From this article you will learn:
- what does tartar look like - photo of dental deposits,
- reasons for education,
- how to remove stones from teeth.
The article was written by a dentist with more than 19 years of experience.
Tartar is completely or partially hardened soft microbial plaque that has not been completely removed through oral hygiene procedures. Tartar contains a large number of pathogenic bacteria, food residues, and calcium salts. The rate of tartar formation varies from person to person and depends not only on the quality of oral hygiene, but also on the characteristics of the diet, the composition and rate of saliva secretion, and other factors.
Stones on teeth can be supra-gingival or sub-gingival. The first ones are clearly visible and are located in the area of the necks of the teeth (Fig. 1-6). They usually have a dark or yellowish-brown tint. In the presence of tartar, patients always complain of accompanying symptoms - bleeding gums, bad breath, as well as swelling, redness or cyanosis of the gingival margin. And in the presence of subgingival dental deposits, in some cases it also affects tooth mobility and purulent discharge from under the gums.
Tartar: photo
Teeth stones consist of organic (10 to 30%) and inorganic (70 to 90%) components. The bulk of inorganic components are calcium salts - primarily calcium phosphate crystals. The organic components include: microorganisms, leukocytes, protein-polysaccharide components, epithelial cells exfoliated from the surface of the mucosa, amino acids, etc. It should be noted that the composition of tartar is not constant, and over time the proportion of organic components decreases.
How do stones form on teeth?
The main factor in the formation of tartar is certainly the presence of soft microbial plaque on the teeth. Its formation begins within 1-2 hours after brushing your teeth, and this process is accelerated many times over in the presence of food residues in the oral cavity (if you did not brush your teeth immediately after eating). In parallel with the increase in the amount of dental plaque, its mineralization also occurs, i.e. it begins to become saturated with calcium salts contained in saliva. Partial mineralization of plaque occurs on average within 10-16 hours from the moment of its appearance.
Thus, if your oral hygiene is poor, it only takes 1-2 days for a thin layer of partially mineralized plaque to form on your teeth. It will be firmly attached to the surface of the teeth, and it will no longer be possible to remove it with a toothbrush and toothpaste. In places where partially mineralized plaque is deposited, the tooth enamel becomes rough, which facilitates the rapid attachment of new portions of plaque and its mineralization. This is how tartar forms.
Looking at the photo above (Fig. 1-6), please note that the formation of tartar occurs primarily in the area of the necks of the teeth, i.e. exactly in those places where soft plaque accumulates after eating. The second favorite location is periodontal pockets (also called periodontal pockets). The formation of such pockets occurs during periodontitis.
Factors contributing to the formation of tartar:
The rate at which tartar forms varies from person to person. In addition to the obligatory presence of soft plaque, a number of other factors can also affect the rate of formation of tartar (but they are only predisposing). Such factors include –
- the predominance of soft, overly processed foods in the diet, as well as a large amount of easily digestible carbohydrates,
- frequent snacking between meals, followed by poor oral hygiene,
- smoking,
- increased salivation,
- changes in the volume of secretion and chemical composition of the gingival fluid (occurs when the patient has gum inflammation - gingivitis or periodontitis),
- and, of course, poor/irregular oral hygiene, refusal to use dental floss to clean interdental spaces, use of low-quality hygiene products for hygiene (for example, old brushes with fluffy bristles), etc.
Causes of enamel hyperesthesia
Many patients complain of increased sensitivity of teeth after tartar removal. The main reason for such complaints is the exposure of hard tooth tissues that were previously covered with tartar. The deposits partially reduced the impact of irritants - high and low temperatures, sour, sweet and spicy foods. Therefore, after the stone is removed, the enamel reacts more sharply to external factors.
Increased tooth sensitivity is caused by:
- existing diseases of the oral cavity - caries, pulpitis,
- thinning of tooth enamel in the cervical area,
- non-compliance with professional cleaning rules.
To reduce the likelihood of enamel hyperesthesia, have your teeth cleaned only by qualified dentists. Contact only experienced specialists in whose professionalism you are confident.
Teeth stones are of the following types:
Stones on teeth (synonym - hard dental deposits) are usually divided into supragingival and subgingival.
- Supragingival calculus on the teeth (Fig. 1-6) – visible to the naked eye when examining the teeth, because always localized above the gum level. It may be dark or yellowish in color. A stone of such localization is not difficult to remove, which is usually carried out using ultrasound (however, very small dental plaque can also be removed using the Air-flow procedure).
- Subgingival stones on teeth (Fig. 7) are localized below the gum level, and therefore they are not visible during a normal visual examination of the teeth. However, in places where subgingival dental deposits are present, the gums usually have a bluish appearance, they are swollen and bleed easily. Also, sometimes when you press on the gum in these areas, a scanty purulent discharge may be released from under it. In the photo below you can see subgingival tartar, localized in a deep periodontal pocket.
Please note that the appearance of pink gums in the photo is completely normal. But after the gums peel off, we see a small amount of tartar and a large amount of destroyed bone around it. This picture is quite common for patients with periodontitis. Finding such stones is quite difficult. Firstly, a panoramic photograph of the teeth can help the dentist with this, because it will show the level of bone tissue around the teeth (the presence of such “bone pockets”).
If there are such pockets in the image, we immediately assume the presence of subgingival tartar in this area. The second method of detecting subgingival dental plaque is associated with the use of dental instruments. For this purpose, an air “gun” is usually used, which every dental unit has. The air flow from it moves the gum away from the root of the tooth, due to which the contents of the periodontal pockets become visible to a certain depth.
Types - place of formation and color
In dentistry, there are two types of tartar - supragingival and subgingival. They are distinguished by their location on the surface of the tooth. The first is visible to the naked eye and has a grayish or whitish-yellow color. It is easily removed by scraping. Minerals coming from saliva participate in the formation of supragingival tartar. It is most often localized in the area of the lower front teeth and the buccal surfaces of the maxillary molars, where the ducts of the salivary glands open.
Subgingival tartar can only be detected by a dentist during probing. It is formed due to minerals coming mainly from the gingival fluid. As a rule, it is dark brown in color with a greenish tint, localized on the neck of the tooth within the gingival groove, on the root cement, in the periodontal pocket. Covering the neck of the tooth, the stone is tightly attached to its surface, and often forms protrusions.
Tartar and oral hygiene –
After eating, a large amount of food debris remains in the mouth (primarily in the interdental spaces), and they cannot be removed by rinsing or chewing gum alone. For their vital activity, bacteria primarily use easily digestible carbohydrates, which are found in sweet and flour products. It has been established that in the absence of proper hygiene for only 1 day, the amount of bacterial plaque in the oral cavity increases at least 2 times.
But bacteria use nutrients not only for reproduction, but also for the production of special enzymes (enzymes), which allow bacteria to firmly attach to the surface of the tooth (24stoma.ru). In the absence of proper hygiene, individual pinpoint bacterial colonies attached to the teeth merge, forming a significant mass of bacterial plaque (Fig. 8-9). At this stage, plaque is still soft and can be removed with a regular toothbrush.
Accumulations of soft microbial plaque –
Next, there will be a gradual mineralization of soft microbial plaque, which will eventually turn into hard tartar. Mineralization (calcification) of soft dental plaque occurs through the deposition of proteins and calcium salts contained in saliva on the surface of bacterial colonies. The mineralization process occurs in combination with the layering of new bacterial colonies.
In parallel, microbial plaque releases toxins and inflammatory mediators, which trigger inflammatory phenomena in the gums. The main signs of gum inflammation are –
- bleeding when brushing teeth,
- redness or bluishness of the gums,
- pain in the gums,
- in later stages - suppuration from periodontal pockets, tooth mobility.
Pathogenic bacteria are very cunning, and gum inflammation is vital for them. The fact is that in the place where the gums adhere to the tooth there is a so-called periodontal groove, into which periodontal fluid is constantly produced from the gums in small quantities. This liquid contains a large amount of salts and proteins necessary for bacteria to quickly grow colonies. The launch of inflammation processes in the gums leads to a sharp increase in the production of periodontal fluid, and as a result, microbial colonies receive even more proteins and salts necessary for the calcification of tartar.
Caries - what is it?
More than 95% of the inhabitants of our planet face the disease. Thus, it can be called the most common dental problem. At the very beginning, the pathological process affects only the enamel, and in the absence of therapy it penetrates into the deep hard layers. Then the soft tissues with nerve fibers and blood vessels become inflamed.
The disease is insidious because in the earliest stages it does not manifest itself in any way, and the patient begins to sound the alarm only when acute pain and a large hole appear that cannot be eliminated by conservative methods.
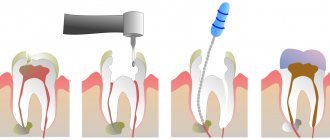
Tartar: removal
When you brush your teeth, you can only remove soft plaque from the surface of your teeth. Partially mineralized plaque, as well as hard dental deposits, can no longer be removed by regular teeth cleaning at home. And in this case, only a dentist can clean the tartar.
1) Cleaning the stone at the dentist’s appointment –
The traditional way to remove hard plaque is ultrasonic teeth cleaning. In this case, stone removal is carried out using an ultrasonic scaler. Removing supragingival calculus is a very simple procedure, and 1 hour is enough to remove calculus from all teeth. But to effectively remove subgingival stones, you need several visits and a highly qualified doctor. Therefore, it is best to remove stones not from ordinary dental therapists, but from periodontists (these are dentists who specialize in the treatment of gum inflammation).
Ultrasonic tartar removal –
There is also the “AirFlow” procedure, with which you can remove small dental deposits, pigment plaque, and polish your teeth. In this case, cleaning and polishing of teeth occurs due to a water-air mixture containing granules of an abrasive substance, sprayed under high pressure from a special tip. But AirFlow will not be effective against massive hard dental plaque, which in any case will first have to be removed with ultrasound.
Tartars: photos before and after their removal
On average, the price for tartar removal is about 100-150 rubles per 1 tooth, including polishing.
2) How to remove tartar at home –
Some patients use recipes for removing plaque, which are replete with many unprofessional websites, promising complete relief from tartar. We'll disappoint you, but these methods not only don't work, but also cause harm to tooth enamel and gums. Just for fun, you can check them out at the link above.
It is impossible to remove well-mineralized tartar and dense pigment plaque with any home remedies. However, not too pronounced pigment plaque and only partially mineralized plaque can still be removed with the help of the following modern dental care products. First of all, we are talking about Oral-B electric toothbrushes - in combination with special highly abrasive toothpastes.
Important: Oral-b electric brushes have a round head with bristles that performs 8,800 reciprocating movements per minute, as well as a minimum of 20,000 pulsating movements. Pulsations help loosen dense plaque (even that which may already be partially mineralized), and rotational movements sweep it away and polish the teeth. This brush is a miniature dentist’s tool and is probably familiar to everyone who has gone to the dentist for professional oral hygiene.
The second component is highly abrasive toothpastes, which can help remove pigmented and partially mineralized plaque. They can only be used once a week. If you are using them in combination with an Oral-b electric brush, it is advisable to use the electric brush only at low speed (in the “whitening/polishing” mode). You can find out how this is done correctly and what toothpastes are used at the link below.
You can also purchase professional teeth polishing products, which the dentist uses to finish polishing teeth after ultrasonic cleaning (they are sold in stores that sell consumables for dental clinics). For example, pastes such as “Detartrine” or “Detartrine – Z” (this one is more effective). They are able to remove even small tartar and not too pronounced smoker’s plaque. Used in combination with an Oral-B electric toothbrush (rotation of the nozzle should be at low speed).
→ Scheme for removing dental plaque at home
Prevention of tartar –
Prevention is, first of all, high-quality and regular oral hygiene, no snacking between meals, and regular use of dental floss. You can read about proper hygiene in the link above. In this article you will find the most detailed description of what proper oral hygiene should be. But we would also like to tell you about what else can help you in the fight against pigmented plaque and dental plaque.
1) Use toothpastes containing pyrophosphates, because... this component prevents the mineralization of dental plaque. Pyrophosphates in toothpastes will not be able to dissolve existing tartar, but they are good at preventing its appearance.
2) Use electric toothbrushes for hygiene. They are at least 2 times more effective at removing plaque compared to regular manual toothbrushes. In addition, the pulsating movements of the Oral-B electric brush heads allow you to loosen tightly attached plaque, and the rotating movements sweep it away from the teeth. But if you have periodontitis, then it is better to use Philips Sonicare sonic brushes rather than Oral-B brushes.
What do dental stones lead to?
- Halitosis (bad breath) – bacteria that are part of dental plaque produce sulfurous substances that have an unpleasant odor. You can try to mask it with special sprays, chewing gums and perfumed rinses, or remove the source of its occurrence (i.e. tartar and plaque).
- Inflammation of the gums (gingivitis and periodontitis) – inflammation of the gums is of an infectious nature.
Microbial plaque and tartar release toxins and inflammatory mediators, which trigger the process of inflammation in the gums. Inflammation is first characterized by swelling and redness of the gums, bleeding, pain when brushing teeth - these symptoms are characteristic of gingivitis. If gingivitis is not treated on time, the inflammation affects not only the marginal gum, but also the bone tissue, and also leads to the destruction of the periodontal attachment. As a result, gingivitis turns into periodontitis. The latter (in addition to the preservation of all the symptoms of gingivitis) is characterized by the development of tooth mobility, suppuration from periodontal pockets, bone atrophy and exposure of tooth roots... - Caries - you need to remember that cariogenic microorganisms that are part of soft and hard dental deposits release hydrochloric acid during the digestion of food residues. This acid destroys the tooth enamel at the point of contact, after which the defect is populated by microflora and the tooth begins to rot.
- Diseases of the oral mucosa - accumulations of dental plaque reduce the local immunity of the oral mucosa, which increases the risk of developing certain diseases of the mucous membrane. We are talking about the formation of erosions and ulcers, and even necrosis of areas of the mucosa. In general, the risk of developing herpetic and aphthous stomatitis in the presence of dental plaque always increases.
- Worsening of chronic diseases - cardiovascular, rheumatoid arthritis, diabetes, etc. This occurs due to the absorption of toxins released by microbial plaque into the blood. Toxins are carried through the bloodstream and affect the functions of all organs and systems.
Important:
remember that the worse your hygiene, the more often you need to visit the dentist for ultrasonic teeth cleaning. Patients with good hygiene are recommended to do this only once a year, with satisfactory hygiene – once every six months. If hygiene is poor - once every 3 months, or even once a month (everything is individual here). We hope you found this article helpful!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a periodontist, 3. National Library of Medicine (USA), 4. American Academy of Periodontology (USA), 5. “Therapeutic dentistry. Textbook" (Borovsky E.V.).