there a long time ago!
The apical delta is a branching at the tips of the roots that can never be adequately sterilized. And if a tooth has many roots, then, naturally, the entire system of root canals is one, like the root of one tree.
Therefore, if an infection gets into a tooth, it is already inside.
And it’s normal that the body fights it, and the sinus mucosa begins to thicken. In the process, some people develop granulomas, others - cysts. But cysts are changes in the periodontium, and the mucous membrane itself begins to thicken and degenerate.
Sometimes it happens that polyps are formed - spherical thickenings on a stalk. Hypertrophy of the columnar epithelium may occur. That is, as a result of chronic inflammation, many, many layers are formed.
The dentist can conduct a computed tomography scan, but it can only identify changes in the mucous membrane in volume - simply establish the presence of this fact.
And only an otolaryngologist can say what exactly happened there. To do this, you need to conduct an endoscopic examination.
But in most cases, it is the dentist who is the first doctor to detect sinusitis on a CT scan.
When a person realizes from various symptoms that he has inflammation in the sinus, he also learns about this from the dentist.
How to avoid such situations?
Firstly, before treating the teeth of the upper jaw, the dentist may recommend doing a 3D diagnosis or computed tomography of the paranasal sinuses and upper jaw.
And then repeat this study after completing the course of treatment. These studies help the dentist to carry out treatment correctly and minimize the risks of complications. If filling material does get into the sinus, it should, of course, be removed.
Doctors at the Lor Plus clinic have a diverse arsenal of treatments for sinusitis and sinusitis, including odontogenic ones. For timely diagnosis and effective treatment, we use traditional methods and, of course, the most modern technologies, including endoscopic ones.
Also about the methods of treating sinusitis at the Lor Plus clinic, see here.
Read also: Questions and answers on the topic - Treatment of nasal diseases
Sinusitis or tooth – what to treat first?
In this case, many otolaryngologists prescribe tooth extraction.
In our clinic, we collaborate with specialists who treat odontogenic sinusitis or help the patient prepare the sinus mucosa for sinus lifting.
Of course, it is not always possible to prosthetize and treat a tooth with a source of infection in the periodontium in the upper jaw. Therefore, such teeth often still need to be removed.
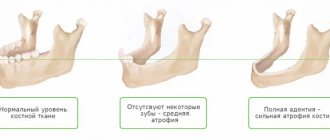
Tooth extraction surgery is a major source of irritation for the body and the immune system. After it, you need to wait 4-6 months until the porous bone tissue of the alveoli is restored.
In this case, conservative anti-inflammatory therapy, antibiotics, and active copious rinsing of the nasal sinuses are prescribed. Treatment lasts about a month after tooth extraction.
If CT and diagnostics revealed a source of infection (cyst or granuloma) on the tooth, then treatment for odontogenic chronic sinusitis begins immediately after removal. Then the chance to reduce inflammatory changes in the mucosa is quite high.
Otherwise, the patient risks getting large growths, which sometimes occupy more than half the height of the sinus.
This is manifested by nasal congestion, because when we have ARVI, the nasal mucosa swells greatly. And our nasal mucosa is exactly the same as in the sinus: the same columnar epithelium. It swells very much when initially, as a result of constant irritation, the infection has already grown by more than half.
In this case, the half of the nose that is more blocked will be an indicator to check what is wrong with the teeth on the same half of the jaw.
Be sure to treat!
What happens if sinusitis is not treated?
Eduard, Rostov
– If acute sinusitis is not treated, it can become chronic, and also cause complications - in the eye socket (as a result of which you can even lose an eye), in the brain (which is fraught with the development of a brain abscess, meningitis). There are (fortunately, rarely) fulminant forms of sinusitis, which develop from several hours to a week and can result in the death of the patient. This happens especially often in people with diabetes, who have high glucose levels in their tissues and are a good breeding ground for microorganisms. So, if you get sinusitis, try to treat it properly.
Implant into a modified sinus - is it possible?
Some time after tooth extraction, the patient may decide to install an implant. If sinus treatment was not carried out in a timely manner after tooth extraction, it remains to treat sinusitis before sinus lift surgery and implant installation.
It is advisable to do this together with an otolaryngologist.
But at the same time, the patient must understand that during a sinus lift, the altered sinus may rupture because it has an altered structure. And if this does happen, the sinus lift may not take place. Therefore, odontogenic sinusitis still needs to be treated during tooth extraction. And prepare the sinus together with the otolaryngologist.
Symptoms of odontogenic sinusitis
Most often patients complain of:
- moderate pain in the cheek or infraorbital region (sometimes the entire half of the face hurts);
- nasal congestion on one side only, feeling of heaviness;
- discharge of pus from the corresponding half of the nose;
- pain when biting on an incorrectly treated tooth;
- dysfunction of the sense of smell;
- feeling unwell – headache, fever, sleep disturbance, chills;
- With an exacerbation of the disease, enlargement of the lymph nodes on the corresponding side is possible.
Systemic antibacterial therapy for odontogenic maxillary sinusitis at the present stage
A significant role in the occurrence of chronic inflammation in the maxillary sinus belongs to diseases of the teeth of the upper jaw. Odontogenic sinusitis (OG), in fact, is a complication that arises as a result of the spread of a pathological process from the periapical focus of chronic infection in the area of premolars or molars of the upper jaw (periodontitis, periostitis, osteomyelitis, suppurating radicular cysts, there are also indications of the possibility of sinusitis occurring with abscessive form of periodontitis). Patients with odontogenic sinusitis are admitted for treatment to both dental and otorhinolaryngological hospitals. According to dentists, odontogenic sinusitis is found in 12–50% of patients with chronic sinusitis. According to the observations of otorhinolaryngologists, the frequency of odontogenic sinusitis ranges on average from 2 to 25%, with its open (perforated) form being 41.2–77.2%. Such contradictory data are not due to the true ratio of odontogenic and rhinogenic sinusitis, but to the specifics of examining patients in hospitals of various profiles. Diagnosis of odontogenic sinusitis is difficult and requires synergy in the work of otorhinolaryngological and dental services. Diseases of the teeth of the upper jaw, which are practically asymptomatic, are, as a rule, not regarded as a cause of sinusitis. Unfortunately, dentists and otorhinolaryngologists often underestimate the cause-and-effect relationship between the pathology of the maxillary sinus and diseases and abnormalities in dental development, which leads to diagnostic errors and a recurrent course of the disease. Treatment of odontogenic sinusitis should be comprehensive and in all cases include sanitation of the source of infection. The difficulty of conservative treatment of odontogenic sinusitis lies in the fact that the inflammatory process in the maxillary sinus, which developed as a result of prolonged periapical inflammation of the teeth of the upper jaw, takes on a primarily chronic nature and in most cases requires surgical treatment, the extent of which depends on both the endoscopic picture and the functional state mucous membrane. Conservative treatment is effective only for the exudative form of inflammation. Antibacterial therapy for odontogenic maxillary sinusitis is empirical in nature and is based on data on the main pathogens and their sensitivity to antimicrobial drugs in the region. It also takes into account the fact that due to the high prevalence of microbial associations, the risk of occurrence of b-lactomase-producing strains significantly increases. In this regard, antibiotic therapy for odontogenic sinusitis comes down to a choice between protected penicillins and respiratory fluoroquinolones. The purpose of our study was to study the possibilities of increasing the effectiveness of treatment of odontogenic sinusitis. Over the past year, we observed 32 patients suffering from odontogenic sinusitis and who were undergoing inpatient treatment in the ENT department of the Moscow Clinical Hospital named after. S.P. Botkin - 13 men and 19 women (average age - 38 years). The diagnosis of odontogenic sinusitis was established on the basis of complaints, medical history, objective examination (sinusoscopy, endoscopic examination of the nasal cavity, oroscopy), and the results of X-ray examination (radiography, panoramic zonography and CT scan of the paranasal sinuses). All patients were consulted by a dentist. All patients had mild to moderate severity of the disease. The “causal” teeth were: 1st molar – 19 patients, 2nd molar – 9 patients, 2nd premolar – 4 patients. In one case, there was a combination of pathology of the second premolar and first molar (Table 1). Among the examined, 4 people had an open (perforated) form of odontogenic sinusitis: 3 – antroalveolar communication with the maxillary sinus due to the removal of the first molar, 1 – second molar (Fig. 1). The group with a closed form of odontogenic sinusitis consisted of 28 people, and in four cases the process was associated with the presence of filling material in the maxillary sinus. The exudative form was registered in 9 patients (Fig. 2). According to the results of the examination, surgical treatment was recommended for 19 patients with a closed form of odontogenic sinusitis, 14 of them refused the proposed operation. As a result of bacteriological studies, associations of anaerobes and aerobes were found in 17 patients with odontogenic sinusitis in the punctate of the maxillary sinus. Isolated cultures of aerobes and anaerobes were obtained in 3 and 7 cases, respectively. No flora growth was obtained in 5 studies (Fig. 3). Aerobic flora was represented by Streptococcus spp., Staphylococcus aureus, Haemophilus influenzae, Pseudomonas aeruginosa. Anaerobic – gram-positive cocci (Streptococcus spp.), Veillonella spp., Prevotella spp., Peptostreptococcus spp., Fusobacterium spp. (Table 2). Conservative treatment included antibacterial therapy with protected penicillins, puncture (washing) of the maxillary sinus with the introduction of saline, and local use of decongestants. All patients were consulted by a dentist; sanitation of the odontogenic source of infection was carried out on days 3–4 after the start of conservative therapy. In our work, we compared the effectiveness of systemic antibacterial therapy for odontogenic sinusitis with amoxicillin/sulbactam, which recently appeared on the Russian market, and amoxicillin/clavulanate, which has long been used in ENT practice. Both drugs belong to the group of protected penicillins. Trifamox IBL® (amoxicillin/sulbactam) is an antimicrobial agent from the penicillin group (registered in the fall of 2005 in Russia (Trifamox IBL®, Laboratorios Bago S.A., Argentina)), has a wide spectrum of bactericidal action against aerobic gram-positive bacteria (including strains producing b-lactamases): Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus saprophyticus, Streptococcus pyogenes, Streptococcus anthracis, Streptococcus pneumoniae, Streptococcus viridans, Enterococcus faecalis, Corynebacterium spp., Listeria monocytogenes; anaerobic gram-positive bacteria: Clostridium spp., Peptococcus spp., Peptostreptococcus spp.; aerobic gram-negative bacteria (including strains producing b-lactamases): Escherichia coli, Proteus mirabilis, Proteus vulgaris, Klebsiella spp., Salmonella spp., Shigella spp., Bordetella pertussis, Yersinia enterocolitica, Gardnerella vaginalis, Neisseria meningitidis, Neisseria gonorrhoeae, Moraxella catarrhalis, Haemophilus influenzae, Haemophilus ducreyi, Yersinia multocida, Campylobacter jejuni, Acinetobacter spp.; anaerobic gram-negative bacteria (including strains producing b-lactamases): Bacteroides spp., including Bacteroides fragilis. Amoxicillin acts bactericidal by inhibiting the synthesis of the bacterial wall. Sulbactam is a stable, irreversible inhibitor of b-lactamases secreted by microorganisms resistant to b-lactam antibiotics. Sulbactam expands the spectrum of activity of the drug against resistant strains, without changing the activity of amoxicillin against sensitive strains, forming complexes with penicillin-binding proteins of bacteria, and exhibits synergy when used simultaneously with b-lactam antibiotics. Sulbactam does not have its own clinically significant antibacterial activity (with the exception of Neisseriaceae and Acinetobacter). The drug is available in both tablet and injection forms, which is very convenient when carrying out step-by-step therapy. When taken orally, the drug has a large volume of distribution and reaches high concentrations in tissues and body fluids, especially in the mucous membrane of the upper respiratory tract. In terms of the rate of development of the bactericidal effect, amoxicillin/sulbactam is significantly ahead of other antibacterial drugs, since it has significantly greater resistance to changes in the pH of the solution than clavulanate or tazobactam, and from a practical point of view, this means that in the conditions of a real infectious process occurring with Due to significant variations in the acidity of the environment, sulbactam is able to penetrate tissue more actively than other b-lactamase inhibitors. In our work, patients who received only conservative treatment, depending on the antibiotic therapy performed, were divided into 2 groups (main and control), similar in gender, age and the nature of the process in the maxillary sinuses and dentofacial area. The main group included patients receiving amoxicillin/sulbactam; in the control group, antibacterial therapy was carried out with amoxicillin/clavulanate (Table 3). All patients received an antibiotic in comparable dosages to amoxicillin (500 mg x 3 times a day per os). Based on the results of the conservative treatment, a pronounced positive dynamics of the main clinical symptoms of the disease was noted by the 7th day in both groups of patients with the exudative form of odontogenic sinusitis (Fig. 4, 5). In patients with purulent polyposis lesions of the maxillary sinus who received amoxicillin/sulbactam, remission was achieved on the 8th day, and in the control group on the 9th. Antimicrobial effectiveness and high sensitivity of microorganisms to drugs are confirmed by data from microbiological studies over time. Thus, amoxicillin/sulbactam is not inferior to traditional protected penicillins, the clinical effectiveness of which has been tested by time, and also has a number of advantages: 1. Sulbactam is more resistant to changes in pH, due to which it is able to more actively penetrate into inflamed tissues. 2. Sulbactam's high tolerance to pH fluctuations allows it to be administered intramuscularly. 3. Sulbactam is more resistant to most plasmid and chromosomal type I b-lactamases. 4. Amoxicillin/sulbactam is more convenient for sequential therapy, since, in addition to oral administration, it has a form for intramuscular and intravenous administration. In conclusion, it should be noted that amoxicillin/sulbactam is an effective drug in the treatment of odontogenic sinusitis and can be recommended as initial therapy for chronic maxillary sinusitis. The optimal choice of antibacterial agents for the treatment of odontogenic processes in the maxillary sinus reduces the treatment time.
Literature 1. Anyutin R.G., Luzina V.V., Romanov I.A. Differentiated surgical treatment of odontogenic sinusitis: Mater, III Congress of the Dental Association (all-Russian) - M., 1996. 2. Pluzhnikov M.S. Conservative and surgical methods in rhinology – St.–Pb., 2005 3. Timofeev A.A. Guide to maxillofacial surgery and surgical dentistry - K., 2004. 4. Sidorenko S.V., Yakovlev S.V. Beta-lactam antibiotics. Russian Medical Journal, 1997; 5 (21): 1367–81. 5. Yakovlev S.V. Amoxicillin/sulbactam – new opportunities to overcome antibiotic resistance. Russian Medical Journal 2005, volume 13, no. 21, p. 1418–22 6. Ambler PR. The structure of beta-lactamases. Philos Trans R Soc Lond Ser B 1980;289:321–31. 7. Bush K, Jacoby GA, Medeiros AA. A functional classification scheme for beta–lactamases and its correlation with molecular structure. Antimicrob Agents Chemother 1995;39:1211–33. 8. Pensotti C. et al. Meta-analisis sobre la actividad in vitro e in vivo. Efficacia y tolerancia de la combinación amoxicillina, sulbactam en humanos. La Prensa Medica Argentina 1998;85(4):515–22.