Removing the nerve or pulp of a tooth is a procedure that can only be done if there are serious indications. For example, if there is severe inflammation or it is impossible to save a tooth without depulping.
- Pulpitis. Often develops against the background of advanced caries. The carious process destroys the enamel gradually. If you go to the clinic in a timely manner, it is not difficult to cure your tooth. In advanced cases, the pulp chamber begins to collapse, and then the pulp becomes inflamed. Inflammation that affects the nerve of the tooth leads to the development of pulpitis. With this disease, it is most often possible to save the tooth only if the nerve is removed. In the early stages of pulpitis, partial removal of the inflamed nerve is possible. This allows you to stop inflammation and at the same time preserve part of the pulp. After surgery, the tissues of such a tooth will continue to receive nutrients, so partial removal of the nerve has advantages over complete removal. The volume of the nerve to be removed will be determined by the doctor based on the diagnostic results.
- Injury. Traumatic pulpitis can develop for various reasons. The most common is a strong blow and destruction of the tooth crown. Dental treatment, for example, deep caries, can also damage the pulp chamber. To drill out all the damaged tissue due to deep caries, the doctor requires experience and almost jewelry work. An inexperienced dentist can damage the pulp chamber during drilling, which can result in traumatic pulpitis. To save a tooth, the nerve often has to be removed after severe trauma to the tooth.
- Retrograde pulpitis. A rather rare disease in which the infection enters the pulp not from the crown, but through the apex of the root. The infection can be transferred to the root of the tooth by the bloodstream from other foci of inflammation: periodontal pocket, maxillary sinuses, etc. Retrograde pulpitis can also develop as a complication of various diseases - influenza, chickenpox, rubella, etc.
- Concretions. If there is a metabolic disorder, hard deposits can form in the dental canals. They put pressure on the pulp, causing permanent injury. As a result, pulpitis may develop over time. If stones are present, nerve removal is almost always required.
It is often necessary to remove the nerve before dental prosthetics. This usually happens when a patient with teeth severely damaged by caries comes to the orthopedist. The doctor will determine whether it is necessary to remove the nerve. If it is not practical to preserve the pulp, the doctor will prescribe removal of the nerve, cleaning and filling of the dental canals.
The orthopedist also evaluates the advisability of removing the nerve if prosthetics require extensive tooth preparation. If there is a risk of injury or overheating of the pulp during preparation, it is more advisable to remove the nerve and reduce the risk of developing inflammation under the installed crown. The doctor always determines the need for depulpation individually in each specific case.
Painless removal of a nerve from a tooth: how it goes and consequences
Many people are familiar with the procedure of removing a nerve from a tooth, which was accompanied by the mandatory placement of arsenic. Previously, this method took several days, during which the substance killed the nerve, after which the doctor removed the pulp and installed a filling or crown. Modern methods make it possible not to resort to arsenic, using more effective and painless methods. The pulp or neurovascular bundle performs important functions; it nourishes and protects tooth tissue from infection. Without it, the enamel changes color, hard tissues are destroyed faster, but in some situations, removal of the nerve is necessary.
What is a dental nerve
Under the coronal part in the root canals there is soft connective tissue penetrated by nerve endings, capillaries, and lymphatic vessels. It is called the pulp, colloquially the nerve. It performs a plastic, sensory, protective, trophic function.
If inflammatory processes occur and untimely therapy occurs, it may die. If it is impossible to preserve the pulp, amputation is performed. Removing the nerve of a tooth leads to fragility of hard tissues, but with correct treatment it will retain its functionality for many years.
Causes of dental pulp damage
The dentist is often visited because of caries - damage and destruction of enamel, which at the initial stage causes aesthetic discomfort.
Important: if the disease is started, the process affects the deeper layers of the tooth and pulpitis develops, that is, the neurovascular bundle becomes inflamed.
Pathologies arise due to the rapid proliferation of microbes, but in addition, the pulp can be damaged for the following reasons:
- gum disease, in which the neck of the tooth is exposed, the bone tissue is destroyed and harmful bacteria penetrate inside;
- trauma, as a result of which part of the tooth can break off, and then microbes enter the resulting cavity;
- mistake by the dentist who installed the filling or crown. If some actions were incorrect, then the nerve will make itself felt after a while.
These are the main causes of pulp damage. The symptoms of this condition will be acute. The pulp will begin to react to cold, hot, too spicy, sweet foods. Removing the nerve in such situations is a necessity, despite the fact that minerals and nutrients will stop flowing to the tooth.
Tooth nerve and need for removal
A tooth is not just a bone. In its roots there is a living pulp - blood vessels with nerve endings. This pulp is called the dental nerve; with its help, the tooth senses heat or cold. If the pulp is removed, the tooth dies, is not supplied with blood, is easily destroyed, and is less resistant to influence.
If a tooth is affected by caries, at first the destruction involves only dentin, the durable tissue of the tooth. But if caries is not treated in a timely manner, it will reach the pulp and pulpitis will begin. Then the pulp has to be removed - completely or partially, and if the pulpitis has reached periodontitis, the pulp has to be completely amputated. The nerve is also removed in case of mechanical destruction or prolonged pain.
Why do you need to remove the pulp?
We talked about the main reasons why nerve inflammation occurs, but most often pulpitis becomes a consequence of advanced caries. Therefore, it is very important to visit a dentist, even if nothing bothers you. The decision to remove the pulp is made in the following situations:
- pulpitis has passed into the stage of periodontitis, when inflammation affects the whole complex of connective tissue in the tooth;
- large area of carious lesion;
- the infection spreads through the apex of the tooth root;
- the appearance of unbearable, prolonged pain;
- spread of infection under an artificial crown;
- consequences of improper treatment.
The nerve can be removed either completely or partially, it all depends on the degree of tissue damage. Depulpation will prevent the spread of the inflammatory process under the crown and preserve the natural tooth, which is a priority for endodontic therapy.
Should I remove the nerve in the tooth or not? That is the question!
Agree, it is quite a common situation when, after treating caries with a therapist or treating a tooth with a crown by an orthopedist, the latter may begin to bother you. One of the controversial questions that patients have to face at this moment is when to remove the nerve in a tooth , and under what circumstances is there a chance to keep the tooth alive? In reality, this question is not always clear-cut for dentists either. In this article we will try to figure out what the difficulty is here.
Firstly, you need to immediately decide that a “living” tooth is always and definitely better than a “dead” one. Because under the “nerve” there actually lies an entire organ, consisting not only of the nerve, but also of blood vessels and other tissues and cells needed by the tooth. And all this is called pulp. It provides the tooth with both nutrition and protection from any external influences. And therefore, without it, it is difficult for our teeth to count on a long and happy life.
But often as a result of caries, injury or dentist intervention (for example, when grinding living teeth for crowns), an inflammatory process can occur - pulpitis . And here it is very important how reversible this process is. This is what is important for the doctor to determine when rendering a verdict on the pulp - to execute it (i.e., depulpate the tooth) or to pardon it (leave the tooth “alive”).
And here we can say that 100% reliable methods for diagnosing the reversibility of the inflammatory process in the pulp do not yet exist. If we had the opportunity to look inside the tooth with a microscope, then determining the vitality of the pulp would not be difficult. But it is impossible to do this on a living patient; such an opportunity is currently available only to pathologists. As a rather cynical saying goes, this is why these doctors are least likely to make a mistake in diagnosis. So what remains for practicing dentists? How can they avoid making mistakes? Which path should you take? You can only rely on much less informative indirect signs and use your experience and intuition.
Let us briefly examine what is still available to us when making a decision.
Patient complaints.
Of course, one of the most subjective signs, however, sometimes very informative. Therefore, it is often enough to listen to your feelings to understand how bad things are with your tooth. Depulpation certainly cannot be avoided if:
- You feel a fairly strong aching pain that occurs without any apparent reason and does not go away for a long time. At the same time, it can intensify when changing the position of the body (mainly when trying to bend over or lie down), and also noticeably intensifies at night. Usually in such a situation, many people run to the pharmacy for a pack of painkillers, although the most correct thing in this situation is to call your dentist with a request for an urgent appointment...
- You do not feel aching pain all the time, but only from some irritant (most often from cold ). The important point is that this pain does not go away immediately after removing the irritant for some time (from several seconds or more).
If, upon contact with cold, you feel only a short, instantly passing pain, then, most likely, everything for the pulp, maybe not right away, will end well. Any other sensations of discomfort, for example, painful biting or sensitivity when touched by a brush when brushing your teeth, are usually associated with completely different things and do not talk about the condition of the pulp.
Cold test.
This point smoothly follows from the first and is based on the inadequate reaction of the inflamed pulp to irritation (primarily to cold). This can be used for diagnostic purposes and, so to speak, to conduct reconnaissance in force. The technique is simple, but with a touch of slight sadism. The doctor cools the cotton ball with a special spray and touches the “suspected” teeth with it one by one.
The resulting response is compared with that of obviously healthy teeth that are 100% above suspicion (i.e., they are on the other side, on the other jaw and do not have carious holes or any traces of previous treatment). If suddenly someone wants to “play dentist” and can’t wait to find a bad tooth themselves, then at home you can do this test yourself by applying, for example, an ice cube from the freezer to different teeth one by one.
In general, self-diagnosis is pointless, but in this case it can still be useful to understand your own feelings, and then more confidently poke the doctor at the problem tooth.
It should be noted that this method is good primarily only in order to understand which tooth is actually bothering you. After all, pulp pain is quite poorly localized, and the patient often cannot say which tooth is bothering him. It even happens that the pain from the causative tooth radiates to the opposite jaw. This happens especially often with pulpitis of 8 teeth (wisdom teeth). Therefore, if in such a situation you trust only the feelings of the patient himself, you can break a lot of wood and depulpate innocent teeth for no reason. It is almost impossible to judge the severity of the inflammatory process and its reversibility using a cold test. For each patient, “oh-yoyoy” and “ah-yayayy” can mean completely different things. Although, as in the first point, by the duration and severity of the pain reaction, the doctor can indirectly judge the hopelessness of attempts to keep the pulp alive.
X-ray.
Another highly informative technique for most cases, which is completely useless for determining the neglect and reversibility of the pulpitic process. X-rays can also only indirectly help identify a problematic tooth if there is any doubt about the “culprit” of the pain. The pulp itself, like soft tissue, does not show any changes on x-ray if it is inflamed. What signs can help a doctor suspect something is wrong?
— location of the previously installed filling close to the pulp chamber
In this image: the red line marks the border of the filling, the blue line marks the border of the pulp. As you can see, they are located quite close to each other.
- hidden, invisible during visual inspection, deep carious cavity in the interdental space
In this picture: the black arrow shows a hidden carious cavity that formed on the back side of the lower 7th tooth under the gum level and led to inflammation of the pulp. The reason in this case was the 8 (wisdom tooth) that was not removed in time.
-presence of denticles in the pulp chamber or root canals
In this image: the yellow line marks the border of the filling, which is close to the pulp (its borders are marked in red). A denticle has formed in the thickness of the pulp due to chronic irritation (marked in blue).
-small reactive expansion of the periodontal fissure around the apex of the tooth root
Electroodontometry (EDO).
This is an old, if not ancient, way to check the condition of the pulp using essentially the same method as with the cold test. Those. irritate her. Only in this case it is no longer a low temperature, but an electric current. This time, nothing sadistic, as everyone usually thinks when explaining the essence of the technique. To carry it out, it is not at all necessary to pass current through the entire patient in some kind of electric chair. It is enough to connect a special small device to the tooth, which generates rather weak microcurrents.
By the value to which the tooth “responds” with slight tingling and pinching, one can judge (again, very approximately, unfortunately) the degree of pulp viability. The advantage of this method compared to the cold test is that instead of “ouch” and “ouch”, the doctor deals with impartial readings from the device. Another thing is that 100% of these indications can only be used to judge whether the pulp is alive at all, or whether it died a hero’s death. Everything else, again, is very conditional.
In the end, what do we have? There are 2 main problems with teeth suffering from pulpitis (or very similar pain : difficulties in some clinical cases in determining the source of pain, and difficulties in making a decision about preserving/removing the pulp. As we have seen, it is not easy for even an experienced and knowledgeable doctor to objectively understand these issues in all cases. If with the first question mistakes can almost certainly be avoided, then with the second... while there are no methods for objectively assessing the condition of the pulp, each doctor will make decisions at his own discretion. Someone, playing it safe, depulps all the teeth in a row indiscriminately. Someone is trying to keep them alive. The more data a doctor can collect and interpret correctly, the risk of making an erroneous decision will be minimized. In general, this is an iron law of medicine: the better and more thorough the diagnosis, the more correct and effective the treatment.
What happens if a mistake is made? I'll tell you one example from my practice. A young girl went to the doctor complaining of aching pain in her teeth “somewhere on the right side.” Without any special diagnostics, treatment began... First, one tooth with a deep filling was depulped, which seemed the most suspicious to the doctor. The pain remains. Then - the next one, the pain did not go away. Then both right normally erupted wisdom teeth were removed. The pain even intensified for a while... Instead of stopping and thinking at that moment, the doctor depulped another 3 (!!!) completely intact (i.e. untouched) teeth on this side, but on the other jaw. When the pain did not go away even after that, the girl, suspecting something was wrong, went to look for reasons in other places. Ultimately, she was diagnosed with trigeminal neuralgia, which, although it is not always well and quickly treated, in her case it was released quite quickly due to the treatment prescribed with the help of a neurologist. The result of the diagnosis using the “finger in the sky” method was 5 completely needlessly killed teeth.
Therefore, it is so important to collect as completely as possible all possible subjective and objective information if the situation is confusing. In this case, the probability of making a wrong decision will tend to zero. In addition, you should strive to preserve the pulp in the tooth, and do not rush into radical decisions if in doubt. At the same time, in borderline cases, you should always monitor the result of treatment, even if the pain has subsided. A cold test, x-rays, and odontometry will be able to promptly identify asymptomatic (“silent”) pulp death and the need for its removal. Otherwise, a cyst may grow completely unnoticed near the root of the tooth. And then there is a risk of losing the entire tooth.
How does the pulp removal process work?
We mentioned the method using arsenic at the very beginning. Some dentists still use it. The disadvantages of this treatment include its duration and pain. Before administering arsenic, the doctor must widen the root canal and place the substance into it. He then seals the area with a temporary filling. After two days, the arsenic kills the nerve, then the dentist cleans the substance from the tooth cavity and removes the pulp.
Important! Arsenic should not remain longer than expected in the oral cavity, as it is a poison and can be destructive to tissue.
There are more modern ways of performing the procedure, which are both safer and more painless. Before any action, an x-ray is required, which shows the vitality of the pulp, the length of the canal and other features.
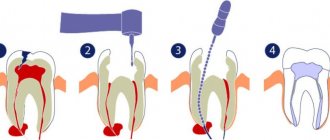
Pulp removal is carried out using the vital and devital method. The first option is used for patients of any age. Its stages are as follows:
- the tooth is exposed;
- the pulp is removed with a special tool - a pulp extractor;
- a filling is installed.
In some situations it may be temporary and after a few days it changes to permanent.
Note: all stages of treatment are performed under anesthesia, so they will not be painful or uncomfortable for the patient.
The devital method is similar to what was used ten or more years ago, only instead of arsenic, a non-toxic substance is installed in the tooth cavity. The main method of pulp removal in modern dentistry is the vital method, when in just 1 visit to the doctor you can undergo complete painless dental treatment.
Important: temporary pain after a dental procedure is considered normal, as tissue intervention has occurred. If severe pain does not go away within 3 days, you should consult a doctor.
Depulpation before prosthetic crowns
Depulpation is unconditional if there is serious tooth decay. It is preferable to remove the dental nerve during prosthetics in the following cases:
- The size of the teeth determines the low position of the crown (too small or short teeth);
- The inclination of the prosthetic tooth is from 15°;
- Increased sensitivity of teeth;
- According to aesthetic requirements.
The need to remove the dental nerve during prosthetics is dictated by deep removal of the top layer of dental tissue: if the doctor is not sufficiently qualified, heating or touching the nerve can cause an attack of unbearable pain. However, cases of nerve-sparing crown installation also occur in modern dental practice.
If over time the nerve under the crown becomes bothersome, it is possible to remove the pulp through the top of the crown and fill the hole after removal.
The danger of such a procedure is associated with the risk of complications in the future due to surgery on the exposed dental nerve.
In what situations should a nerve not be removed?
We are talking not only about contraindications, but also about cases in which the pulp can be preserved. The procedure is not performed if the patient has:
- any infectious disease;
- one of the forms of stomatitis;
- psychoemotional disorders;
- acute pathologies of the heart and blood vessels;
- unsatisfactory condition of the oral cavity with suppuration and inflammation.
The nerve is preserved if it is not subject to inflammation due to caries or other pathologies and injuries. The dentist’s task is to save the pulp and remove it only in case of emergency.
Important: you cannot endure a toothache and hope that the pain in your nerve will stop. Inflammation can become chronic and show almost no effect, but any provoking factor will affect the development of a purulent abscess. In this case, the minimal consequence will be tooth loss, and the possible consequence will be the spread of infection to other tissues.
Indications and contraindications for removal
Pulpitis is treated conservatively and surgically. If it is possible to preserve the pulp, the dentist tries to cure the disease with medications and physiotherapy.
The nerve must be removed in the following cases:
- if the carious lesion has spread to the canals and pulp;
- there is a concomitant disease of periodontitis (inflammation of the periodontium, which holds the tooth unit in the socket);
- severe damage to dentin by caries (large area, presence of several carious cavities);
- mechanical damage;
- the presence of concrements in the canals - hard deposits that cause irritation and inflammation of soft, sensitive tissues;
- lack of positive results from therapy;
- unbearable pain that cannot be relieved by medications.
Depulpation can also be carried out if the orthopedist indicates prosthetics.
The procedure is not performed if:
- stomatitis, acute infections, since pathogenic microorganisms can penetrate deep into the jaw and cause the development of serious diseases;
- poor blood clotting due to the risk of heavy bleeding;
- pregnancy due to the inability to provide the necessary anesthesia.
Consequences of nerve removal
If the treatment was carried out by a professional and experienced dentist, then apart from slight pain the patient will not be bothered by anything. Otherwise, there may be such complications:
- a fragment of the instrument remains in the dental canal;
- the nerve was partially removed;
- incorrect or poor-quality filling of the canal;
- mechanical damage to the root or wall;
- rapid darkening of the enamel;
- suppuration due to poor disinfection.
Important! Depulpation at the Crystal clinic is carried out with the minimum possible complications, since all procedures are carried out by certified doctors with extensive experience using high-tech equipment and tools.
After depulpation, it is recommended not to eat for 2-3 hours, not to eat cold, hot, hard or other foods that irritate the mucous membrane. Your doctor will tell you in more detail about the necessary actions after removing the nerve.
Change in tooth color (darkening of the tooth) - when a nerve is removed
When the nerve is removed from the tooth, after a while (from six months to several years) due to the fact that the nervous, circulatory and lymphatic supply to the tooth has ceased, the color of the tooth changes - discoloration and darkening are noted in the future. If chewing teeth have been depulped, the color change is not noticeable in most patients, unlike the front teeth. Anterior teeth after root canal treatment often require color correction to achieve smile aesthetics. This is achieved through endodontic whitening, veneers, or crowning such teeth. In most cases, when the crown of a tooth is filled or a permanent crown-shaped prosthesis is installed after root canal treatment, this discoloration is not noticeable. In cases where a tooth crown is not required, and the tooth itself is located in the frontal area of the smile, whitening or veneering helps eliminate discoloration of the teeth.
The list of treatments for dental pulpitis includes:
| — Mechanical and medicinal treatment of 1 channel |
| — Pulpitis (simple) root canal filling with three-dimensional obturation system E&Q Plus (1k/k) |
| — Pulpitis (simple) root canal filling with three-dimensional obturation system E&Q Plus (2k/k) |
| — Pulpitis (simple) root canal filling with three-dimensional obturation system E&Q Plus (3k/k) |
| — Pulpitis (complex) filling of root canals with the E&Q Plus three-dimensional obturation system (1k/k) |
| — Pulpitis (complex) filling of root canals with the E&Q Plus three-dimensional obturation system (2k/k) |
| — Pulpitis (complex) filling of root canals with the E&Q Plus three-dimensional obturation system (3k/k) |
Treatment of pulpitis: review of modern treatment methods
When treating pulpitis, the most important task is to eliminate inflammation. For this purpose, conservative procedures or surgical methods that involve complete or partial removal of the pulp can be used. The doctor determines the type of treatment method for pulpitis individually for each patient, taking into account the form of the disease, as well as the stage of its development.
Conservative methods of treating pulpitis
If the patient does not self-medicate and at the first sign of pulpitis seeks professional medical help, then the disease can be treated using a conservative method and at the same time saving both the tooth and its nerve. The diseased tooth is drilled out so that the dentist has access to the pulp. It is treated with special antibacterial drugs and a medical gasket is placed on top, and the drilled tooth is closed with a temporary filling.
The patient will walk with the temporary filling for several days, after which he will return to the clinic for an X-ray. An image is taken to assess the quality of pulp treatment and if it shows that the inflammation has been stopped, the dentist will process the tooth canals, fill them and restore the tooth with a permanent filling.
USEFUL TO KNOW: Conservative methods of treating pulpitis will be effective if all procedures are carried out efficiently. Therefore, it is so important to choose the right dentistry for the treatment of pulpitis.
Surgical methods for treating pulpitis
The surgical treatment of pulpitis may involve either complete or partial removal of the dental nerve. The choice of a specific method depends on the stage of development of inflammation and is determined by the doctor after examining the patient and making a diagnosis. Most often, complete removal of the pulp is used: doctors are forced to make this choice for patients who came to the clinic for treatment of pulpitis too late, waiting for the inflammation to develop to a critical stage.
Complete pulp removal can be:
- Vital. This method involves extracting the dental nerve under anesthesia. To do this, the tooth is drilled with a drill, and all dental tissue affected by caries is removed. The drilled cavity is treated with an antiseptic and then the dentist, using a special tool, removes the pulp, and then fills the canals and tooth. This method is considered universal and suitable for the treatment of various forms of pulpitis, but it cannot be used for patients with allergies to anesthetic drugs;
- Devital. When choosing this pulp removal technology, the dental nerve is first exposed to toxic substances, which are placed in the form of a paste into the tooth cavity for up to 2 days. After the specified time has passed, the patient returns to the clinic, where the dentist removes the dead dental nerve from the tooth, treats the canals and places a permanent filling on the tooth.
This method of treating pulpitis is highly effective, but cannot be used in cases of purulent form of the disease or severe tissue necrosis.
Sometimes amputation is used as a method of treating pulpitis, which involves removing only part of the dental nerve. This method is not applicable for teeth with only one root, since in this case the dentist is not able to accurately identify individual parts of the dental nerve. Amputation is usually performed in the treatment of acute pulpitis.
Removal with arsenic
Once upon a time there was only one way to remove it, it was terribly painful, especially since you had to visit the doctor several times. At first, the doctor drilled the tooth down to the pulp with a drill, which was extremely painful. Next, arsenic was placed in the hole and it was temporarily sealed with a filling. In a couple of days, the arsenic dealt with the nerve, and the tooth hurt so much that no medicine could help. Then I had to go to the doctor again, he opened the temporary filling, removed the nerve, and cleaned the root canals. Pulp is a tenacious substance, so this process was also extremely painful.
This technology poses a certain danger, because arsenic is a poison, and the doctor, when using it, must be especially careful, and the patient must be careful: if you are late with the second visit to the doctor and leave arsenic in the tooth, it will completely destroy it, which will end deletion. Dentists stopped using arsenic and developed new techniques for removing pulp.