In dental treatment, almost no manipulation is complete without pain relief.
At the moment, there are many types and subtypes of anesthesia, which differ in drugs, methods of administration and areas of use.
Anesthesia in dentistry is torusal – this is anesthesia that is performed on the lower jaw to block nerve fibers. In this case, the anesthesia itself is placed in the area of the torus - the ridge on the lower jaw, hence its name. Due to this, you can numb the teeth in the lower jaw with a small amount of the drug.
Indications for torusal anesthesia
Indications for this method of local anesthesia are:
- Treatment of teeth on the lower jaw
- Splinting the lower jaw after trauma
- Extractions on the lower jaw
- Treatment of pericoronitis
- Cleansing purulent foci
- Removal of tumors
- Surgeries in the area of TMJ
Contraindications include all the usual contraindications for local anesthesia - allergies, some mental and systemic diseases, as well as the psychological state of the patient - if you are very afraid of injections, then perhaps you should choose a different type of pain relief during treatment.
Intraoral methods of mandibular anesthesia
Anesthesia is carried out by palpating bony anatomical landmarks and using the apodactyl method (without palpation). Mandibular anesthesia by palpation.
To carry it out, it is necessary to palpate to determine the location of the retromolar fossa and the temporal ridge, which is a guide for inserting the needle. From the coronoid process to the lingual side of the alveolar process of the lower jaw, a bone ridge descends - the temporal crest (crista temporalis). In the lower section, this ridge is divided into internal and external legs, which limit a small triangular area - the retromolar triangle. Between the anterior edge of the ramus of the lower jaw, which passes downwards into an oblique line (linea obliqua) and the temporal ridge, there is a small triangular depression - the posterior molar fossa (fovea retromolaris). Bony landmarks are palpated with the index finger of the left hand if anesthesia is performed on the right, or with the thumb if it is performed on the left. With the patient's mouth wide open, the anterior edge of the lower jaw branch is felt at the level of the distal edge of the crown of the third molar (if it is absent, immediately behind the second molar). By moving the finger slightly inward, the temporal ridge is identified, the projection of which is mentally transferred to the mucous membrane. The finger is fixed in the retromolar fossa. Having positioned the syringe at the level of the small molars of the opposite side, the needle is inserted medially from the temporal ridge and 0.75-1 cm above the chewing surface of the third major molar. Advance the needle outward and backward. At a depth of 0.5-0.75 cm it reaches the bone. After releasing 0.5-1 cm of anesthetic solution, the lingual nerve, which is located anterior to the inferior alveolar nerve, is turned off. Having advanced the needle another 2 cm, they reach the bone groove (sulcus colli mandibulae), where the lower alveolar nerve is located before it enters the canal of the lower jaw. Here, 2-3 ml of anesthetic is injected to turn off this nerve. The branch of the lower jaw is not located strictly in the sagittal plane, but at a certain angle to it, with its anterior edge lying closer and its posterior edge further from the midline. The severity of the inclination of the branch varies in different patients. Therefore, having inserted the needle to a depth of 0.75 cm to the bone and turning off the lingual nerve, it is not always possible to move it deeper to the mandibular foramen without changing the initial position of the syringe. It often becomes necessary to move the syringe to the level of the central incisors and move the needle posteriorly parallel to the inner surface of the mandibular ramus to a depth of 2 cm towards the mandibular foramen and sulcus colli mandibular
Apodactyl method of mandibular anesthesia.
When performing anesthesia using the apodactylic method, the main landmark is the pterygomandibular fold (plica pterigomandibularis). It is located medially from the temporal ridge and can be wide, narrow, or have a normal (medium) transverse size. With the patient's mouth wide open, the syringe is placed at the level of the small molars or the first large molar of the opposite side. The needle is inserted into the outer slope of the pterygomandibular fold in the middle of the distance between the chewing surfaces of the upper and lower large molars (in their absence, in the middle of the distance between the ridges of the alveolar processes). The needle is advanced outward and posteriorly until it contacts the bone tissue (to a depth of 1.5-2 cm), after which 2-3 ml of anesthetic is injected to turn off the inferior alveolar and lingual nerves. Sometimes, having advanced the needle to a depth of 2 cm, it is not possible to achieve contact with the bone. This may be due to the indicated anatomical features of the mandibular ramus, when its inclination to the sagittal plane is significantly pronounced. In this case, the needle, when immersed in the tissue, moves parallel to the inner surface of the jaw branch, without touching it. Then it is necessary to move the syringe even further in the opposite direction, placing it at the level of the second molar. By changing the angle between the inner surface of the branch and the needle, it is possible to achieve its contact with the bone. If the pterygomandibular fold is wide, the needle is inserted into the middle, if it is narrow, into its medial edge. The pterygomandibular fold is a less reliable landmark than the temporal crest, therefore, with the apodactyl method of anesthesia, it is not always possible to accurately deliver the anesthetic solution to the inferior alveolar nerve.
Types of torus anesthesia in dentistry
There are two main techniques for performing this type of anesthesia:
- According to Vazirani-Akinosi
- According to Go-Gates
The Vazirani-Akinosi technique is used only if all other methods of pain relief have already been tried and have not sufficiently relieved sensitivity.
The advantage of Vazirani-Akinosi is effective pain relief in the case of the presence of more than 3 nerves in the tooth, but the disadvantages include the complex method of implementation.
The Go-Gates method is more common, although it is also not so easy to use.
Extraoral methods of mandibular anesthesia
If it is impossible to block the inferior alveolar nerve using intraoral access, extraoral methods are used. Mandibular anesthesia with access from the submandibular region.
To more accurately perform anesthesia, it is rational to determine the projection of the opening of the lower jaw onto the skin.
It is located in the middle of a line drawn from the upper edge of the tragus of the auricle to the intersection of the anterior edge of the masticatory muscle with the base of the lower jaw. By moving the needle towards the mandibular foramen, you can focus on this point. The needle is inserted in the area of the base of the lower jaw, 1.5 cm anterior to the angle of the lower jaw. The needle is moved up 3.5-4 cm along the inner surface of the branch parallel to its posterior edge. At the same time, contact of the needle with the bone should be maintained. It is more convenient to insert the needle without a syringe and attach it only before injecting the anesthetic. Inject 2 ml of anesthetic solution. By moving the needle up, the lingual nerve is turned off another 1 cm. Subzygomatic method (Bershe-Dubov anesthesia).
The needle is inserted directly under the lower edge of the zygomatic arch, 2 cm anterior to the base of the tragus of the auricle.
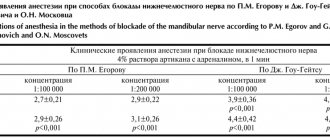
The needle is placed perpendicular to the skin and advanced 3-3.5 cm to the midline strictly horizontally, gradually releasing the anesthetic solution. The needle extends between the heads of the external pterygoid muscle or onto its inner surface, where the inferior alveolar and lingual nerves are located nearby. After administration of 3-5 ml of anesthetic, pain relief occurs within 10-20 minutes. The zone of anesthesia when the lower alveolar and lingual nerves are turned off: all the teeth of the lower jaw of the corresponding half, the bone tissue of the alveolar process and part of the body of the lower jaw, the mucous membrane of the alveolar process on the vestibular and lingual side, the mucous membrane of the sublingual region and the anterior 2/3 of the tongue, skin and mucous membrane of the lower lip, skin of the chin on the side of anesthesia. It should be remembered that the mucous membrane of the alveolar process of the lower jaw from the middle of the second small molar to the middle of the second large molar is innervated not only by branches extending from the lower dental plexus, but also by the buccal nerve. To completely anesthetize this area of the mucous membrane, it is necessary to additionally inject 0.5 ml of anesthetic according to the type of infiltration anesthesia. Anesthesia during mandibular anesthesia most often occurs after 15-20 minutes, its duration is 1-1.5 hours. The severity of anesthesia in the area of the incisors and canines is less due to the anastomoses on the opposite side. Complications of mandibular anesthesia.
When a needle is inserted medial to the pterygomandibular fold, numbness of the pharyngeal tissue and damage to the internal pterygoid muscle are possible, followed by the appearance of contracture of the lower jaw. To eliminate this complication, long-term treatment is sometimes required using physiotherapeutic procedures, mechanotherapy and injections of pyrogenal solution. Damage to blood vessels and the occurrence of hemorrhage are possible, sometimes - the formation of a hematoma, and the entry of the anesthetic into the bloodstream, the appearance of ischemic zones on the skin of the lower lip and chin. When the lingual and inferior alveolar nerves are damaged by a needle, neuritis sometimes develops, for which galvanization and diathermy are used. Occasionally, paresis of facial muscles is observed due to blockade of the branches of the facial nerve. Due to a violation of the technique of mandibular anesthesia, a fracture of the injection needle is possible. This complication can occur when the initial position of the needle changes with a sharp movement, when its central end is deeply immersed in soft tissue or located between muscle and bone. The danger of this complication increases when the needle is inserted into a muscle tendon (usually the temporal muscle). The needle breaks at the point where it enters the cannula. To prevent this complication, you should use high-quality needles, strictly follow the anesthesia technique, do not immerse the needle into the tissue up to the cannula, and do not make rough and sudden movements of the needle. If the broken part of the needle is completely immersed in tissue, there should be no immediate attempt to remove it in the clinic. If indicated (pain spontaneously and when opening the mouth, development of contracture, inflammatory phenomena), removal of the needle is possible only in a hospital after a thorough x-ray examination. This labor-intensive procedure requires good operative technique and surgical experience. Sometimes a broken needle is encapsulated in tissue and does not cause complaints in patients. In these cases, it does not need to be deleted.
Complications of torusal anesthesia
When performing torusal anesthesia, the doctor must be fluent in the technique and be able to easily inject into the desired location.
Therefore, if the patient does not open his mouth wide enough, the needle may move during the injection, which will lead to incomplete numbness of the anesthesia area. A small internal hematoma may also form due to injury to small vessels with a needle.
One of the specific risks of torusal anesthesia is respiratory failure. This is a rare complication and our doctors know the procedure, that is, what to do if they notice breathing problems in their patient.
Anatomical implications
After introducing the anesthetic into the mandibular eminence, the drug immediately begins to act on the mandibular, buccal and lingual nerve endings.
The mandibular ridge is formed from 2 bone cords of the condylar and coronoid processes, they are located above and anterior to the bone uvula, along the slopes of this formation there are 3 nerve endings that lose sensitivity.
Thanks to this effect, sensitivity in the area from the 2nd premolar to the 2nd molar in the middle is turned off, which makes it possible to painlessly perform dental procedures on the dentition and operate on problem areas of the oral cavity.