No one is immune from jaw displacement. Dislocation of the lower jaw can occur either as a result of a blow or when the mouth is suddenly opened. But there are a number of factors that provoke the occurrence of such situations. How to behave if jaw displacement occurs? How soon can it be put back in place, and where should one go if the lower jaw is dislocated? Experts answer these questions.
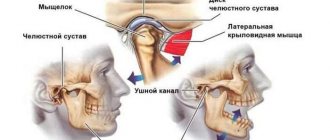
Dislocation of the lower jaw is a situation when the articular head of the temporomandibular joint is displaced. Dislocation can only affect the lower jaw, since the upper jaw is immobile. The mandible is connected to the temporal bone by the TMJ, which helps the mandible move.
Why does dislocation of the lower jaw occur?
Mandibular displacement can occur because:
- the patient suddenly opened his mouth during a conversation or yawned;
- the man dropped his jaw sharply;
- the patient suffers from certain diseases that have weakened the skeletal system and articular ligaments. Among the most common diseases that provoke dislocation of the lower jaw are osteomyelitis, rheumatism, arthritis, etc.;
- a person has a habit of opening bottles with his teeth;
- the temporomandibular joint was affected due to improper distribution of the load on the teeth (for example, if on one side there are no chewing teeth, but on the other side they are there and do more work).
Causes
The reasons for displacement of the jaw bones from their original position can be divided into 2 categories: traumatic and non-traumatic. The first category of factors provoking the problem include: bruises, accidents, falls, blows.
Non-traumatic causes include:
- chewing rough foods;
- wide opening of the jaw by a person during yawning;
- diseases of the ligamentous apparatus (rheumatoid arthritis, osteoarthritis, osteomyelitis).
If medical care is not provided in a timely manner, swelling and hematoma gradually appear in the area of the dislocation. Lack of adjustment also leads to the transition of the dislocation to the old stage. The disorder is characterized by weakening of the jaw muscles, the formation of compacted scars at the site of injury, and the inability to hold the jaws in an anatomically correct position even after reduction. A person's chewing and speech functions are impaired.
How to understand that a dislocation of the lower jaw has occurred?
The symptoms of dislocation of the lower jaw are quite clear:
- it becomes impossible to open your mouth;
- pain is felt in the projection of the jaw, as well as in the area of the temporal bone;
- after dislocation of the lower jaw there may be speech impairments;
- redness may be observed in the area of the temporomandibular joint;
- the lower jaw is pushed forward or shifted to the side;
- against the background of joint dislocation, uncontrolled salivation occurs.
As a rule, a person immediately understands that something is wrong with the lower jaw. Visually, the displacement of the lower jaw is also visible. If you notice similar symptoms of dislocation, you should urgently seek help from a doctor.
Classification and main symptoms
Dislocations can be unilateral, affecting one joint, or bilateral, in which the jaw moves forward, the mouth remains open, and speech function becomes difficult. Injuries are also divided into anterior, posterior, lateral, acute, chronic, congenital, acquired. If the dislocation does not violate the integrity of the skin, it is considered simple. When a rupture of the skin and soft tissue is observed, a complicated condition is diagnosed.
With a bilateral dislocation, it is painful for the victim to speak, he cannot close his teeth and lips, and there is severe discomfort in the behind-the-ear area. The chin shifts forward and the cheeks flatten. With unilateral dislocation, the following symptoms are observed:
- facial asymmetry;
- inability to close the jaw;
- displacement of the chin to the healthy side;
- crunching and clicking sounds;
- pain in the damaged area.
Anterior and posterior dislocations are characterized by identical signs: difficulty swallowing and breathing, slurred speech, sharp pain in the parotid area, forced bending of the head forward, hemorrhage in the external auditory canal.
What types of dislocations of the lower jaw are there?
Depending on the side of displacement of the articular head, there are:
- posterior dislocation of the lower jaw (when the jaw moves back);
- anterior dislocation of the lower jaw (when the jaw is pushed forward).
Based on the nature of the injury, we can distinguish:
- complex dislocation of the jaw, when soft and hard tissues are affected, and an open wound is visible;
- simple or closed dislocation of the lower jaw, when the displacement of the jaw bones is not visualized.
Based on the number of affected joints (and there are two of them) in articular dislocation of the lower jaw, the following are distinguished:
- bilateral dislocation of the lower jaw is a complex diagnosis in which the jaw “pops out” of both joints and is therefore pushed forward, the mouth remains slightly open, the jaw moves forward, the person is drooling, and there are problems with speech;
- unilateral articular dislocation of the lower jaw, when one temporomandibular joint is involved, while the chin shifts towards the unaffected joint.
If, when the lower jaw is dislocated, the tips of the bones do not touch each other, a complete dislocation of the lower jaw is diagnosed. If the ends of the bones partially touch, most likely the patient has articular subluxation of the lower jaw.
Description of the problem and its symptoms
Only the lower jaw is mobile, so when they talk about dislocation, they mean it. A dislocation is an injury to the mandibular-temporal joint with its displacement from the anatomically correct position. In this case, the articular head pops out of the fossa of the articular-temporal bone.
Dislocation is divided into complete (when the head completely flies out of the fossa) and partial (when the head is displaced relative to its normal position, but is in the fossa). Subluxation is considered less dangerous and can be corrected at home by the victim himself.
Injury to the lower jaw is not always visible to the naked eye. Sometimes the damage is felt only by the victim himself. The main signs of a dislocation include: aching pain in the area of injury, radiating discomfort into the ear, and increased symptoms when trying to open the mouth. At the moment of complete dislocation, the victim may hear a click, characteristic of the head coming out of the articular fossa.
The symptomatic picture of the disorder depends on the type of injury. In an anterior dislocation, the damaged bone structure sags and moves forward. At the same time, the patient notes increased salivation and difficulty pronouncing words.
Additional signs of anterior dislocation:
- facial asymmetry;
- inability to close the mouth independently;
- displacement of the jaw to the right or left.
In a posterior dislocation, the damaged bone structure moves backward. A typical clinical picture of the injury: partial hearing impairment, swelling of the auricle. These symptoms arise because with a posterior dislocation, a fracture of the ear canal wall often occurs.
Signs of bilateral dislocation:
- difficulty breathing (especially when lying down);
- inability to open the mouth without outside intervention;
- increased pain when sitting.
How can you determine that a dislocation of the lower jaw has occurred?
As we said above, based on the symptoms, the patient immediately understands that something is wrong with his lower jaw. A doctor will be able to make an accurate diagnosis based on the following diagnostic steps:
- general examination;
- radiography of the jaw;
- computed tomography or MRI of the joint.
The specialist must also make sure that the dislocation or subluxation does not hide a fracture of the jaw, which is much more serious and requires surgical intervention.
It is important! If a person has a dislocation of the lower jaw as a result of injury or an accident, he should be given first aid - apply a tight bandage to the jaw and take him to a medical facility.
Displacement classifications
Dislocations are classified according to certain criteria:
- Unilateral - the head of the joint moves out of its normal position, the mouth opens, and the jaw moves to the healthy side.
- Bilateral - considered the most common, the mouth is completely open, the jaw is pushed forward;
- Complete - the articular surfaces do not touch.
- Incomplete (subluxation) – there is partial contact of the joints; if the soft tissue is ruptured, it is considered complicated.
- Habitual – diagnosed when a dislocation occurs with light pressure on the jaw or chewing, this is the only way when you can correct it yourself; surgical intervention will help prevent further displacement. As part of its implementation, an increase in the depth of the cavity or the height of the tubercle is provided, and the joint capsule is also strengthened. Sometimes additional support is created, which ensures its fixation in the desired position.
- Posterior – the main cause is considered to be a blow to the chin, as a result of which the jaw moves back. Such a dislocation is the most dangerous, as it leads to rupture of the capsule and damage to bone tissue, which leads to ear bleeding.
Treatment of lower jaw dislocation
To solve the problem of dislocation of the lower jaw, the jaw should be moved back into place. This should be done exclusively by an orthopedic traumatologist or orthopedic dentist. Adjusting bones yourself after a dislocation is fraught with complications - do not try to repeat the same thing at home, contact a professional.
The procedure for realigning a patient's jaw consists of 5 main steps:
Step No. 1 - the person lies down on a hard surface, takes a comfortable position;
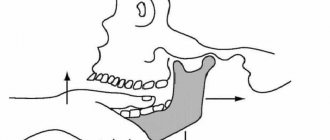
Step No. 2 - the doctor places his thumbs on the chewing teeth of the lower jaw, the remaining fingers seem to clasp the lower part of the face;
Step No. 3 – the specialist makes movements, moving the jaw back and down, but at the same time slightly lifting the chin;
Step No. 4 - the doctor must make sure that the articular head has moved down the back of the TMJ tubercle and returned to its original position;
Step No. 5 – the doctor needs to have time to remove his fingers from the teeth so that the person does not automatically bite them, closing the jaw.
Repositioning the jaw after a dislocation takes several minutes, but must be done very carefully.
If a person’s jaw has been dislocated for a long time and for some reason he has not consulted a doctor, the bones have shifted, he is prescribed surgery under local or general anesthesia.
In case of complex dislocations, a person is recommended to have a reconstructive operation, in which the height of the articular tubercle is artificially increased, while the articular capsule is reduced. Thus, an optimal balance of the elements of the connecting apparatus is achieved, and the jaw does not move.
As a recovery after jaw realignment or surgery to correct a dislocation, the patient is recommended to wear special orthodontic appliances.
First aid and treatment measures
Before the doctor arrives, it is necessary to make a bandage for the jaw from scrap materials.
It is highly undesirable to deal with the problem yourself. First aid for a person with a dislocated lower jaw is to call a doctor. You can contact a traumatologist, surgeon, or dentist. Before the specialists arrive, it is necessary to calm the victim, not allow him to speak, laugh, or move his jaw. You should make a bandage from a scarf or scarf that will fix and support the joint, avoiding complications.
When the mouth is dislocated, it remains in an open position, making swallowing difficult. Therefore, the oral cavity must be covered with a handkerchief (gag) so that saliva is easily absorbed and does not flow down the chin. In addition, the gag will serve as reliable protection against infections and various contaminants.
If it is not possible to get medical help or go to the emergency room, the dislocation can be corrected independently, using one of three methods.
Reduction according to Hippocrates
Reduction of the jaw according to Hippocrates.
Used for simple dislocation. The patient is seated so that the head rests against the wall and the level of the jaw is at the level of the reducer's elbows. Further:
- Local anesthesia is performed with lidocaine solution or another analgesic.
- Hands are thoroughly washed, disinfected with an antiseptic, and thumbs are wrapped in a bandage to avoid possible injury if the patient’s jaw suddenly closes.
- The thumbs are placed on the molars, and the rest hold the lower jaw.
- The jaw is carefully moved slightly down, while pressing on the chin. The jaw is moved back, then slightly upward, so that the head of the joint returns to the notch.
If the manipulation is carried out skillfully, a characteristic click will be heard, indicating that the bone has fallen into place. As soon as this happens, the jaw will reflexively close, so it is important to react quickly and stick your fingers out of the patient’s mouth.
Blechman-Gershuny technique
When the depth of the jaw sockets is shallow, the Blechman-Gershuny technique is used.
The simplest and fastest way to reduce a dislocated temporomandibular joint. Suitable for dealing with simple bilateral dislocations, but requires good reaction and coordination:
- the setter feels the arches of the cheekbones and finds the processes of the jaw bone;
- Use your fingers to move the bone down and back until a click appears.
The jaw can be adjusted both from the outside and from the inside by feeling the coronoid processes on the inside of the mouth. The main thing is to be able to find the right place and have a certain skill.
It is recommended to resort to the Blechman-Gershuny method for frequent simple dislocations caused by weakening of the ligaments or insufficient depth of the articular sockets.
Popescu technique
A cardinal method that can only be used by a specialist with the appropriate skills and experience. The victim lies down on the couch. The damaged area is treated with an anesthetic and, if necessary, general anesthesia is given. A 1.5 cm thick bandage roll is placed between the teeth. Press firmly on the chin upward and then back, after which a click is heard.
How to behave after lower jaw reduction?
If the doctor has successfully adjusted the lower jaw, the patient is recommended to wear a thick elastic bandage for 10 to 14 days, which will securely fix the bones.
During this time, you should stop eating solid food - it is better to concentrate on liquid soups, pureed cereals, fruits and berries. It is important not to overload the jaw with chewing load, so as not to provoke re-dislocation.
With successful reduction of the lower jaw after dislocation and a professionally performed operation, the prognosis for the patient is favorable. In some cases, jaw mobility may be impaired.
If you or your loved ones have a displacement of the lower jaw, contact dental specialists. Here, experienced doctors will help you with dislocations even in the most difficult cases.
Symptoms of a dislocated jaw
Regardless of the type of jaw dislocation, there are several common symptoms that help identify it. These include difficulty opening and closing the mouth, protrusion or skew of the lower jaw relative to the norm, difficulty speaking, severe salivation and sharp pain in the lower jaw, radiating to the temple.
In addition, jaw dislocation is accompanied by severe pain in the parotid region, as well as in the lower jaw area. The patient loses the ability to speak clearly because he cannot close his mouth. There is increased salivation. Depending on the type of dislocation, the pain may affect only one or both sides of the skull. Changes in the position of the lower jaw are externally noticeable. It may be pushed forward or skewed.
A jaw dislocation can be diagnosed by external examination, but to differentiate it from a fracture, an x-ray examination is necessary.
You won’t be able to straighten your jaw if it’s dislocated on your own. It is necessary to contact specialists as soon as possible. However, as a first aid measure, the patient's mouth should be covered with a handkerchief to prevent dust and foreign bodies from entering it. The jaw can be temporarily supported with a bandage. Applying cold helps relieve pain.
First aid
If you have dislocated your jaw, you should not make sudden movements, as they can lead to a deterioration in your health. In case of severe pain, it is recommended to take any analgesic, but only if you are sure that you are not allergic to its components. With this pathology, there is already an increase in blood pressure and difficulty breathing, and an allergic reaction to an unfamiliar drug will only worsen the condition.
Then you need:
- Fix the knocked-out jaw in one position with a bandage made from available materials (as with any other sprain) to prevent it from moving even further.
- Make something like a gag out of absorbent fabric to remove excess saliva.
- Call an ambulance. If you are unable to speak on your own, you should ask neighbors, passers-by, or employees of nearby stores to call an ambulance if the injury occurred on the street. If there is a hospital nearby, it is better to go straight to the emergency room of a medical institution.
It is not recommended to speak if the jaw apparatus is injured
, since any movements of the mouth will be painful. Trying to straighten your jaw at home without proper practice is also not worth it.
Self-treatment of a jaw dislocation, even if it occurs during normal yawning, can lead to long-term joint dysfunction and damage to the setter's fingers.
How to straighten your jaw yourself
A dislocated jaw can be adjusted at home, but this should only be done by someone with appropriate experience and/or medical training. Jaw joint insertion at home should not be done by non-professionals. Below are general recommendations for the procedure. In any incomprehensible and emergency situation, it is better to call 03 - skull bones are not to be trifled with!
To insert a dislocated articular head into the fossa, you must:
- Place the victim on a hard chair next to a wall.
- Tilt the patient's head towards the wall.
- Wrap your thumbs in a thick towel, as slamming your jaws sharply can damage them.
- Stand opposite the patient and ask him to open his mouth as wide as possible.
- Place your thumbs on your bottom teeth.
- Use the remaining fingers to clasp your chin.
- Use your thumbs to press down on your teeth, and with the rest, lift your chin.
- Quickly remove your fingers from your mouth or at least move them towards your cheeks.
- Insertion of the jaw will be accompanied by a characteristic click.
The photo shows the principle of jaw realignment
With a bilateral dislocation, you need to straighten each side separately, and with a unilateral dislocation, try to put pressure only on the sore spot.
Treatment for jaw dislocation due to yawning
When yawning, it is usually not a full-fledged dislocation, but a subluxation that can be treated at home.
To do this you need:
- Fix the jaw.
- Anesthetize the injury site.
- Apply ice wrapped in a towel to the injury site.
- Hold the ice for 5 minutes every hour.
Dislocation of the jaw joint can occur at any age and at any time, even when yawning. If a pathology occurs, you should not try to cure it yourself; it is better to consult a doctor: he will know exactly what to do.
More details about what to do in case of a dislocated jaw are described in the video:
Classification
All jaw dislocations can be classified according to various indicators:
| According to the placement of the articular head relative to the fossa (it is indicated in which direction it came out) |
|
| By location: |
|
| By statute of limitations: |
|
| By severity: |
|
| By etiology: |
|
Any dislocation can and should be treated. Immediately after the incident, you should go to a hospital or emergency room to seek qualified medical care.