Alveoloplasty methods
Correction of the alveolar process
It is used before the start of rational prosthetics, for the convenience of the patient while wearing a removable denture.
Relocation of the inferior alveolar nerve
The operation is performed when there is not enough space to place an implant; this situation often occurs in the lower jaw.
Graft transplant
Transplantation - increasing the volume of the mucous membrane or bone tissue. The need for this method arises after the removal of teeth or anatomical features of the body in order to comply with the conditions for implantation.
Gingivosteoplasty
This method is used for periodontal diseases with varying degrees of severity. Gingivosteoplasty is intended to correct gum recession.
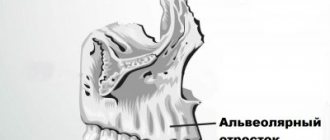
Alveolar process atrophy
Rice. 1a
Rice. 1b
Rice. 1c
Rice. 2a
Rice. 2b
Rice. 2c
Rice. 2d
Rice. 3a
Rice. 3b
Rice. 3c
Rice. 3d
Rice. 3e
Rice. 4a
Rice. 4b
Rice. 4c
Rice. 5a
Rice. 5b
Rice. 5c
Rice. 5d
Rice. 6a
Rice. 6b
Rice. 6s
Rice. 7
Loss of bone tissue in the alveolar processes of the jaws often occurs due to the loss of teeth, as well as their primary absence. Bone tissue deficiency accompanies chronic forms of periodontitis, which may be a consequence of internal pathology of the body. This condition causes cosmetic disturbances, often complicates full dental prosthetics, and in some cases makes it impossible to install dental implants. Elimination of atrophy of the alveolar processes of the jaws (restoration of lost structures) is possible through transplantation (grafting) of bone tissue borrowed from other parts of the body. The use of artificial drugs produced by the domestic and foreign medical industry, such as kollapan, collaost, bioss, etc., is ineffective, since they do not contain a single living osteogenic cell. As you know, the bone tissue of the jaw bones consists of a compact and spongy part. They include bone cells (osteocytes, osteoblasts, etc.) and intercellular substance, due to which the strength properties necessary to withstand the chewing load without traumatic damage are determined (in the molar zone an average of 60-80 kg, in the incisor zone - 30- 40 kg), and spongy substance and bone marrow cells. Bone tissue is richly supplied with blood, since osteocytes die within 2 hours if they are located further than 0.2 mm from a blood vessel. Metabolic processes constantly occur in its thickness, ensuring its trophism (nutrition) and the constancy of the internal environment, as well as processes of bone remodeling (atrophy and replacement of non-viable tissue, including restructuring of the structure depending on changes in load (direction and force). Based on the above, it becomes It is clear that the above drugs are not fully able to replace missing bone structures. After they are placed in the body, they undergo resorption, and the body is forced to direct its energy to get rid of resorption products. These processes not only require large energy costs (due to which patients after such type of operations, they complain for a long time of general weakness and malaise), but also subject to resorption of the bone tissue surrounding the implant used, which inevitably leads to even greater loss. Foreign bone tissue (allogeneic, cattle, etc.) after placement in bone defects is rejected or resorbed (dissolves), since it does not contain viable bone structures, and therefore it is impossible to achieve the desired result. The most effective method of restoring the lost structures of the alveolar parts of the jaw bones (used in our clinic) is the transplantation of osteogenic tissue (immature bone tissue) grown in the thickness of the patient’s iliac crest. This technology does not have the above disadvantages, since the transformation of transplanted tissue in defects is possible only into bone structures. It was established experimentally, clinically and radiologically that the transplanted osteogenic tissue in bone defects was rebuilt to the formation of an organotypic regenerate. This transplant material, due to its inductive properties due to the high content of low-differentiated bone elements of mesenchymal origin, as well as the properties of diffuse nutrition, anaerobic glycolysis, resistance to hypoxia conditions, appositional and interstitial growth, was not resorbed in defects and its cells actively participated in the processes of reparative osteogenesis .
Bone atrophy - what is it?
Bone atrophy is the process of a gradual decrease in the hard tissue of the jaw bone, while the size of the alveolar ridge is significantly reduced, pronounced nasolabial folds appear, the jaw decreases in size, and a “drooping” of the face occurs. Bone resorption (loss) occurs most often after surgical removal of the root, but a person can be born with this pathology.
Clinical case: a person’s tooth and root were removed a long time ago, and an implant and prosthesis were not installed in their place. Over the course of a year, bone tissue atrophies by approximately 25%.
Dentistry for those who love to smile
+7
Make an appointment
Causes
In addition to mechanical trauma from an impact, the cause of a fracture of the alveolar bone may be some disease that disrupts the normal state of bone tissue:
- osteomyelitis - inflammation of bone tissue;
- fibrous osteitis, characterized by bone dystrophy, thinning of the bone structure;
- various cysts and neoplasms that cause bone degeneration.
If the patient has the above diseases, even a slight impact on the bone can lead to a fracture of the alveolar process.
In children aged 5 to 7 years, that is, at the stage of growth of permanent teeth, trauma to the alveolar process can also be diagnosed due to the presence of follicles of permanent teeth in the bone, which subsequently disappear.
Material and methods
In the period from 2016 to 2022, 18 patients aged from 6 to 60 years with a current diagnosis of a defect of the hard palate and/or alveolar process and oronasal anastomosis were operated on in the Department of Reconstructive, Plastic Maxillofacial Surgery of the Federal State Budgetary Institution "Central Research Institute of IIS and Maxillofacial Surgery", Surgical treatment was performed to cover the defect and oronasal anastomosis with a FAMM flap.
Most patients have a history of multiple operations for the underlying disease in the scope of primary uranoplasty, reuranoplasty, the number of previously undergone surgical interventions on the palate in this group of patients ranges from 1 to 8-10, and yet in all cases there was a recurrent residual defect coupled with cicatricial -changed surrounding tissues due to repeated surgical interventions, inflammatory and necrotic processes. The size of the defect from 3 to 40 mm, the need to separate two anatomical zones - the oral and nasal cavity / maxillary sinus, as well as the presence of a persistent inflammatory process in the nasal cavity / maxillary sinus dictated the need to bring in a sufficient amount of well-supplied tissue from another anatomical area.
The psychological and emotional state of these patients makes it a priority to choose a traumatic surgical intervention, without serious donor damage, an optimal surgical intervention in terms of time, with a minimization of the rehabilitation period associated with lower risks in case of failure.
At the first stage of treatment of such patients, the primary task is the reliable and effective elimination of the oronasal anastomosis with a soft tissue flap; in the future, patients are planned to undergo bone reconstruction followed by dentofacial rehabilitation.
In all 18 cases, to plan a flap in the projection of the facial artery, as an instrumental method of research, patients underwent duplex ultrasound scanning of facial vessels with determination of qualitative and quantitative characteristics of the facial arteries, which in 100% of cases helped to determine the localization of the facial artery in a typical place, as well as to register a satisfactory blood flow speed and vessel diameter.
In cases of extensive bilateral defects, CT angiography of the vessels of the face and neck was performed to visualize the bone edges and determine the true size of the defect, which is the most reliable method of preoperative diagnosis and precision flap planning.