Endodontic treatment of teeth for pulpitis and periodontitis takes up to 35% of the working time of a dentist, requiring high-quality mechanical and medicinal treatment of the canals. However, microflora in the form of biofilm in inaccessible areas of the root canal system is not completely removed in one visit, as a result of which the percentage of successful treatment does not reach maximum values. Thus, after lateral condensation of gutta-percha, complications account for 5 to 20% of all cases of endodontic treatment.
Significantly reduces periapical inflammation by disinfecting root canals with calcium hydroxide, which is a white powder without taste or odor, in an aqueous solution has a pH of about 12.5, breaking down into calcium and hydroxyl ions.
Antimicrobial activity is provided by the following mechanisms.
Damage to the bacterial cytoplasmic membrane: hydroxyl ions accelerate lipid peroxidation, which leads to the destruction of structural components of the cell membrane.
Denaturation of microbial cell proteins: alkalization of the environment with calcium hydroxide leads to the destruction of ionic compounds that support the tertiary bonds of proteins, loss of biological activity of the enzyme and disruption of cellular metabolism.
Destruction of gene structures: hydroxyl ions react with bacterial DNA, which leads to a disruption of their spatial structure. As a result, DNA replication is inhibited and cellular activity is disrupted.
The antimicrobial effect of calcium hydroxide is most significant immediately after applying the drug to the root canal.
The concentration of hydroxyl ions decreases as a result of the action of buffer systems (bicarbonate and phosphate).
At the same time, antibacterial activity decreases.
Calcium hydroxide has an effect on the periapical tissues, promoting the formation of a layer of coagulative necrosis, causing mild irritation of the underlying tissues, the formation of a connective tissue layer, which subsequently undergoes mineralization. The alkaline pH level neutralizes the lactic acid of osteoclasts, protecting the mineral components of dentin and bone from dissolution, and activates alkaline phosphatases, which play an important role in the formation of hard tissues.
The practical use of calcium hydroxide preparations is designed to solve the following problems:
- reduction in the number of intracanal microorganisms;
- removal of the maximum amount of necrotic tissue;
- reduction in the concentration of bacterial endotoxins.
Mechanical treatment in combination with irrigation of medications does not provide complete disinfection of the canal and removal of necrotic tissue. Effectively reduces the amount of bacterial flora, and also dissolves living and necrotic organic tissue. Temporary filling with calcium hydroxide. The latter also reduces the amount of bacterial endotoxins.
Materials for temporary canal filling
There are conflicting opinions about the need to replace calcium hydroxide paste in the canal with new portions. HSChawla suggests that a single application is sufficient. A. Chosack et al. It is believed that repeated administration of calcium hydroxide is necessary after 1-3 weeks. Proponents of one-time fillings point to the fact that the hydroxide is only needed to initiate the reparative reaction, so no replacement of the drug is required. Many authors suggest re-introducing calcium hydroxide paste into the canal only when symptoms worsen.
The results of the study showed that Ca(OH)2 in its pure form is not always effective in destroying microbes, for example E.faecalis, C.albicans. A paste of calcium hydroxide with iodoform turned out to be more effective, penetrating into the tubules to a depth of more than 300 microns.
Calcium hydroxide paste with paramonochlorophenol and glycerol killed bacteria, including E. faecalis, within 24 hours of use. Calcium hydroxide in combination with 2% chlorhexidine gel has increased antimicrobial activity against resistant microorganisms.
The question of how long the hydroxide remains in the channel remains controversial.
In accordance with the recommendations of most companies, the duration of stay of the products in the tooth is up to 14 days, which creates some inconvenience in the work, namely, some patients do not complete the treatment, forgetting about the need to visit the dentist again. On the other hand, research results have shown that the paste creates an antibacterial effect after just 1 day of use. Calcium hydroxide causes complete inactivation of various types of microorganisms within 12-72 hours (Stuart et al., Estrela et al.). The combination of chlorhexidine and hydroxide inhibits the growth of E. faecalis 100% after 1-2 days of contact.
These results are confirmed by our own microbiological studies of the contents of the root canal after each of the three stages: standard mechanical and medicinal treatment; additional medicinal effects with a 2% solution of chlorhexidine for 2-3 minutes; temporary filling with calcium hydroxide or hydroxide in combination with iodoform for 48 hours. For this purpose, scraping was carried out from the walls of the root canals with an H-file, which was placed in a sterile tube with a transport system (2 ml of trypticase soy broth). The latter was delivered in thermal containers to the microbiological laboratory (40 samples).
0.1 ml of the prepared homogenizate was continuously inoculated onto a blood agar plate. Petri dishes were placed in a thermostat. Cultivation was carried out at 35-37 0C for 48 hours. When growth appeared, colonies were counted by determining CFU per 1 ml. Gram-stained smears were examined under a light microscope for the purpose of generic identification of microorganisms. In root canals with an initially low degree of contamination after standard mechanical and medicinal treatment, the number of microorganisms was 100 CFU/ml. Temporary filling of the canals with a paste based on calcium hydroxide made it possible to reduce the number of microorganisms to the level of 0[0/0] CFU/ml.
With an initially high degree of contamination, the contamination of the canals decreased significantly at each stage of the study. Thus, after standard treatment, the microbial number was 1,400 CFU, after drug treatment with a 2% chlorhexidine solution - 200 CFU, after temporary filling (for 48 hours) - 0 [0/100] CFU.
Thus, the use of additional medicinal treatment and temporary filling makes it possible to reduce the number of microorganisms in the root canal to a minimum.
Preliminary clinical trials have shown that reducing the residence time of calcium hydroxide in the canal under a temporary filling to 48 hours reduces the risk of incomplete treatment of pulpitis and periodontitis by 8-11%, and the combined use of calcium hydroxide preparations with iodoform reduces the number of complications by 5-25%.
Indications for temporary filling of root canals
Temporary filling with a paste based on calcium hydroxide is indicated for chronic pulpitis with a closed tooth cavity that has 2 or more root canals; chronic apical periodontitis with a closed tooth cavity having 2 or more root canals; acute apical periodontitis of pulpal origin with a closed tooth cavity.
Temporary filling with a paste based on calcium hydroxide with iodoform is indicated for acute purulent pulpitis with an open and closed tooth cavity; chronic ulcerative pulpitis with an open tooth cavity; chronic hyperplastic pulpitis; pulp necrosis with open and closed tooth cavity; acute apical periodontitis of pulpal origin after the removal of acute phenomena; chronic apical periodontitis with an open tooth cavity.
All patients in need of endodontic treatment are prescribed an X-ray examination at the stages of measuring the working length, filling the root canals, as well as in the long term.
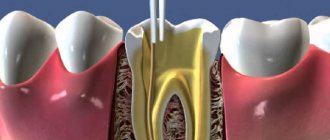
Instrumental treatment, which involves eliminating the source of infection and forming the required shape of the root canal, is carried out using the “Step Back”, “Crown Down” or a mixed method.
After mechanical processing, a funnel-shaped canal is formed with a minimum diameter in the apex area and a maximum at its mouth; a balance is maintained between the diameter of the channel and the thickness of its walls; a constant position of the apical foramen is ensured; an apical stop is created to prevent the filling material from being pushed into the periodontium. Medicinal treatment is carried out, the walls of the root canal are dried using paper points.
In the treatment of pulpitis without symptoms of apical periodontitis (low contamination of the canals), the method of temporary filling of root canals with calcium hydroxide-based paste is used. In case of pulpitis with symptoms of periodontitis, chronic periodontitis, acute and at the acute stage of chronic periodontitis (after acute symptoms have resolved), the root canals are additionally treated with a 2% solution of chlorhexidine (exposure 2 minutes), after which they are temporarily filled with a paste based on calcium hydroxide with iodoform.
Method of temporary filling of root canals
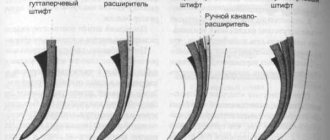
Filling a canal with paste can be done either manually or using a canal filler.
Method of “manual” filling. Using a limiter, the working length of the canal is fixed on a K-file, K-reamer or on a special cannula - a syringe attachment. At the tip of the instrument, a small amount of paste is introduced into the equine canal up to the apex. Condense the paste using a damp cotton pad. The next portion of paste is injected to 2/3 of the working length of the canal.
Condense the paste in the same way. The next portion of paste is injected to 1/3 of the working length of the canal. Excess paste that has accumulated above the mouth is pressed into the canal using a cotton ball. The tooth cavity is hermetically sealed with a temporary filling for 48 hours.
Filling technique using canal filler. The canal filler, a size smaller than the last instrument used to expand the root canal, is fixed in the tip and the working part is immersed in the paste, retaining a small amount of material on the spiral. The instrument is inserted into the canal up to the apex, turned on at low speed (100-120 rpm) for 2-3 seconds, then the instrument is slowly removed from the canal while the drill is running.
The canal filler is again enveloped with filling material, inserted into the canal to 2/3 of the working length, the drill is turned on and the material is pumped into the canal, then the procedure is repeated. Excess paste that has accumulated above the mouth is pressed into the canal using a cotton ball. The tooth cavity is hermetically sealed with a temporary filling for 48 hours. If there is painful percussion, the canal is filled again at the next visit.
If the apical opening is wide or it was expanded during instrumentation, then the first portion of the paste is injected and condensed “manually” and only then the canal filler is used.
On the second visit, the remains of the temporary sealer are removed from the root canal using an H-file of the required size using scraping movements. Scraping is periodically alternated with irrigation of the root canal with an antiseptic solution using an endodontic syringe with a needle until the temporary sealer on the H-file is completely removed, after which the root canal is dried with paper points and filled using the sealer and gutta-percha points using the lateral condensation method. For permanent filling, according to indications, sealers are used, which contain calcium hydroxide with iodoform, zinc oxide eugenol, hydroxyapatite, and glass ionomer cement.
Assessment of the quality of endodontic treatment is carried out immediately after treatment and in the long term (after 6, 12 months). The criteria for clinical well-being are: absence of complaints; painless percussion; normal state of the transitional fold in the area of projection of the apex of the root of the tooth under study; positive dynamics or absence of pathological changes in the tissues of the apical periodontium on the radiograph.
Efficiency of temporary filling of root canals
Postgraduate student of the Department of Therapeutic Dentistry of BelMAPO O. V. Fedorinchik assessed the immediate results of endodontic treatment in study groups I (pulpitis without periodontitis) and II (with apical periodontitis).
After treatment, there were no complaints in 75.0% of cases in the control (without the use of calcium hydroxide); after temporary filling, this figure reached 95.2%. Within 1-2 days, complaints of pain when biting were reported in 11 cases (17.2%) in the control group; in the main group they were recorded in only three teeth (4.8%).
On days 3-5, in the control group, pain persisted in 5 teeth (7.8%), while in the main group it was absent.
In group II, complaints of pain after endodontic treatment were absent in the control group in 50.8% of cases, in the main group - in 85.7%. Pain when biting 1-2 days after treatment was noted by 22 patients (36.1%) in the control group and 6 (10.7%) in the study group.
On days 3-5, pain in the control group was 13.1%, i.e. 8 cases, and only 2 (3.6%) in the main group. Thus, when using temporary root canal filling, pain is significantly reduced.
The results of endodontic treatment after 6 months are presented in Table No. 1. In the main group, in 100% of cases there were no complaints of pain in the area of the treated tooth. In the control group, complaints of periodic pain were reported in one case. An X-ray examination in the control group revealed an expansion of the periodontal gap in the apical periodontal tissues in five teeth (7.8%), in the main group this figure was recorded in one case (1.6%).
When using a paste with iodoform for temporary filling, there were no complaints of pain in 98.2% of patients, and periodic pain was observed in only one tooth (1.8%). At the same time, in the control group there were no complaints in 72.1%, and periodic pain in the area of the treated tooth was bothersome in 17 cases (27.9%).
On the radiograph in the control group, there were no changes in the periodontium in 55.7% of cases, in the main group - in 80.4% of treated teeth.
At a follow-up examination after 12 months in group I (pulpitis), there were no complaints of pain in the control group in 95.3% of cases; in the main group there were no complaints in 100% of cases. Periodic pain in the area of the treated tooth was recorded in the control group in 3 cases, 4.7%. X-rays after 12 months showed no changes in the apical periodontal tissues in 85.9% of the teeth in the control group; in the main group, this figure reached 98.4%. In the apical region of 9 teeth (14.1%) in the control group, an uneven expansion of the periodontal fissure was noted, while in the main group these changes were recorded only in one case (1.6%).
In the main group II (apical periodontitis) there were no complaints in 100% of cases, in the control there were no complaints in 93.4%.
During X-ray examination, the absence of changes in the apical periodontal tissues was noted in 73.8% of cases in the control group. In the main group, this figure reached 92.9%. The expansion of the periodontal fissure in the area of the apical periodontium was preserved in 12 teeth of the control group (19.7%). In the main case - in 4 cases (7.1%).
Conclusion
Studies have shown that temporary filling of root canals can statistically significantly reduce the incidence of complications in both pulpitis and periodontitis. 6 months after treatment of pulpitis, the number of complications was minimal.
Complaints about pain and radiological changes in the area of the treated tooth were significantly less common in the main group. After 12 months, positive radiographic dynamics were more often observed in the main group, where a paste based on calcium hydroxide with iodoform was used.
LITERATURE
- Antanyan A. A. // Endodontics today. - 2007. - No. 1. - P. 59 - 69.
- Kazeko L. A., Fedorova I. N. Calcium hydroxide in endodontics: yesterday, today, tomorrow // Modern dentistry, 2009. - No. 2. - P. 4 - 9.
- Lopatin O. A., Fedorinchik O. V. The use of calcium hydroxide preparations in the treatment of complicated caries // Modern dentistry, 2007. - No. 3. - P. 33 - 37.
- Lutskaya I.K. Restorative dentistry: equipment, tools, auxiliary materials. - Rostov-on-Don: Phoenix, 2008. - 202 p.
- Lutskaya I.K., Martov V.Yu. Medicines in dentistry. - M.: Medical literature, 2007. - 384 p.
- Lutskaya I.K., Chukhrai I.G., Novak N.V. Endodontics: A Practical Guide. - Moscow: Medical literature, 2009. - 191 p.
- Bartlett D. A difference in perspective - the North American and European interpretation of tooth wear / D.Bartlett, K.Phillips, B.Smith // Int. J. Prosthodont. - 1999. - Vol. 12, No. 5. - P. 401 - 408.
- Basrani B., Santos JM et al. // Oral Surgery Oral Medicine Oral Pothalogy Oral Radiology & Endodontics. — 2002. — Aug; 94(2). — P. 240—245/
- Cwikla S., Belanger M., Giguere S., Vertucci F. // J. Endod. - 2005. - V.31, No. 1. - R. 50-52.
- Gomes B., Souza S., Ferraz C. // Intern. Endod. J. - 2003. - V. 36. - P. 267-275.
- Ingle JI, Bakland LK Endodontics. - Baltimore$ Philadelphia et al., 1994. - P. 230-241.
- Katebzadth N., Hupp J., Trope M. Histological signs of periapical inflammation after obturation of infected root canals of teeth in dogs // Journal of Endodontics 25, 1999: 364 -8.
A complete list of references is in the editorial office.
How to understand whether the root canal is filled properly
Signs of a properly treated canal are visible on x-ray: filling to the tops of the root, dense filling of the canal without any excess or voids. It is not desirable to have material residues outside the root canal. If the paste does not dissolve, an inflammatory process may develop in the future. But the quality of work depends not only on the attending physician: the patient himself also plays an important role. By following all the dentist’s recommendations, observing the rules of oral hygiene, as well as a careful approach to the health of your teeth, this is the only way you can achieve the desired results.
Root canal treatment and filling should always be trusted only to experienced specialists. An experienced dentist in Minsk is waiting for you at the Family Dentistry Center. Comfortable treatment, modern equipment of European quality, highly qualified specialists and an individual approach to each patient. Thanks to the use of drug sedation, all procedures can be performed without stress and pain, and children's fears of the dental office will go away on their own.