Ridge splitting is a type of bone grafting - a procedure that increases the volume of bone tissue. This operation is often required before implantation if there is a lack of bone tissue. There are various bone grafting techniques, but we will look at one very common one – bone splitting.
Indications for bone splitting surgery
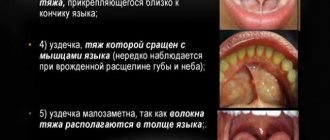
- Narrow ridge of the jaw, this often happens on the lower jaw;
- Long absence of a tooth in the jaw - during this time the bone decreases and it becomes insufficient for installing an implant;
- Anatomical features in which a person initially has little bone tissue.
There are implantation methods when bone grafting is not required, but they are not classical and should be considered individually with the dentist.
In order for the splitting of the bone crest during implantation to proceed as it should, two basic conditions must be met:
- Its minimum height should be 8 millimeters;
- The width of the bone should be at least 3 millimeters at its narrowest point.
Why is the operation performed?
In the presence of a narrow ridge, it is impossible to carry out high-quality dental restoration, especially on toothless jaws. The jaw may have this shape naturally or acquire it as a result of atrophy, injury, removal of a tumor, or a previous disease. Indications for surgical intervention:
- Insufficient tissue volume.
- Thin alveolar process.
- Atrophy or other defects of the jaw.
Carrying out bone grafting
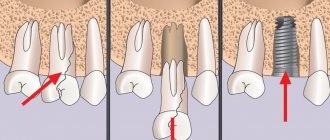
Bone grafting using the method of splitting the alveolar ridge is carried out in several stages:
- The surgical area is numbed through an injection using local anesthetics. This guarantees complete loss of sensitivity in the intervention area;
- The gum is cut and peeled off using a scalpel, the dentist gains access to the bone;
- A horizontal incision is made in the bone itself with a scalpel or laser;
- The edges of the alveolar ridge are moved apart, creating an empty space between them;
- The surgeon introduces the selected material into the space to form bone tissue;
- If necessary, the surgeon can place a protective membrane on top;
- The implant is installed;
- The gum is returned to its place and stitched with special surgical sutures.
All this is done quite quickly - the operation, even in complex cases, does not last more than an hour. During the procedure, the patient feels absolutely nothing.
Systems used
The benefits of using split ridge surgery include:
- elimination of atrophy, effective installation of an artificial root without plastic surgery;
- formation of a bone base with proper density;
- reduction of the rehabilitation period;
- prosthetics are performed after 3-4 months;
- tissue restoration is rapid;
- The integration process is excellent, there are practically no complications.
Disadvantages include:
- a large number of restrictions and contraindications;
- inability to use four or more units for restoration;
- high requirements for the qualifications of a doctor.
Preparation and installation
Before you begin the split-ridge installation procedure, you must complete a number of preparatory measures:
- visual examination, diagnostics to determine the possibility of surgery;
- laboratory tests to identify contraindications;
- allergy tests for the medications used;
- hardware study of the structure of the dental system;
- sanitation, elimination of oral diseases;
- office cleaning.
The surgery is performed under local anesthesia and the following steps are followed:
- administration of anesthetic, surface treatment with antiseptic solutions;
- incision of the mucosa, gaining access to the cortical plate;
- retracting the flap, making cuts with a fissure bur;
- breaking the bone, drilling holes for installing the structure;
- insertion of the rod, filling the remaining space with a bone substitute;
- tightening screws;
- installation of a bioresorbable pad to isolate the area;
- suturing the wound.
Engraftment, risks of complications
Integration of the structure occurs 14-16 weeks after installation. This time is enough for penetration into the tissue, formation of a full-fledged structure, and healing after the intervention. After just three to four months, the installation of an expander, abutment and crown is allowed.
The duration of such a rehabilitation period depends on many factors, including:
- age, health and tissue status of the Patient;
- professionalism of the dentist, compliance with the installation protocol;
- bone density;
- compliance with personal hygiene rules.
Complications rarely develop; signs are usually observed on the second to fourth day. You can exclude them by strictly following your doctor’s recommendations. Possible risks include:
- divergence of applied sutures under mechanical loads of the operated area;
- inflammatory processes, increased pain, redness of tissues;
- peri-implantitis, which develops in the absence of proper oral care.
If any problems occur during the engraftment stage, you should immediately consult a doctor. If this is not done, the situation may worsen, leading to the loss of the installed implant and serious tissue damage.
Types of bone grafting
Depending on what material will be used for transplantation, there are three types of bone grafting: • Autoplasty – using the patient’s own bone. Bone material for this purpose is taken during a separate operation, for example, from the jaw in the area of the eighth teeth, or from the thigh. This option is quite traumatic, but at the same time guarantees better survival rate; • Xenoplasty – the use of carefully processed animal bones, mainly cattle. This method is now almost never used; • Alloplasty is the use of special synthetic materials that not only replace human bone tissue, but also stimulate its growth by creating a frame. The method is convenient and non-traumatic, widely used and loved by many dentists and patients. It is facilitated by a wide selection of modern osteoplastic materials with good properties and a high percentage of engraftment. These methods do not have any fundamental differences, and the choice of bone material does not affect the course of the operation. But in certain clinical cases it has a significant impact on the result of bone grafting.
Use of biomaterials
As I wrote above, with osteotomy, technically, we can do without biomaterials at all.
But, as practice shows, it’s easier with them. And, if you really want to push something into the patient, and the patient is ready to pay for this pushing, then you will most likely need:
– barrier membrane. In this case, it will play an exclusively insulating function, which means that you should not bother with its properties. There is also no need to fix the barrier membrane, since the frame of the defect is the displaced bone defect and installed metal structures.
Anticipating the question, I will answer that in our clinic for such purposes we use a Geistlich Bio-Gide barrier membrane of dimensions 16x22 or 25x25 mm. The latter turns out to be even too much - sometimes we divide it and lay it in two layers. But this is not important.
– graft. We mainly use xenografts. The ideal xenograft for such purposes is one that comes in the form of a solid cube, which itself will serve as a support for the displaced bone fragment. For example, such as Geistlich Bio-Oss Collagen. It is easy to process, place and hold the displaced bone fragment, but there is a fly in the ointment here - for large defects, even a large (250 mg) package of Bio-Oss Collagen is not enough.
Bio-Oss Block would probably be good in such cases, but its fitting and processing presents certain difficulties. Besides, as far as I know, it has been discontinued.
So, perhaps, to fill the “box” resulting from osteotomy, it is worth considering other, more suitable grafts from other manufacturers.
We use regular Bio-Oss 0.5 g. Its volume (1.5 cubic cm) is quite enough even for an end defect the size of several teeth.
Patient reviews
In general, on the Internet on forums, patients speak positively about this operation, especially if it is performed on the upper jaw. After it, recovery is faster, especially when compared with grafting a bone block. A problem such as shifting of the installed bone material is much less common, that is, complications arise less often. Swelling and pain also go away very quickly. Patients are especially pleased that implants can be placed immediately during surgery, and not some time after bone grafting.
Most often, bone deficiency is observed on the vestibular side of the alveolar process. Many authors have proposed their own classifications of alveolar ridge defects, including Allen et al, Seibert, Cawood and Howell, Studer, and others.
In accordance with the classification of Wang and Shammeri, defects of the alveolar process are distinguished by height, thickness and combined. Splitting of the alveolar process is recommended for thickness and combined defects.
It is generally accepted that bone augmentation techniques are less predictable and cause a higher percentage of complications than isolated implant treatment.
Today, methods for reconstructing the alveolar process are available using:
titanium mesh or foil;
· resorbable or non-resorbable membranes;
· titanium modules or screws for osteosynthesis;
· bone materials (autogenous, allogeneic, xenogeneic blocks);
· 3D-techniques; splitting of the alveolar process and their combinations.
The success rate of different techniques varies. For example, the effectiveness of GBR varies between 85 - 98%, while the newly formed bone tissue, from the point of view of implantation, turns out to be as close as possible to natural bone.
However, this technique requires much more time. One of its complications is membrane exposure, which can cause loss of the implant and bone in the intervention area.
Autotransplantation of bone blocks in the form of inlays or onlays, according to various sources, ranges from 60% to 93%. However, all publications note a high risk of resorption of autogenous bone grafts and a long healing period.
Technique using bone materials for splitting the alveolar process
It is known that it is more difficult to achieve success in restoring the alveolar process after vertical atrophy than horizontal atrophy. To eliminate the consequences of horizontal atrophy, you can use the technique of splitting the alveolar process.
The classic surgical protocol is as follows:
· Incision of the mucosa, submucosa and periosteum behind the grafting line; making releasing incisions.
· Peeling of the mucoperiosteal flap.
· Performing bone cuts along the apex of the alveolar process and vestibular surface within the compact lamina.
· Expansion of the bone using any of the available methods.
· Introduction of bone material.
· Stitching.
This technique was proposed in the early 90s of the last century. Despite the wide possibilities of clinical application, the intervention has a number of disadvantages:
· Narrow range of conditions for carrying out.
· Possibility of longitudinal jaw fracture.
· Excellent manual skills required.
· Greater discomfort experienced by the patient during the operation.
· Limited volume of augmentation replanting.
· Limitation of use within individual dentition defects.
Of course, to perform splitting of the alveolar process, certain conditions must be met, otherwise this technique cannot be successfully implemented.
Conditions for splitting the alveolar process:
· The width of the top of the ridge should be about 3 - 6 mm.
· The alveolar ridge is narrow in the coronal part and wide in the apical part.
· The alveolar process must have a spongy part.
· Possibility of fixing at least 1/3 of the implant apical to the splitting zone.
· Possibility of installing an implant of sufficient length.
· Possibility of covering with soft tissues.
Many modifications of the alveolar process splitting technique have been proposed. In 1994, Summers proposed a technique for splitting the alveolar process with osteotomes.
Many surgeons use a combined flap (incomplete-complete-incomplete) to split the alveolar process. That is, the periosteum is peeled off only in the area of the future cut. This makes it possible to maintain trophism, flexibility and elasticity of bone tissue, as well as prevent excessive resorption and traumatic fracture.
When constructing the flap, Dehasjuk et al do not recommend releasing incisions.
Here are several methods for expanding the alveolar ridge:
· Expansion with osteotomes (as a rule, pointed conical osteotomes are used according to the Summers method).
· Expansion with an implant (special implants are used for this, which are used only for the splitting technique).
· Expansion with osteotomes and an implant, or a combined technique (the so-called expansion with closed sinus lift).
The technique discussed below will use expansion of the alveolar bone using a chisel. This technique makes it possible to easily, without special manual skills, expand the alveolar process. Its disadvantage is the significant discomfort experienced by the patient during the operation.
A free gingival or connective tissue graft can be used to provide adequate soft tissue coverage.
Some authors believe that transplantation of a graft before osteoplastic interventions is inappropriate, since after augmentation the number of attached keratinized gums will significantly decrease and transplantation will not make sense. In addition, a break of at least 3 months is needed after soft tissue transplantation for maturation before osteoplastic measures.
On the other hand, soft tissue grafting is appropriate when soft tissue augmentation is necessary to adequately cover the augmented area.
Another argument in favor of autotransplantation of soft tissues in the area of clefting of the alveolar process is the need to convert a thin periodontal biotype into a thick one to form an aesthetic contour and imitate gingival papillae at the second stage.
So, let's consider each stage of treatment and the role of bone materials in the splitting of the alveolar process in combination with transplantation of free flaps.
First surgical stage
In the edentulous area within the attached keratinized gum, an incision is made with an offset towards the tongue in the lower jaw and the palate in the upper jaw. In this case, the incision in the lower jaw is shifted so that approximately 2 mm of keratinized gum remains on the tongue side.
On the upper jaw, the incision is shifted towards the palate, according to anatomical conditions. On the vestibular side, instead of releasing incisions, incisions are made around the necks of natural teeth. As a rule, the vestibule of the oral cavity deepens in the area of intervention.
To preserve the blood supply to the vestibular cortical plate, the bony crest is preferably left covered by periosteum. To separate the vestibular and lingual parts of the alveolar process, the cut is carried out with a surgical bur. Splitting is performed with straight or angled tips.
The limit to the degree of separation of the bone plates is the elasticity of the bone crest and the diameter of the implant that is planned to be installed.
After expansion is completed, the bed is prepared for implants using cutters with diameters that are selected in accordance with the manufacturer’s protocol.
Implants are installed manually. Bone material in the form of a gel is injected into the splitting site. The insufficient amount of soft tissue in the upper jaw can be compensated with local tissues (apical displacement of the flap), in the lower jaw - with free gingival or connective tissue flaps.
The proposed protocol provides for a two-stage installation of implants. If premature spontaneous opening of the implant occurs, a gum former is installed, the height of which depends on the formed volume of soft tissue.
The sutures are applied with silk and polyamide, and the graft itself is fixed with materials based on polyglycolic acid.
Examination of the patient and removal of sutures are planned 5-7 days after surgery. In the postoperative period, patients can optionally have permanent adhesive structures made.
Second surgical stage
To control integration before the second stage, the following indicators are assessed:
· Patient complaints.
· X-ray data.
· Stability of the implant at the time of deployment, etc.
The second surgical stage is recommended to begin at the following times: on the lower jaw after 10 weeks, on the upper jaw - after 14 weeks. As a rule, during healing in all cases it is possible to achieve an increase in the width of the alveolar process and the amount of attached keratinized gum.
Exposure is carried out using various methods, depending on the clinical situation and the need to form an aesthetic contour or imitate gingival papillae.
Orthopedic stage of treatment
In accordance with the described method, the orthopedic stage begins 23 weeks after opening the implants. For prosthetics, you can use both individual zirconium oxide abutments and factory-made abutments.
The choice of abutments is determined by the characteristics of the orthopedic design (metal-ceramic or all-ceramic), the height of the smile and aesthetic requirements, as well as the wishes of the patient.
Conclusions and recommendations
According to Dehasjuk and a number of other authors, this augmentation technique and the use of bone materials for splitting the alveolar process have many advantages.
Firstly, this technique is less traumatic compared to others used for lateral augmentation. The easy postoperative period and the absence of an additional surgical area for autologous bone collection make it possible to widely use this technique.
Secondly, there is the possibility of combining the technique with the installation of dental implants in one stage. Its use almost always provides high levels of primary stability and allows the use of an early loading protocol.
Thirdly, due to the absence of the need for the use of additional means, the cost of the operation is significantly reduced and, as a rule, surgery is not required to remove membranes, meshes, screws and the like.
The fourth advantage is the fact that bone grafting is carried out into a three-walled (according to some classifications, four-walled) defect with a high osteogenic potential. This promotes rapid replacement of the material with bone tissue.
The healing period when using the above-described treatment method is much shorter than with other reconstructive methods, and is about 2-4 months.
By splitting the alveolar process, the vestibular fragment is significantly displaced, thereby partially or completely compensating for the unaesthetic contour that is formed due to bone resorption.
Loss of an implant when using this technique is considered a fairly rare occurrence, which is usually observed in the reparative phase. And even after disintegration, the resulting volume of bone tissue remains to a large extent.
Possible complications
Of course, after the intervention, swelling and pain appear, but they quickly pass and are easily relieved with pharmaceutical painkillers. Also, if too much stress is placed on the surgical area, the stitches may come apart, but the dentist can quickly fix this problem. But still, we do not recommend putting too much stress on the operated area for several months. It’s better to give up food that needs to be chewed hard and for a long time, don’t crack seeds and don’t try to use your teeth as a bottle opener - then there won’t be any problems. Well, be sure to maintain oral hygiene to prevent infection and inflammation.
Contraindications
Let's just say that I would seriously think about it and, perhaps, would prefer a different method of osteoplastic surgery if:
– we are dealing with atrophy in both the height and width of the alveolar ridge,
– we work with bone tissue biotype I or II,
– there is “no more bone tissue left.” Well, really waaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaay up
– all that we have from the equipment of the surgical office is a rusty tip made in China.
For example, in this case:
I would be pissing to do an osteotomy, I would prefer another method of osteoplasty
Contraindications for bone splitting surgery
- The presence of foci of acute inflammatory diseases in the oral cavity;
- General acute and chronic diseases;
- Weakened immunity, immunodeficiency;
- Oncological diseases, especially in the oral cavity;
- Osteoporosis;
- Age over 50 years – a particularly thorough examination is required;
- Pregnancy and breastfeeding;
- Blood diseases, especially blood incoagulability;
- Mental illnesses in which the patient cannot behave adequately in the dentist's chair and during rehabilitation.
If there are complications, we recommend either eliminating them or choosing another method of prosthetics - for example, installing removable dentures.
Advantages and disadvantages
The use of this technique is not always permitted; the list of indications is limited:
- severe bone deficiency was diagnosed at the repair site;
- there is ridge resorption.
In addition, the following requirements must be met:
- the height of the bone at the installation site should not be less than ten millimeters;
- alveolar width – from 0.2 millimeters;
- Bone density is average or higher.
There are many more contraindications, these include:
- allergic reactions to drugs used for pain relief;
- infectious lesions, inflammatory processes at different stages;
- exacerbation of chronic diseases;
- disorders of hematopoiesis, blood clotting;
- endocrine system problems;
- pregnancy;
- tuberculosis;
- negative condition of the oral cavity;
- caries and other diseases.