Why you can’t install removable and bridge dentures against the background of advanced periodontitis
Loss of bone tissue and widening of the sockets during periodontitis create a very ambiguous situation: on the one hand, long-term conservative treatment in the later stages is rarely effective, on the other hand, prosthetics are also difficult, and the problem of missing teeth needs to be solved. However, not every treatment method is suitable.
Why are dental bridges not suitable?
Teeth with periodontitis are weakened and are on the verge of falling out; it is strictly forbidden to use them as support for a denture. The bridge will be movable along with the teeth on which it is attached. The risks are high, even if complex and long-term treatment was carried out before.
Why are removable dentures not suitable?
In fact, after a course of treatment for periodontitis (or closer to the middle of it after acute inflammation has resolved), removable dentures can be installed to solve the problem of partial absence of teeth. But only for a short time, because... When used long-term, they lead to many problems:
- do not stop bone atrophy, but only aggravate this process,
- put increased pressure on the gums and can provoke inflammation, which is extremely undesirable during the course of therapy,
- will require regular correction, since during treatment the damaged tissues are restored, which means the level of the bone with the gum will change - the dentures will no longer fit tightly, will shift, dangle,
- if teeth are partially missing, there is nothing to attach them to - as in the case of bridges, it is better not to use living teeth for support, especially if they are mobile,
- if the teeth are removed scatteredly, then removable dentures will not work at all; the minimum segment is 2-3 missing teeth in a row.
That is, removable dentures can provoke the development of periodontitis and negate all the results of a course of complex treatment. In addition, they are difficult to get used to - more than half of patients are not satisfied with them either in aesthetics or functionality.
Stages of chronic periodontitis
Depending on the level of damage to periodontal tissues, doctors distinguish four stages of the disease.
- At the initial stage, the patient experiences only slight discomfort while eating and brushing teeth. Gingival swelling may be present and periodontal pockets do not exceed 2.6 mm.
- With mild chronic periodontitis, the structure of the gums gradually changes, bleeding appears, and periodontal grooves increase to 3.6 mm. The patient may experience pain when contacting the toothbrush. Due to the accumulation of pathogenic microorganisms, bad breath occurs.
- With moderate chronic periodontitis, the periodontal pockets deepen up to 0.5 cm. The bone begins to atrophy, the necks of the teeth are exposed, and the teeth themselves become sensitive and begin to wobble. At this stage, the installation of implants may be difficult and even contraindicated.
- In severe chronic periodontitis, the tooth root is only half covered by the alveolar bone. Periodontal depressions become even larger, there is constant bleeding of the gums and purulent discharge. Hygiene and eating are difficult, teeth are mobile and may fall out.
Is it possible to carry out implantation against the background of advanced periodontitis?
Implantation with preservation of living teeth in this form of the disease is extremely rare, but is not excluded. In general, this is assessed at the stage of primary diagnosis - the doctor will understand what results can be achieved with complex treatment, whether it makes sense to spend time and money on therapy, or whether it is better to immediately remove mobile teeth, replacing them with implants, thus stopping the inflammation process once and for all.
It is also important to understand the attitude of the patient himself - it is worth preserving your teeth if you are ready to fight for your natural teeth to the end, if you are ready for the fact that over the next year you will need to visit a periodontist at least once a month and undergo regular treatment, and after installing implants you will have to strengthen hygiene and similar courses will become commonplace for you.
Periodontitis is an infection. Do not follow the lead of those doctors who offer implantation without complex treatment. One-time cleaning, curettage or splinting is not enough; inflammation will progress, which means there is a high risk of it spreading to the tissue around the implant. Rejection in such a situation is guaranteed - you will lose money, time, nerves and will be forced to undergo implantation again, but 100% with the removal of living teeth and most likely with bone grafting, because its own is destroyed.
Thus, implantation for this form of periodontitis while preserving your teeth can be carried out subject to the following parameters:
- if there is something to save - if you only have 3-4 teeth left, there is no point in investing time and money,
- if, based on the diagnostic results, we understand that it will be possible to eliminate the disease during a period of stable remission and the risks of implantation will be minimized due to this,
- if you are ready for long-term treatment and follow all your doctor’s recommendations in the field of lifestyle changes, nutrition, and oral hygiene.
Kinds
In order to correctly prescribe treatment for chronic periodontitis, the doctor must accurately determine which areas of the periodontium are affected and how far the disease has progressed. Depending on this, experts divide periodontitis into localized (focal) and generalized (diffuse).
Localized periodontitis
characterized by inflammation of a small area of the gum and is often the result of external influences, such as trauma or tissue damage due to inaccurate dental intervention. Read more about localized periodontitis in the article.
Generalized periodontitis
affects large volumes of tissue (often both jaws at once) and almost always occurs in a chronic form.
Read more about the different types of periodontitis here.
Why do we most often recommend removing teeth with periodontitis?
Our natural teeth are a hotbed of inflammatory processes. They have a porous structure, so it is on them that all microbes, which have a destructive effect on periodontal tissue, first settle. If implants with an active surface are placed next to such teeth, even the most resistant ones, which contain chemical elements that promote the healing of bone cells (such as SLActive® from Straumann and TiUnit® or TiUltra® from Nobel Biocare), they will still are unable to cope with a massive attack from all sides and bone tissue atrophy. That is, by preserving our natural teeth, we risk losing all the results of implantation.
So if there are only a few teeth left, they are destroyed and affected by diseases, then there is no point in preserving them - it is much easier to carry out removal with simultaneous replacement with implants, after which it will be enough to carry out regular oral hygiene (on your own and with a dental hygienist) and actually forget about dental problems forever. After all, if there are no teeth, there is no inflammation.
We categorically do not recommend implantation on one jaw if there are foci of generalized periodontitis of a severe and acute stage on the second - even though there is no direct contact, it is still dangerous. Our body is a single whole, let alone the oral cavity. Pathogenic microorganisms will circulate along with saliva, so inflammation of the tissues around installed implants is only a matter of time. It is impossible to talk about any lifelong service in such a situation.
Features of the initial stage of treatment of patients with severe periodontitis
T. V. Zakirov Ph.D., Associate Professor, Department of Pediatric Dentistry and Orthodontics, USMU
Periodontitis is one of the diseases with mild symptoms in the initial stages of its development. Typically, the only symptom of mild periodontitis is bleeding gums when brushing your teeth. Over time, this symptom disappears, and the disease does not manifest itself for a long time.
By the time severe periodontitis develops, the patient accumulates a whole complex of problems in the form of a pronounced loss of supporting-retaining periodontal tissues, pathological mobility and displacement of teeth, endo-periodontal lesions develop, periodontally altered occlusion, and occlusion of the dentition is disturbed [2, 7].
The condition is aggravated by the presence of concomitant somatic diseases in patients. These patients usually turn to the doctor at the stage of severe exacerbation of the inflammatory process in the periodontium with the presence of symptoms such as suppuration from periodontal pockets, sometimes abscess formation, severe tooth mobility, bad breath, etc. (Fig. 1, 2).
rice. 1. Oral cavity of a 30-year-old female patient with exacerbation of severe periodontitis. rice. 2. OPTG of the same patient, pronounced resorption of alveolar bone tissue.
The further prognosis for the entire human dental system often depends on the correct tactics of the dentist at this first stage. Unfortunately, in clinical practice, the choice of a doctor often takes one of the marginal positions: either total removal of teeth with subsequent problems with prosthetics, or, conversely, preservation of teeth in the absence of periodontal treatment as such. The situation is aggravated by the fact that the treatment of such patients requires the participation of almost all dental specialists, and the severity of the existing problems requires highly qualified doctors. In most cases, the first stage involves superficial cleaning of dental plaque.
Often this manipulation is performed by a clinic hygienist with secondary medical education. It should be noted that in the case of severe periodontitis, such tactics are unacceptable, because it inevitably leads to low effectiveness of the treatment, increases the likelihood of local and general complications, and makes it difficult to plan a further set of treatment measures. Patients, not seeing a significant improvement in the condition of their gums, lose confidence in the team of specialists and refuse recommended treatment measures (Fig. 3, 4). Therefore, knowledge of the features of managing patients with severe inflammatory periodontal diseases plays an extremely important role both in achieving clinical success at the initial stage of treatment and in planning further comprehensive dental rehabilitation.
rice. 3. Persistence of gum inflammation 1 month after professional hygiene in another clinic, right view. rice. 4. Oral cavity of the same patient, left view.
The first stage of treatment for patients with periodontal diseases should begin with a detailed conversation. During this period, the doctor must receive comprehensive information about the patient’s health status, medications he is taking, dietary habits and oral hygiene. Particular attention is paid to allergic diseases, diseases of the blood system with impaired coagulation, the speed of wound healing (regeneration can be suppressed due to diabetes mellitus, taking cytostatics, immunosuppressants, hormones; the risk of jaw necrosis is sharply increased when taking medications from the group of bisphosphonates, etc.). Despite the banality of this stage, it must be remembered that only the most detailed informing the doctor about the patient’s health status will help in the future to prevent the occurrence of serious complications in the form of unexpected bleeding, suppuration or extensive necrosis of periodontal tissue (Fig. 5).
When examining the patient, a periodontal card is filled out with a detailed indication of the depth of the periodontal pockets, the degree of gum recession, tooth mobility, the degree of furcation damage, etc. Hygienic and periodontal indices are assessed, as well as, if possible, the gum bleeding index. It is better to photograph the patient’s oral cavity before treatment and at the stages of complex therapy. Considering the constant increase in the legal literacy of patients, the increasing number of cases of defending their rights in court and the high cost of dental treatment, this stage is of particular importance.
The fact is that patients and doctors evaluate some results of treatment of moderate periodontitis completely differently. If the doctor pays attention to a decrease in the depth of periodontal pockets, a decrease in gum swelling and a decrease in exudation, then for the patient the leading symptom after the treatment will be exposure of the roots, loosening of the teeth and increased sensitivity (Fig. 6, 7).
rice. 5. Necrosis of the gums after professional hygiene due to 10 years of taking methotrexate. rice. 6. View of the gums before treatment in severe aggressive periodontitis. rice. 7. Generalized gum recession 1 month after the first stage of treatment.
Naturally, these symptoms are assessed sharply negatively by patients, so the patient should be warned about their development in advance when signing informed consent. In this case, emphasis should be placed on the temporary nature of the changes that occur. Increased sensitivity gradually disappears, pathological mobility of teeth also decreases, and gingival papillae are fully or partially restored while maintaining the distance from the contact point to the alveolar ridge within 5-7 mm [8]. In severe periodontitis, these changes are irreversible, but the doctor must focus on their cause (advanced periodontitis and loss of a large amount of tissue as a result of a long-term inflammatory process in the periodontium), as well as on the possibility of completely eliminating or leveling these symptoms at subsequent stages of treatment (splinting teeth, restoration, etc.). In other words, forewarned means forearmed.
The actual treatment of a patient with severe periodontitis must begin with empirical antibiotic therapy. The pronounced stage of inflammatory periodontal disease is characterized by deep massive invasion of aggressive anaerobic bacteria not only into the tissue of the periodontal complex and other organs and tissues of the oral cavity (for example, periodontal pathogenic microorganisms are found in the folds of the tongue, tonsil crypts, epithelial cells of the mucous membrane), but also in remote regions of the human body. body (endocardium, atherosclerotic vascular plaques, etc.).
In addition, after professional hygiene in severe periodontitis, a fairly large number of microorganisms are released into the blood - the phenomenon of transient bacteremia occurs [3]. And if in most patients this is accompanied by a feeling of weakness, malaise and a slight increase in body temperature, then in patients at risk (prosthetic heart valves and joints, congenital or acquired endocardial defects, etc.) this can lead to such serious complications as bacterial endocarditis or even sepsis [4].
Therefore, only systemic antibiotic therapy will suppress the majority of pathogenic microbes in the biofilm on the root surface, significantly increase the effectiveness of treatment, improve the healing period after dental intervention, and prevent the occurrence of local and general complications [6].
The drugs of choice include antibiotics such as Tsifran ST (a combination of ciprofloxacin and tinidazole) 1 tablet. 2 times a day, amoxiclav (amoxicillin and clavulanic acid) 375 mg, 1 tablet. 3 times a day, doxycycline 100 mg 2 times a day. Usually, at the stage of exacerbation, it is enough to prescribe drugs for 5-7 days. For patients wary of antibiotic therapy, more modern once-daily medications can be recommended, such as sumamed (azithromycin) 500 mg for 3 days or avelox (moxifloxacin) 400 mg for 5 days. In this case, the minimum inhibitory concentration of the antibacterial drug will be maintained in the patient’s body for a week.
Antibiotic therapy should be started 1-2 days before professional oral hygiene. Key point: the main treatment of periodontal pockets, even if it is divided into several stages, should involve taking antibiotics. It is important to focus the patient’s attention on the need to take an antibiotic; to increase motivation, you can show him suppuration from the pockets by applying finger pressure to the gums.
Of course, antibiotic therapy is a serious medical intervention in the human body, so it must be carried out in compliance with all the basic requirements of chemotherapy, taking into account the patient’s health status, indications and contraindications, and under the constant supervision of a physician. To minimize the side effects of antibacterial drugs, it is necessary to prescribe in parallel the administration of eubiotics for 2 weeks (Linex, Bifiform, Acipol, etc.).
It is better to carry out the treatment of periodontal pockets in 2 visits, separately for the upper and lower jaws, although under certain conditions (small number of teeth, remote place of residence of the patient) all the work can be carried out in one visit. Before use, the patient should rinse the mouth with an antiseptic, for example 0.2% chlorhexidine, which will reduce the contamination of the bacterial aerosol generated when using ultrasonic devices.
A prerequisite for effective pocket work in the vast majority of patients is adequate pain relief. A priori, it is impossible to treat the root surfaces to the full depth when using topical anesthesia. To increase the effectiveness of anesthesia in the lateral areas of the lower jaw, anesthetic injections are carried out not in the area of the transitional fold, but in the area of the attached gum. This promotes better deposition of the anesthetic and its penetration through the cortical plate of the jaw.
Considering the number of injections, it is necessary to periodically replace the needle to reduce trauma and pain when puncturing the mucous membrane. In the case of particularly massive jaws and significant destruction of bone tissue in the area of the interdental septa, conduction anesthesia may be the method of choice.
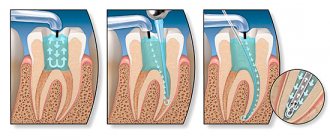
Treatment of periodontal pockets at the first stage of treatment of periodontitis should include not only the removal of dental plaque above and below the gum, but also smoothing the surface of the roots, correction of overhanging fillings in contact areas, removal of granulations, rinsing with antiseptics and, if necessary, in especially problem areas, should be completed by applying local antibacterial drugs in addition to systemic antibiotic therapy. It should be noted that, contrary to the opinion of many doctors, removal of deposits is not the only goal of this procedure. In case of aggressive periodontitis, for example, hard dental deposits may be completely absent, however, despite this, the pathological process is characterized by a highly pronounced destructive effect on periodontal tissue, rapid progression and low effectiveness of treatment [1].
There are often cases when patients undergo vector therapy 4 times a year, but this does not lead to any significant improvement in the condition, and sometimes (for example, with simultaneous orthodontic movement of teeth) it even ends catastrophically (Fig. 8, 9).
rice. 8. Severe inflammation of the gums with ineffective regular vector therapy. rice. 9. Progressive bone resorption as a result of orthodontic treatment.
A much more important goal of working in periodontal pockets is to remove a large amount of inflammatory granulation tissue, suppress the activity of periodontopathogenic microflora and shift the biocenosis of periodontal pockets towards less aggressive saprophytic species. It is necessary to begin work with ultrasonic devices, which remove the bulk of dental plaque. Without dwelling on the principles of operation of these devices, it should be noted that the treatment should be carried out to the entire depth of the periodontal pocket. In this case, partial separation of the granulation tissue occurs, and it is then easier to remove it with hand instruments. The mandatory set of tools when treating pockets includes not only ultrasonic devices, but also periodontal burs and curettes (Fig. 10, 11).
rice. 10. Burs for working in periodontal pockets. rice. 11. Comparison of the working parts of the scaler, universal curette and Gracie curette.
Without hand tools, periodontal pockets are not treated all over the world, although the choice of a specific set of tools remains at the discretion of the specialist [5]. The main characteristics of such instruments are a rounded, non-aggressive tip (for working in the subgingival area) and sharp working edges. Today there are enough opportunities for regular sharpening of curettes, which can be carried out both in specialized centers and independently in a dental clinic (Fig. 12, 13).
rice. 12. Device for sharpening periodontal curettes. rice. 13. Checking the sharpness of hand tools.
When working with hand instruments, involuntary dissection of the gingival papillae in the interdental area is possible. In most cases, this does not require suturing: in conditions where the mucoperiosteal flap is not peeled off, the papillae, after the end of the procedure and the onset of hemostasis, take their original position and the postoperative period proceeds without any complications. We also do not recommend applying periodontal dressings. In conditions of inflammation, they only interfere with the healing process - they compress the swollen gum tissue, impede the free evacuation of the contents of periodontal pockets, and again create conditions for the growth of anaerobic microflora.
Despite the fact that modern devices sometimes have built-in methods for detecting hard dental deposits, the best method for diagnosing them remains probing the root surface with a periodontal probe.
Elements of curettage require certain skills, and this procedure can be carried out by a doctor with a higher medical education, regardless of his profile - this can be done either by a therapist or dental surgeon specializing in the treatment of periodontal diseases, or by a periodontist at a clinic (let me remind you that the specialty There is no periodontist in Russia). Due to the increased invasiveness, it is unacceptable to entrust this treatment to a hygienist: this will not only be ineffective, but in some cases it is dangerous for the health and life of the patient.
The result of a correctly carried out first stage of periodontitis treatment is a significant improvement in the condition of periodontal tissues. Regardless of the severity of the disease, the gums acquire a pale pink color, active exudation and suppuration from periodontal pockets stop, tooth mobility decreases, and bad breath disappears (Fig. 14, 15).
rice. 14. Severe periodontitis in the acute stage in a patient. rice. 15. View 1 month after the initial stage of treatment, relief of inflammation.
Patients usually note an improvement in their condition. It should be noted that sometimes, with particularly deep periodontal pockets and severe bleeding gums, it is not possible to carry out full treatment in one visit. In this case, the remnants of dental plaque and granulations can be removed after 3-4 weeks under conditions of better visibility, after the inflammatory phenomena have subsided. The only condition is that it is necessary to timely assess the severity of the disease, the amount of deposits on the teeth and warn the patient about the need for a two-stage procedure.
After a month, you can take repeated photographs of the oral cavity and gather a consultation of specialists to develop a further treatment plan. Obviously, in conditions of stopping the acute inflammatory process in the periodontium, it is easier for doctors to assess the current clinical situation, the true mobility of the teeth, and the resulting gum recession. From experience, it can be noted that even with further surgical treatment using modern osteoplastic materials and membranes, recession, if increased, is very slight, and in some cases the degree of root exposure can even be reduced by carrying out orthodontic treatment or bringing the contact point closer to the gingival papilla (Fig. 16, 17).
rice. 16. Severe gum recession with abnormal position of teeth against the background of periodontitis. rice. 17. Reduction of gum recession after orthodontic treatment.
Only when remission of the inflammatory process in the periodontium is achieved can a correct, informed decision be made on further therapeutic measures [9]. Thus, an orthodontist will be able to assess the possibility of moving teeth, and an orthopedic dentist will be able to assess the possibility of using teeth as a support for fixed dentures. Sometimes the effectiveness of deep cleaning of the gums is so high that there is no need for surgical interventions with flaps and the time for complex rehabilitation of the human dental system is significantly reduced. The effectiveness of the following stages of treatment also increases.
For example, even in the case of a surgical intervention with a flap, the surgeon will not spend additional time removing dental plaque, which, in conditions of generalized lesions, will certainly significantly reduce the operation time. Regardless of the preservation of the tooth, the procedure for regenerating bone tissue or preserving the volume of the socket will be more effective, since bone formation will occur in the absence of an inflammatory process, the retaining function of the sutures will also increase due to the restoration of the original gum density (Fig. 18-22).
rice. 18. Abscess formation in the area of the 11th tooth with severe periodontitis. rice. 19. View 1 month after professional hygiene. rice. 20. View 5 months after the removal of teeth 12 and 11 with osteoplasty of the sockets. rice. 21. View 2 years after prosthetics on implants. rice. 22. Look when smiling.
Thus, a correctly carried out first stage of treatment of moderate periodontitis creates conditions for increasing the effectiveness of complex dental rehabilitation, reduces the likelihood of complications and increases patient confidence in the team of specialists.
Information about the author Zakirov Taras Valerievich, Ph.D., Associate Professor of the Department of Pediatric Dentistry and Orthodontics, USMU (Ekaterinburg)
Zakirov TV, Ph.D., Assistant, Department of Pediatric Dentistry and Orthodontics, UGMA
Features of the initial stage of treatment of patients with severe periodontitis
Annotation. Periodontitis is one of the diseases with mild symptoms in the initial stages of its development. Typically, the only symptom of mild periodontitis is bleeding gums when brushing your teeth. Over time, this symptom disappears, and the disease does not manifest itself for a long time.
By the time severe periodontitis develops, the patient accumulates a whole complex of problems in the form of a pronounced loss of supporting-retaining periodontal tissues, pathological mobility and displacement of teeth, endo-periodontal lesions develop, periodontally altered occlusion, and occlusion of the dentition is disturbed.
Annotation. Periodontitis is one of the diseases with mild symptoms at the initial stages of its development. Usually the only symptom of mild periodontitis is bleeding gums when brushing your teeth. Over time, this symptom disappears, and for a long time the disease does not manifest itself.
By the time severe periodontitis develops, the patient has accumulated a whole range of problems in the form of pronounced loss of periodontal supporting and retaining tissues, pathological mobility and tooth dislocation, endoperiodontal lesions, periodontal malocclusion develop, and occlusion of the dentition is impaired.
Key words: periodontitis, empirical antibiotic therapy, periodontal pocket, granulation tissue
Keywords: periodontitis, empirical antibiotic therapy, periodontal pocket, granulation tissue