Generalized periodontitis is a type of oral disease that belongs to the group of inflammatory diseases and affects periodontal tissue. Its course is accompanied by bleeding gums, swelling, and unbearable pain. The situation is aggravated by the occurrence of bad breath, the appearance of dental plaque, and the formation of periodontal pockets.
Only a competent periodontist can diagnose the disease by examining the oral cavity and performing a biopsy of the gum tissue. Treatment involves the use of medications and surgery. General and immunomodulatory therapy plays an important role.
Periodontitis is a condition in which diffuse disruption of the periodontal complex occurs. The disease affects several teeth at once, and in particularly serious cases, all teeth. This is one of the most difficult problems in dental practice. The generalized form of the disease is 5 or 6 times more likely than caries, leading to partial or complete adentia. And the prolonged development of infection in the oral cavity is the cause of the formation of rheumatoid arthritis, infective endocarditis, atherosclerosis, stroke, and heart attack.
What is periodontium, its features
In dental practice, the term “periodontium” is used. It includes a whole complex of tissues surrounding the teeth. They all have a common nerve origin and a single blood supply, therefore they are closely related to each other. The periodontium forms several constituent elements: gums, bone tissue, periodontium, cement of the root system of the teeth. Its functions include providing support, maintenance, and protection of the entire dental system. Pathologies associated with periodontal damage include conditions such as gingivitis, periodontal disease, tumors, and periodontitis.
Causes of gum recession
Quite often, gum recession is one of the manifestations of periodontitis (periodontal disease). In this case, as a result of poor circulation in this area, gum atrophy and exposure of the tooth root occurs.
As a rule, this condition is diagnosed in middle and older age, although there are exceptions - for example, juvenile periodontitis.
Gum recession due to periodontitis
Chronic mechanical trauma to the gums - for example, from an overhanging edge of an artificial crown or filling, which happens very often, trauma from a removable denture or its fixing element - a clasp, which, due to the rapid development of implantology, is much less common today. The presence of tartar is also a risk factor for the development of gum recession.
Chronic gum trauma with wide crowns
Acute trauma to a tooth, leading to its displacement towards the lip or cheek.
Acute trauma – tooth dislocation
Anatomical features of the structure of the alveolar process - a thin layer of cortical bone located on the anterior surface of the alveolar process or the so-called “thin gum biotype”.
In the latter case, the problem is not the thickness of the bone, but rather the thickness of the gum covering the bone along the anterior (vestibular) surface. However, in both cases, the problem is associated with insufficient blood supply to the area.
Gingival recession as a consequence of thin biotype
Incorrect (low on the upper jaw or, conversely, high on the lower jaw) location of the frenulum of the lip or frenulum of the tongue.
Gingival recession of the lower incisor due to a labial frenulum
If in the case of a lip frenulum, the recession will be located on the front surface of the tooth root, then in the case of a lingual frenulum, the posterior (lingual wall) of the tooth will be exposed.
Another cause of gum recession can be orthodontic treatment, which can result in thinning of the vestibular bone.
And, of course, oral hygiene can also cause recessions and wedge-shaped defects. Moreover, oddly enough, too thorough brushing of teeth is not at all a good thing, because as a result of excessive mechanical action, both the gums and teeth suffer, in the cervical area of which wedge-shaped defects are formed, which we wrote about above.
Reasons for the development of generalized periodontitis
The precursors to the formation of the disease are some exogenous and endogenous factors. The first group is small; most of the diseases of this system are provoked precisely by the internal state of the body. All etiological factors are classified into local (plaque, tartar, problems with bite, abnormal position of teeth, strands of the mucous membrane) and general (diseases of the body - diabetes mellitus, goiter of toxic origin, excess weight, hypovitaminosis, hepatitis, gastritis, etc. ). All this one way or another affects the condition of the periodontium and leads to a deterioration in its functioning.
Microbiological studies have been able to prove the fact that the leading role in the development of this condition is given to microorganisms called Prevotella Intermedia, Bacteroides forsythus, Peptostreptococcus, etc. In order for the dental system to be protected from their influence, protection in the form of plaque is provided in the dental plaque , accumulated in the gingival sulcus, periodontal pockets, and tooth roots.
The life products of pathogenic organisms contribute to the activation of the secretion of certain substances (prostaglandins, cytokines, enzymes), which lead to the destruction of periodontal tissue structures. Factors that entail a decrease in local and general protection from the influence of pathogenic bacteria include:
- smoking,
- radiation damage,
- ignoring the rules of personal hygiene regarding the oral cavity.
The development of this condition is usually preceded by inflammation of the gingival margin, which entails disruption of the connection, destruction of the ligamentous apparatus, and resorption of the alveolar bone. These changes lead to pathological mobility of teeth, overload of their individual groups, and occlusion. In the absence of adequate therapy, this disease provokes tooth loss or removal, as well as problems with the functioning of the jaw system as a whole.
Periodontitis
Diabetes
Atherosclerosis
2170 26 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Periodontitis: causes, symptoms, diagnosis and treatment methods.
Periodontitis is a chronic inflammatory disease of the dental system, which is accompanied by the gradual destruction of the tissues surrounding the tooth (periodontal tissue) and a decrease in the volume of the bone tooth socket (alveoli) and the entire alveolar ridge. The name “periodontal disease” is considered outdated, but implies processes similar to periodontitis.
Most often, the disease has a chronic course, accompanied by the appearance of deposits on the teeth, redness and bleeding of the gums, the formation of deep periodontal pockets and pathological mobility of the teeth.
Gradually, this leads to tooth loss in an adult and contributes to the development of pathological processes in the body. Complications of periodontitis can include sinusitis, osteomyelitis, and diseases of the cardiovascular system.
Causes of periodontitis
Periodontitis is a multifactorial disease, meaning it can occur for many reasons. Acute periodontitis (periodontitis) is less common than chronic and is most often the result of mechanical or chemical trauma to the periodontal junction. An abscess (ulcer) appears on the gum, which can lead to the appearance of a fistula (a canal connecting the abscess cavity with the external environment).
Chronic periodontitis often develops as a result of poor oral hygiene, when the activity of oral microorganisms increases.
Soft and hard deposits on teeth are a biofilm, which also includes pathogenic bacteria. Their activity can lead to inflammation of the gums (gingivitis), periodontium (tissues surrounding the root of the tooth) and alveolar bone tissue. The inflammatory reaction leads to the gradual destruction of the ligamentous apparatus of the teeth. The necks of the teeth become exposed, and the teeth gradually become loose and fall out.
Local factors causing the occurrence of periodontitis include overload of the periodontium due to malocclusion due to crowding of teeth, poor prosthetics or loss of a group of teeth. The habit of clenching your jaw tightly and grinding your teeth also leads to overload and inflammation of the periodontium.
The development of periodontitis can be caused by a narrowing of the lumen of blood vessels due to diabetes mellitus, atherosclerosis, changes in the composition of saliva, and tissue swelling that occurs due to endocrine disorders.
In addition, the role of vitamin deficiency in periodontal diseases has been proven. Thus, hypovitaminosis C leads to fragility of blood vessels, decreased collagen synthesis, which weakens the ligaments of the teeth, and a general weakening of the immune system.
Classification of periodontitis
Depending on the clinical symptoms and speed of development of the disease, periodontitis is divided into acute and chronic. An acute process, accompanied by pain and bleeding of the gums, develops within a few days after physical or chemical trauma, most often soon after the placement of a filling, crown or other orthodontic structure. If left untreated, acute periodontitis can be complicated by a fistula. However, in most cases, the acute process is replaced by a chronic one, which can last for several years. In this case, the period of attenuation of clinical symptoms due to provoking factors is replaced by a relapse.
In most cases, the disease becomes chronic from the very beginning. This is facilitated by poor oral hygiene and the formation of soft and hard deposits on the teeth. Chronic periodontitis begins gradually and spreads to the entire surface of the gums, then it is called generalized.
If bleeding gums are observed periodically and are caused by brushing teeth and eating hard foods, a diagnosis of mild periodontitis is made.
With increased bleeding, pain, loosening and loss of teeth, moderate and severe degrees of generalized periodontitis are noted.
Symptoms of periodontitis
In acute periodontitis, pain, swelling and bleeding of the gums develop within a few days after exposure to a traumatic factor. As a rule, pain occurs not only when biting, but also outside of chewing load. It is possible for an abscess to form in the area of the “causal” tooth, which breaks through to form a fistula. If the traumatic factor is not eliminated (remove the crown, remove excess filling), the fistula can become a permanent outlet for pus accumulated in the gingival abscess.
Symptoms of chronic periodontitis develop gradually.
However, over time, mild pain when brushing teeth and chewing becomes commonplace. Bleeding becomes constant, the gums change color, and the necks of the teeth become exposed. The periodontal pockets, which can be measured with a dental probe, deepen. There is an unpleasant odor from the mouth, a burning sensation, pain in the gums and jaws, which intensifies when the teeth are closed. Painful pustules may form under swollen gums. Eating becomes difficult. Gradually, the necks of the teeth are exposed, the bone sockets in which the teeth are attached are reabsorbed, then the teeth become loose and easily fall out.
Diagnosis of periodontitis
First of all, a clinical blood test and a biochemical blood test are needed to assess metabolic processes (total protein, protein fractions, C-reactive protein, ALT, AST, LDH, creatinine, electrolytes: potassium, sodium, chlorine, calcium) and urine for differential diagnosis with inflammatory processes caused by blood diseases (leukemia, agronulocytosis, aplastic anemia, thrombocytopenic purpura) or various diseases of internal organs (including endocrine ones - diabetes mellitus, dysfunction of the liver and kidneys, etc.).
Classification and symptoms of generalized periodontitis
If you take into account the depth of the pockets and the severity of bone tissue destruction, the doctor can diagnose three forms of manifestation of the disease. They differ in symptoms and signs.
Mild periodontitis
This stage is characterized by a slight sensation of itching and burning. Bleeding periodically occurs during brushing your teeth and after eating (hard foods - meat, fresh fruits and vegetables). The depth of periodontal pockets reaches 3.5 mm, and a decrease in gum tissue is observed at approximately 1/3 of the height of the root. Pathology may not manifest itself for a long time. Therefore, at the first stage of the disease, patients are in no hurry to contact doctors, which provokes the transition of the disease to more severe forms.
Average degree of periodontitis
During its course, various pathological changes occur in the patient. In particular, the functions of the dental system change. The pocket reaches a depth of 5 mm, the teeth become mobile and slightly loose. Gaps appear between them. The tissue structure of the hole is reduced by half the root. There may be an unpleasant odor coming from your mouth.
Severe periodontitis
This disease is typical for adult patients. The depth of the periodontal pockets exceeds 5 mm, the loss in tissue is more than ½ the length of the tooth root. The gums are subject to severe inflammation and bleed. They come out with purulent discharge. Not only tissue elements are destroyed, but also bone parts. Sometimes the walls between the teeth completely dissolve, leading to severe tooth mobility. In this case, it is almost impossible to preserve them in their natural form.
The more advanced the disease, the more difficult it is to cope with it and choose adequate treatment. And the chances of a full recovery decrease with each step of its progression.
Classification
According to the number of units affected by pathology:
- Catarrhal (localized) – 1-3 units in the affected area;
- Generalized – the entire dentition is affected.
According to the severity of generalized periodontitis (ICD code K05):
- Generalized mild periodontitis (ICD 10 code K05.3). This clinical diagnosis is made when the depth of the pockets in the gingival tissue is less than 3.5 mm, and less than 1/3 of the root is resorbed.
- Average. The subgingival depressions are 3.5-5 mm, and the bone is sclerosed at 50% of the root length.
- Severe degree. This stage is indicated by the depth of periodontal changes greater than 5 mm and resorption of more than 1/2 of the root.
Differential diagnosis according to pathogenesis:
- acute - more than one annual exacerbation;
- chronic generalized periodontitis (according to ICD K05) is an ongoing pathological process;
- exacerbation of chronic periodontitis – pain, discomfort, activation of the inflammatory process.
Features of the chronic form of generalized periodontitis
Any other oral disease can be a provoking factor in the development of the disease. Gingivitis, neglect of personal hygiene rules, mechanical damage - all these are obvious reasons for the development of a chronic form of pathology. It occurs in two stages:
- exacerbation, accompanied by throbbing pain in the gums, excessive bleeding, pus discharge, abscesses, fever, inflammation of the lymph nodes (such symptoms often make themselves felt against the background of pneumonia, stressful situations, ARVI);
- remission, which occurs during therapeutic measures; during this time, symptoms do not appear, and nothing bothers the patient.
The further the pathology develops, the longer the exacerbation lasts, and the time of remission gradually decreases.
Generalized periodontitis (GP) currently occupies a leading place among periodontal diseases among the population of all age groups.
According to the World Health Organization, the maximum prevalence of periodontal tissue diseases, including GP, occurs in the age category of 35-44 years.
According to some studies, from 65% to 95% of the most able-bodied population in different countries of the world suffers from periodontal diseases.
A significant proportion of these patients will eventually require surgical treatment using various osteoplastic materials to restore bone tissue.
The occurrence of functional disorders of the dentofacial system as a consequence of damage to the oral cavity is recorded 4-5 times more often than with complications of caries.
Untimely treatment and ineffective symptomatic treatment of generalized periodontitis in almost 50% of clinical cases lead to early loss of groups of teeth in able-bodied patients of relatively young age.
Complications of HP require significant financial costs and qualified dental care to fully restore chewing function.
The lack of a trend towards a reduction in the incidence of HP in Russia and post-Soviet republics dictates the need to find new methods of prevention, early diagnosis and effective treatment.
The most important criteria for successful treatment of periodontitis are the elimination of bone pockets, manifestations of the inflammatory process in the periodontium and traumatic occlusion with the achievement of long-term stable remission.
The most effective way to achieve these goals is the use of surgical treatment methods using modern osteoplastic materials, as well as the comprehensive use of additional conservative methods.
According to foreign studies, the redox balance of oral and gingival fluid plays a key role in the treatment of periodontitis in the context of maintaining the activity of natural biochemical reactions and reducing the manifestations of metabolic acidosis in periodontal tissues.
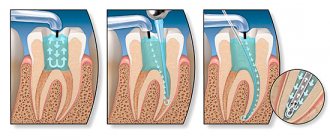
For the surgical treatment of generalized periodontitis, various types of gingivectomy, curettage, and numerous flap techniques are used. The key to success is the correct choice of techniques and materials.
Characteristics of osteoplastic materials for the treatment of periodontitis
The development of surgical treatment of HP originates from the resection technique of periodontal surgical interventions. It involved mandatory leveling of bone tissue in areas of bone pockets with excision of the soft tissue component of periodontal pockets. This resulted in excessive post-operative gum recession.
Thanks to the progress of surgical periodontology and the emergence of more modern surgical intervention techniques, the need for mechanical removal of the affected bone tissue has disappeared. Improved clinical results were achieved through more gentle sanitation of periodontal pockets and ensuring more effective reparative regeneration of bone tissue in these areas.
In the first half of the twentieth century, the famous scientists Widmann, Neumann and Cieszynski proposed a completely new surgical approach.
It involved performing flap operations with a specific type of incision and detachment of mucoperiosteal flaps to access intraosseous pockets and adequate removal of granulation tissue, subgingival dental plaque and stratified ingrown epithelium.
Complications of surgical treatment of periodontitis were serious:
- Multiple gum recessions
- Unacceptable aesthetic defects
- Tooth hypersensitivity
Due to numerous complications, especially in the areas of the frontal group of teeth, researchers almost immediately began work on a deep modification of the new technique and the search for fundamentally new solutions to the problem of GP.
Among them, the modified Widmann flap, coronally and laterally displaced flap, split flap, non-displaced flap and others appeared.
Despite obvious progress, due to the proliferation of osteoplastic materials and membranes, the resection approach began to be replaced by the regenerative concept of treatment. A technique for targeted regeneration of periodontal tissue
(SRT).
Materials for the restoration of periodontal tissues are classified by origin:
- Autogenous
- Allogeneic
- Xenogeneic
- Alloplastic
Alloplastic materials, in turn, can undergo complete or partial resorption or remain unresorbed in the defect area.
Classification depending on the severity of osteogenic potential:
- Osteoinductive
- Osteoconductive
- Osteoneutral
Some authors classify into a separate group materials that are used for targeted bone and tissue regeneration. Bone autografts of intra- or extraoral origin are classified as osteoinductive materials.
According to the concept of Boyne (1973), the optimal osteoplastic material for periodontal purposes should meet the following criteria:
- Availability in required quantities
- Promoting revascularization of the defect site
- High osteoinductive potential
- Osteoconductive properties
In addition, the ideal material should not interfere with the formation of new bone tissue, and to obtain it the patient should not undergo additional painful manipulations (excludes autografts).
Cohen et al in 2011 put forward additional requirements for osteoplastic materials for periodontal purposes:
- Lack of antigenic properties
- Resistance to microorganisms
- Preventing tooth root resorption
- Mechanical strength and elasticity
- Adaptation to the three-dimensional structure of the bone pocket
- Stimulation of new attachment formation
- Complete osteogenesis and cementogenesis
- Formation of a functional periodontal ligament
- Prevention of apical migration of epithelium
Autogenous bone tissue
in the form of bone autografts (intra- and extraoral origin) best meets these requirements. Currently, it remains the gold standard for the surgical treatment of periodontitis.
Autogenous bone tissue was previously used as an osteoplastic material characterized by a number of positive properties. It can be intraoral (bone exostoses, toothless areas of the jaw, hump of the upper jaw) or extraoral (proximal epiphysis of the tibia) of origin.
Autologous bone was used by mixing bone chips with the patient's blood in a sterile container to create a mixture to fill the bone pockets. However, such a product had a very unpleasant tendency to microbial contamination and further sequestration.
The feasibility of the clinical use of autologous bone in regenerative periodontology has been confirmed by numerous histological studies. They confirmed the ability of autogenous osteoplastic material to form new connective tissue attachment.
However, given the always limited amount of donor autologous bone, especially from intraoral sources, as well as the need for painful surgery, its use has been limited.
According to Dumitrescu, the above features should be taken into account when planning periodontal treatment in cases of multiple deep bone pockets. This limits the widespread use of autologous bone and requires the involvement of a qualified, high-profile specialist for intervention.
Therefore, a number of alternative materials were subsequently developed for the surgical treatment of generalized periodontitis. Among them were allogeneic materials, hydroxyapatite (HAP), and growth factors in combination with HAP.
However, the presence of antigenic properties, a weak osteoinductive effect, the need to create specific conditions for collecting and preserving the material, as well as the impossibility of standardization for osteogenic potential complicate their use.
When using xenogeneic osteoplastic materials
For the treatment of periodontitis, special treatment largely eliminates the antigenic effects. However, the presence of the problem of antigenic incompatibility during xenoimplantation, along with immunological incompatibility, retains the threat of material rejection.
However, despite the positive properties of xenogeneic osteoplastic materials and their wide practical application, the problem of potential prion transfer even after careful chemical treatment has not been solved.
An alternative for periodontology has become the use of inorganic and organic synthetic materials
. Among them worthy of attention:
- Synthetic hydroxyapatite
- Alpha and beta tricalcium phosphate
- Organic synthetic polymers
- Bioactive glass
- Calcium sulfate
- Calcium carbonate
- Bioceramics
Various combinations of these products with other osteoplastic materials have also gained some clinical significance.
Among the disadvantages of bioceramic materials for the treatment of HP is their ability to transform during the preparation process into hard and inelastic masses that do not facilitate rapid integration with the surrounding bone tissue.
The use of collagen in surgical periodontology is popular in many countries around the world. Combinations of highly purified collagen with sulfated glycosaminoglycans (sGAG), hyaluronic acid, hydroxyapatite and tricalcium phosphate, and autografts have been proposed.
Melcher formulated the concept of directed tissue regeneration in 1976.
Data from histological studies have demonstrated the successful formation of new connective tissue attachment in humans as a result of the use of this technique, which was first shown back in 1982.
The CTP concept has opened up exciting possibilities for clinical applications of various types of membranes
- resorbable and non-resorbable. But the presence of technical difficulties, including the occurrence of exposure (resorbable membranes) and the need to involve a qualified surgeon to prevent complications during periodontal intervention, are associated with a deterioration in their results.
Use of autologous periosteum
in periodontal practice it is a relevant method due to its high biological compatibility.
The presence of fibroblasts in the periosteum ensures the attachment of various types of undifferentiated cells to the soft tissue and the internal cambial region, which contains mesenchymal and osteoprogenitor cells.
Periosteal cells produce, under specific influence, an intercellular matrix with the subsequent formation of a membrane structure, which takes part in the formation of complete bone tissue.
The use of autologous periosteum is an effective method in the treatment of periodontal furcation defects of bone pockets and gingival recession.
The need for additional surgical intervention to collect material limits the use of the method. Therefore, Saimbi et al in 2014 proposed a new technique for transplanting autologous periosteum from a mucoperiosteal (full-thickness) flap.
Considering the peculiarities of using each of the materials for STR, the search for the most universal option for periodontal regeneration is one of the most pressing issues of modern regenerative periodontology in Russia and in the world.
According to foreign authors, the goal of treating generalized periodontitis and treating periodontal defects of any type is to achieve predictable regeneration of lost periodontal tissue.
Choosing a surgical treatment method for periodontitis
Personalized comprehensive treatment of periodontitis using therapeutic, surgical, orthodontic and physiotherapeutic methods is an effective way to achieve long-term remission.
In the 1980s, research demonstrated the formation of new connective tissue attachments through the concept of guided tissue regeneration. Karring's experimental studies have determined the role of the oral epithelium, alveolar bone, periodontal ligament and gingival connective tissue in the regeneration of periodontal tissues.
The authors showed that it is the cells of the periodontal ligament and root cement that take part in the formation of new cement on the root surface. This played an important role in the further development of therapeutic approaches and surgical techniques.
Numerous authors have concluded that successful treatment of periodontitis with a decrease in the depth of bone pockets is possible subject to complex treatment
, combining measures of professional oral hygiene, non-surgical and surgical.
Currently, much attention is paid to modern methods of conservative therapy for GP, which suggests delaying periodontal surgical interventions. This is explained by the introduction of new methods and protocols for patient management using modern devices and medications that expand the possibilities of conservative treatment of periodontitis.
Modern technologies make it possible to influence the chronic inflammatory process of periodontal tissues and their redox state, helping to achieve optimal clinical results before surgery.
Analyzing data from three decades of research, Cortellini et al showed that regular ultrasonic scaling
and smoothing of root surfaces with a periodontal pocket depth of 4-6 millimeters provides a decrease in depth by an average of 1.3 mm with an increase in the level of clinical attachment by 0.55 mm.
With a periodontal pocket depth of 7 millimeters or more, a decrease in depth is achieved within 2.15 mm with an increase in the clinical attachment index by 1.2 mm.
According to other authors, it will take 4-8 weeks to evaluate the effectiveness of the conservative phase of treatment of generalized periodontitis before moving on to the surgical phase. This is the optimal time.
Badersten et al point out that reduction in pocket depth can last up to 9 months (!), so early probing and assessment of pocket depth reduction 8 weeks after treatment may provide unreliable information, hastening the transition to the surgical phase of periodontitis treatment.
But according to other authors, the transition to the surgical phase of treatment of HP, especially in the presence of multiple deep periodontal pockets, should begin if there is no improvement in periodontal status after conservative therapy.
Despite the existence of generally accepted classical surgical techniques, the issue of choosing the optimal technique using additional methods remains poorly understood and requires further clinical research.
Schwarz et al note that the percentage of patients with pain after surgical periodontal treatment is 20-40%, which negatively affects the effectiveness of treatment of GP and further cooperation.
This fact requires the development and modification of surgical interventions aimed at minimizing pain in patients.
Many foreign authors compared different groups of surgical techniques
periodontal interventions and indicators of PC depth, level of increased clinical attachment and other indicators. Among the main compared treatment methods:
- Resection surgery
- Modified Widmann flap
- Sublingual curettage
- Scaling with smoothing of root surfaces
Summarizing the publications of Pihlstrom, Silvestri, Ramfjord and other studies, we can conclude that with a periodontal pocket depth of up to 6 mm
Ultrasonic scaling and smoothing of root surfaces is the most effective procedure.
With a periodontal pocket depth of 7 mm
The decrease in depth after surgery using the modified Widmann flap technique averaged 4.8 mm, and the level of clinical attachment was 3.3 mm.
Studies by Serino and Linghe have shown that the greatest change in clinical attachment loss can be achieved by avoiding the bone recontouring step in deep pockets and tightly suturing the periodontal wound.
Other authors obtained similar results and concluded that when the depth of the root layer is from 6 mm, it is necessary to perform flap operations after preliminary scaling with smoothing of the root surface, which reduces the depth of the root layer and increases the level of attachment to the maximum extent.
Reddy's studies have shown that de-epithelialization of the flap is a necessary step during flap operations and affects the indicators of periodontal status during treatment using the modified Widmann flap technique.
Ramfjord and Reddy compared the clinical effectiveness of the coronally advanced flap and the modified Widmann flap, finding a reduction in attachment loss after modified flap surgery.
However, numerous studies by Bosshardt and others demonstrate that there is no clinically significant improvement in the reduction of PC depth and clinical attachment loss when using such techniques.
Studies by Zamet et al have shown that the coronally advanced flap is a more effective surgical technique in reducing periodontal pocket depth compared with the modified Widmann flap. However, the technique does not improve the rate of clinical attachment loss.
Ben-Yehouda et al demonstrated a slight superiority in the effectiveness of the coronally advanced flap technique in reducing PC depth compared with the modified Widmann flap.
The results of the six-year Axellson study indicate the effectiveness and importance of providing regular maintenance therapy after the surgical phase of treatment for HP.
Histological studies by Bosshardt and Salaria demonstrated that, despite existing surgical techniques for periodontal treatment, they can result in the formation of a wide zone of ingrown epithelium with tissue recession and loss of underlying bone tissue. In this case, the speed of migration of epithelial cells into the periodontal wound exceeds the speed of migration of ligament cells.
These
and other listed points are important to consider when choosing a method of surgical treatment of HP. , along with the development of modern osteoplastic materials for the treatment , are current problems in periodontology.
Treatment methods for periodontitis
Treatment of chronic generalized periodontitis is complex and depends on the severity of the manifestation. In general, medical and preventive measures are aimed at solving a number of problems.
- Elimination of symptoms that cause discomfort.
- Relieving inflammation in the oral cavity.
- Strengthening the protective properties of periodontium.
- Prevention of the appearance of dental deposits in the form of stone and plaque.
- Prevention of relapses and exacerbations.
This is the general treatment plan. There are private sets of measures, depending on the stage of progression of the pathology.
Generalized periodontitis: symptoms and treatment
Periodontitis is a very common pathology of periodontal tissues (soft tissue structures around the dental unit). If the pathological process is started and left without treatment, then you can lose all the dental units.
Periodontal pockets are the best location for the emergence and development of an infectious process, which does not have the best effect on the healthy state of the body. A beautiful and healthy smile gives you self-confidence and makes you feel natural. When periodontal tissue is damaged, the gums become red and swollen. The disease affects the overall health of the body and the well-being of a person. If something bothers you in the oral cavity, you should immediately consult a specialist. Dentist therapists at the branches of the West Dental family clinic in Yanino-1 and Vsevolozhsk will help with identifying the origins of anxiety and their treatment.
It has been scientifically determined that the occurrence of periodontitis is influenced by: soft plaque and hard deposits; filling material or orthopedic structure fixed in violation of treatment protocols.
Directions of therapy for mild periodontitis
The chronic form of mild periodontitis is treated in stages, here is an approximate diagram.
- First, plaque and deposits formed on the tooth enamel are removed.
- Subsequently, the doctor prescribes topical antibacterial agents. They need to be applied in the form of applications to the affected areas. An important role is played by rinsing the mouth with solutions containing antiseptic components.
- The key to successful therapy is compliance with hygiene procedures (purchase and use of special healing pastes, professional toothbrushes, dental floss).
By providing thorough daily oral care and learning to visit the dentist regularly, you can avoid this sore and prevent worsening if it progresses.
Mild degree
As usual, mild degrees are not given any importance. A subgingival pocket is formed near the dental unit, where microorganisms accumulate. There are signs of periodontal inflammation, and on the Rg image there is destruction of bone tissue by 1/3 of the root, gum pockets up to 3.5 mm. In the cervical area of the teeth, hard deposits are observed, the gums are loose, slightly inflamed and swollen. There is slight bleeding when cleaning, and discomfort when chewing solid food. Mobility and movement of teeth is not observed at this stage.
Treatment of moderate periodontitis: possible options
If the disease is of moderate severity, therapy will take longer. In addition to these procedures, the complex should include the removal of decayed teeth and the use of steroidal and non-steroidal anti-inflammatory compounds. Also, to improve the general condition, doctors prescribe physiotherapy procedures:
- exposure to affected areas through short-wave ultraviolet radiation;
- carrying out a special massage of the gums, which can be vacuum, vibration, etc.;
- darsonvalization procedures;
- local hypothermia;
- electrophoresis.
Upon completion of treatment, it is necessary to make a follow-up visit to the doctor so that he can assess the general condition and make a prognosis.
Causes of the disease
Periodontitis is considered a polyetiological disease - it is formed in most cases by a combination of several predisposing factors. Activation of the inflammatory process is provoked by external and internal factors, systemic and local disorders of the body. The causes of periodontitis are divided into two large groups: endogenous and exogenous.
Endogenous causes of periodontitis:
- diseases of the digestive tract;
- some types of vitamin deficiencies, especially lack of ascorbic acid;
- endocrinopathies - diabetes mellitus, hypothyroidism, thyrotoxicosis;
- vascular diseases;
- bruxism.
Some researchers describe a hereditary predisposition to periodontitis, but it has not yet been fully proven.
Exogenous causes of periodontitis:
- plaque and tartar - found in approximately 90% of patients with periodontitis;
- pathogenic microorganisms;
- chronic dental injuries associated with malocclusion;
- Iatrogenesis - consequences of improper dental treatment, for example, non-compliance with prosthetic technology;
- basal caries;
- gum recession;
- the absence of several teeth - the formation of periodontitis in this case is associated with a violation of the distribution of chewing load.
The causes of periodontitis in most cases act in combination: a combination of several factors leads to disruption of microcirculation in the area of the periodontal junction. Then an infection occurs, which intensifies the inflammatory process. The impact of waste products of microorganisms on bone tissue is accompanied by its resorption (resorption), which leads to a weakening of the fixation of teeth in the jaw. If left untreated, the symptoms of periodontitis continue to worsen and ultimately lead to edentulism.
Treatment methods for generalized severe periodontitis
Chronic periodontitis, the course of which has moved to the last, most dangerous stage, requires not only careful conservative therapy, but also surgical intervention. Indeed, at this stage, tissue destruction is pronounced, and conventional antibiotics are not enough. You will need to undergo a number of procedures aimed at restoring the affected areas and replacing teeth. Depending on the overall picture, the following types of surgical interventions are prescribed:
- removal of teeth with a high degree of mobility;
- vertical dissection of the gum wall in order to scrape tissue that has undergone pathological changes;
- horizontal excision of the pocket wall together with the affected gum (if the depth of the periodontal pockets is more than 4 mm);
- flap surgery (coronal displacement, lateral, therapy, transplantation, etc.);
- abscess incisions;
- plastic surgery in the frenulum of the tongue, lips.
An important role in the treatment of this form of the disease is played by the use of anti-inflammatory drugs, vitamin compounds, and drugs that strengthen immune function. The prognosis of the disease at this stage is unfavorable, since exacerbation does not entail remission and lasts almost constantly. In addition to tooth loss and gum decay, there is the possibility of systemic complications.
Treatment of chronic periodontitis
Therapy for chronic periodontitis has several goals: to reduce the patient’s discomfort, stop inflammation and eliminate its causes, and restore damaged periodontal tissue. As a rule, doctors prescribe comprehensive treatment for periodontitis, which includes:
- professional cleaning (removal of plaque and tartar);
- antibacterial and anti-inflammatory therapy, as well as stimulation of tissue regeneration;
- physiotherapeutic procedures - electrophoresis, laser therapy, darsonvalization, etc.;
- surgical intervention - curettage (treatment of gum pockets);
- splinting to secure mobile teeth;
- opening of abscesses, removal of teeth with pathological mobility, osteoplasty;
- treatment of diseases that contribute to the development of periodontal disease (diabetes, gastritis, etc.);
- correction of occlusion.
You should be prepared for the fact that treatment of periodontal tissue will take time, especially if the patient consulted a doctor with moderate or severe chronic periodontitis. Restoring the affected areas can take from several months to several years, although in complex cases, losses cannot always be completely restored. But with due attention, regular visits to the periodontist and maintenance therapy, stable remission can be achieved.
What to do to avoid complications
To avoid complications, it is necessary to recognize the disease in the early stages and take measures for adequate treatment. All this will allow you to achieve stable and long-term remission and preserve the functions of your teeth and gums. In order for the dental system to be healthy, it is necessary not only to observe the rules of personal hygiene, carrying out regular care procedures, but also to periodically visit a specialist who will perform professional cleaning in order to remove minor dental deposits.
General symptoms of the disease
In the initial stages, the patient suffers from severe bleeding gums. They become loose and swollen. The patient feels itching, throbbing, severe burning, pain when he chews food. An unpleasant odor begins to emanate from the mouth. Dental pockets at this stage are shallow, they are located mainly in the interdental spaces. At the initial stages, the teeth are motionless and not displaced anywhere. The patient's general condition is normal.
The clinical picture of the developing disease is somewhat different. In addition to the above symptoms, the patient may experience:
- displacement of teeth and their loosening;
- high sensitivity of teeth to external irritants (temperature fluctuations);
- problems chewing food;
- disturbance of general well-being (typical of severe forms of pathology), accompanied by weakness, malaise, and increased body temperature;
- an increase in the size of regional lymph nodes, which in addition become painful;
- during a dental examination, the doctor observes signs of diffuse gingivitis;
- Plaque and deposits accumulate abundantly on the teeth;
- tooth loss, fistula, abscesses (signs are characteristic of advanced stages of the disease).
In the case of a chronic form of the disease, the gums have a pale pink tint. There are no dental deposits, manifestations of pus or blood. There is a possibility of exposure of the roots of the teeth. X-ray does not show signs of bone resorption.
Severe degree
Chronic generalized severe periodontitis, as diagnosed, is determined by deep periodontal pockets over 5 mm and 2/3 of the tooth root being exposed. With this degree of pathology, great swelling, bleeding and hyperemia of the gums occurs, and eating is quite painful. In periodontal pockets there is a large accumulation of pus and microorganisms in the form of dental deposits. Patients have complaints of pain, itching, burning and pulsation in the gums. It is impossible to carry out high-quality hygienic cleaning on your own; a persistent unpleasant odor persists for a long time. In the absence of proper therapy, severe suppuration and mobility of grade III-IV units are observed, up to prolapse. Complications may develop in the form of abscess formation of foci of infection and periodontal disease.
Also, this pathology is manifested by a violation of the general condition of the body. A person is worried about weakness, fever, and in connection with this, fatigue. Regional submandibular lymph nodes enlarge and become painful on palpation.
Diagnosis of generalized periodontitis
In identifying the disease, a special role is played by the clinical picture and the “age” of the disease. If there are concomitant diseases, the doctor can refer the patient for examination to other doctors - an endocrinologist, therapist, gastroenterologist, immunologist, rheumatologist, etc. When analyzing dental status, the doctor should pay attention to the following criteria:
- the amount of deposits on the teeth;
- their character;
- general condition of the gums;
- depth of the vestibule of the oral cavity;
- features of bite;
- condition of the bridles;
- degree of tooth mobility;
- formation of periodontal pockets.
As part of the initial examination, a Schiller-Pisarev test is taken and the periodontal hygiene index is determined. The doctor also examines scrapings from the gum pocket using PCR diagnostics and saliva chemiluminescence. Among additional diagnostic methods, it is recommended to conduct a biochemical analysis of blood fluid for glucose and CRP. Of no small importance is the determination of IgA, IgM, IgG indicators.
To identify the stage of development of the disease, the following is used:
- orthopantomography,
- x-ray of the intraoral cavity,
- biopsy of gum tissue.
Doctors pay special attention to differential diagnosis with pathologies such as gingivitis, periodontal disease, periostitis, and osteomyelitis. Like therapy, diagnosis must be comprehensive and include several examinations to make the most accurate diagnosis.
Symptoms of periodontitis
Dental periodontitis is a disease that manifests itself somewhat differently in different forms. The clinical picture depends on the extent of the lesion and the activity of the inflammatory process. Let's take a closer look at what it is - the forms and stages of dental periodontitis.
Generalized periodontitis
This is the most common and unpleasant type of periodontitis - the pathological process affects both dentitions, the inflammation is generalized (widespread) in nature. At the initial stage of periodontitis formation, signs of widespread gingivitis prevail:
- swelling and looseness of the gums;
- tendency of the mucous membrane to bleed;
- pain when chewing food;
- itching and burning at the base of some teeth;
- unpleasant odor (halitosis).
As the inflammatory process develops, hyperesthesia of the teeth is noted, and they become loosened and displaced. In the most advanced cases of periodontitis, signs of a systemic inflammatory reaction appear: body temperature rises, general weakness increases, and local lymph nodes enlarge. The specialists of the AcademyDENT clinic will help you even with the most severe form of periodontitis, but the sooner you contact, the better the result.
The degree of bone destruction and the severity of periodontal pockets are criteria for classifying the disease into degrees:
- I degree - periodontal pockets in depth do not exceed 3.5 mm, and resorption affects the alveolar bone to a depth of no more than 1/3 of the length of the dental roots.
- II degree - the depth of the pockets approaches 5 mm, resorption extends to a depth of up to half the length of the tooth root;
- III degree - the depth of the pockets is significantly more than 5 mm, the resorption process affects the bone for more than half the length of the roots.
This division is necessary to determine treatment tactics - grades I-II can be treated with conservative methods, but grade III cannot be avoided without surgical intervention.
Localized periodontitis
The main difference between this form is the volume of the lesion - only a few teeth are involved in the process. Usually its occurrence is associated with local exposure to pathogenetic factors:
- in the absence of several teeth, which leads to improper distribution of the load when chewing;
- in case of dental injuries, when the periodontium is damaged at the site of impact;
- with improper dental hygiene, when certain areas of the dentition are not cleaned thoroughly enough.
In general, the symptoms of localized periodontitis are no different from the symptoms of generalized periodontitis, but their severity is usually somewhat less.
Acute periodontitis
The clinical manifestations of acute periodontitis are pronounced - there are both local signs of inflammation and systemic manifestations. Patients are concerned about severe pain in the gums, which intensifies when chewing. Even a slight mechanical impact on the gums causes bleeding. When examining the mouth, swollen, loose gums with areas of hemorrhage are visible; against the background of a long-term process, loose teeth are found. In 30% of patients with the acute form, suppuration is observed from the gum pockets.
Acute dental periodontitis is a disease that often becomes chronic if proper treatment is not available. At the AcademyDENT clinic, treatment of acute periodontitis for the first time is carried out so thoroughly that relapses, and especially chronicity of the process, do not occur.
Chronic stage
Without treatment, the process becomes chronic. Chronic dental periodontitis is a disease characterized by a less aggressive course. This form of the disease occurs more often in people with weakened immunity against the background of some systemic pathology, for example, in patients with diabetes mellitus. Symptoms of inflammation are rather weakly expressed; degenerative-dystrophic changes prevail.
In chronic conditions, the gums have a pale color, the destruction of bone tissue occurs much more slowly, but the result is still loosening of the teeth and loss of teeth. Typically, there is an alternation of remission with episodes of exacerbation, in which the symptoms of acute periodontitis come to the fore. Exacerbations occur from 1 to 5 times a year; in rare cases, remission lasts more than a year.
Periodontal measures for moderate disease
If the disease has become moderately severe, selective therapy is added to the above measures. It is aimed at grinding the surface of teeth that have undergone occlusion, removing deposits under the gums, applying therapeutic dressings and compresses. Along with this, questions are being resolved about whether it makes sense to remove roots or individual teeth, and whether it is worth carrying out splinting and orthopedic therapy. Local anti-inflammatory procedures are usually complemented by general therapy.
Is it possible to cure chronic generalized periodontitis?
In the process of getting rid of generalized forms of severe periodontitis, surgical manipulations are added to the listed methods. As part of these procedures, teeth with 3-4 degrees of mobility are removed, patch surgery is performed, abscesses are opened, etc. Based on the available indications, plastic surgery of the vestibule of the oral cavity and frenulum is performed. If the disease is accompanied by a particularly severe course, systemic anti-inflammatory therapy, immunomodulatory treatment, and vitamin intake are mandatory measures.
Physiotherapy takes part in complex therapy. In particular, the doctor prescribes electrophoresis, darsonvalization, laser treatment, hirudotherapy, herbal medicine, and apitherapy. Activities must be carried out under the supervision of a treating specialist in compliance with all his instructions. Violation of the treatment regimen is fraught not only with a lack of effect, but also with a complication of the general condition.
Medical Internet conferences
Acute periodontitis
It is often focal and has a sudden onset with a pronounced clinical picture. Severe pain appears, bleeding gums, inflammation of the gums in a certain area, pain when chewing with teeth located in this area.
There are three stages of the disease:
• Mild degree - there are no visible changes, but itching, bleeding and hypersthesia in the gum area appear.
• Moderate degree - pain, increased bleeding and looseness of gums, periodontal pockets, and tooth mobility appear.
• Severe degree - atrophy of the gums and alveolar processes occurs with exposed necks of the teeth, which ultimately leads to their loss.
Treatment of all stages of acute periodontitis should be carried out comprehensively. General treatment consists of boosting the body’s immune system with a balanced diet, biologically active substances and vitamins. Local treatment includes: removal of tartar, massage of the gums and rinsing of the gums with disinfectant solutions, followed by proper hygienic care of the oral cavity and, if necessary, prosthetics.
Chronic periodontitis
During the course of the disease, alternating phases of exacerbation and remission occur.
Depending on the severity of pathological changes in the periodontium, there are 4 degrees of severity of chronic periodontitis:
• Initial degree - there is itching and pulsation in the gums, loose bleeding gums, a feeling of discomfort when chewing food, and bad breath. When examining the oral cavity, signs of catarrhal gingivitis, the presence of dental plaque and shallow periodontal pockets are revealed, but the teeth remain immobile.
• Mild degree - characterized by the progression of pathological changes. Pain, swelling and bleeding of the gums increases. Soft plaque quickly accumulates, tartar forms, the necks of the teeth become exposed and become hypersensitive. When examining the oral cavity, signs of gingivitis are revealed; periodontal pockets, when pressed on them, release pus. The teeth begin to loosen.
• Moderate degree – increased bad breath, bleeding gums, gums change color, purulent discharge from pockets, gaps between teeth, exposure and hypersensitivity of the necks of teeth to temperature and chemical influences. The teeth are mobile.
• Severe degree - characterized by severe symptoms: increased pain, bleeding gums, mobility and displacement of teeth, swelling of the gums, abundant dental plaque, diffuse gingivitis. Loss of individual teeth is noted.
Exacerbation of chronic periodontitis is accompanied by a sharp deterioration in the general condition of the patient, severe general intoxication is observed, and sharp throbbing pain appears. The severity of chronic periodontitis is determined based on X-ray and orthopantomography data. To determine the microbial contamination of periodontal pockets, PCR scraping and bacteriological inoculation on nutrient media are performed. Chronic periodontitis is differentiated from gingivitis and periodontal disease based on gum biopsy data.
Treatment depends on the severity and includes non-surgical and surgical methods. In the initial and mild form, conservative treatment is carried out, which includes the removal of dental plaque and treatment of the oral mucosa with antiseptic drugs: hydrogen peroxide, chlorhexidine, furatsilin, and anti-inflammatory applications complement the treatment. Physiotherapeutic procedures are prescribed: electrophoresis, laser therapy, darsonvalization, ultraphonophoresis, ozone therapy. Next, the patient is given recommendations on maintaining oral hygiene and using hygiene products [1-3, 5].
Moderate treatment is supplemented with antibacterial therapy to increase immunity, followed by closed and open curettage with medicinal treatment of periodontal pockets. If necessary, therapeutic splinting of mobile teeth is performed.
Severe cases are treated with a combination of therapeutic and surgical methods. In addition to the procedures of local and systemic anti-inflammatory therapy, according to indications, teeth with pathological mobility are removed, gingivectomy, flap operations are performed, and periodontal abscesses are opened.
With timely and correctly carried out complex treatment of chronic periodontitis and the patient’s further compliance with recommendations, the function of the dental system can be restored for a long time.
Generalized periodontitis
It is characterized by bleeding, swelling and looseness of the gums, itching, pulsation and burning in the gum area, pain when chewing food, bad breath, the presence of dental plaque, and the formation of periodontal pockets. In addition to the listed symptoms, loosening and displacement of teeth, increased sensitivity of teeth to temperature stimuli, and difficulty chewing food are also typical.
In severe cases, generalized periodontitis may be accompanied by general intoxication, enlarged regional lymph nodes, and acute pain in the gum area. In this case, there is an abundant accumulation of soft plaque and tartar, multiple periodontal pockets, often with purulent contents. In advanced stages, generalized periodontitis can lead to the formation of periodontal abscesses, fistulas and tooth loss.
In chronic generalized periodontitis in the remission stage, there is no dental plaque or suppuration. The gums are pale pink, the roots of the teeth may be exposed, but there is no bone resorption.
Depending on the severity of the disease, there are three degrees of generalized periodontitis:
• Mild degree – the depth of the periodontal pockets is 3.5 mm; bone resorption does not exceed 1/3 of the length of the tooth root;
• Medium degree - depth of periodontal pockets up to 5 mm; bone resorption is 1/2 the length of the tooth root;
• Severe degree – the depth of periodontal pockets is more than 5 mm; bone resorption exceeds half the length of the tooth root.
Treatment of generalized periodontitis should be comprehensive. Includes local conservative and surgical treatment; general anti-inflammatory and immunomodulatory therapy. Complex therapy, according to indications, includes physiotherapy (medicinal electrophoresis, darsonvalization, ultraphonophoresis, laser therapy, magnetophoresis), hirudotherapy, ozone therapy, apitherapy, herbal medicine.
In case of mild disease, plaque removal, medicinal treatment of periodontal pockets with antiseptics, and periodontal applications are carried out [11 - 14].
When treating moderate periodontitis, the above procedures include curettage of periodontal pockets, application of therapeutic dressings, and grinding of tooth surfaces. If necessary, tooth roots or individual teeth are removed, therapeutic splinting and orthopedic treatment are performed, as well as general therapy.
Treatment of severe generalized periodontitis may require additional surgical intervention: removal of teeth of III-IV degree of mobility, gingivotomy or gingivectomy, flap surgery, opening of periodontal abscesses. According to indications, plastic surgery of the oral vestibule, osteogingivoplasty, and plastic surgery of the frenulum of the tongue and lips are performed. In severe cases of the disease, anti-inflammatory immunomodulatory therapy and vitamin therapy are mandatory.
Localized periodontitis
The localization zone of focal periodontitis is a small group of teeth or tissues around them. This form of the disease has an acute form, which, if left untreated, becomes chronic.
The disease occurs suddenly with the following pronounced symptoms in a certain area of the gum: pain when chewing, bleeding, redness, swelling.
Treatment of focal periodontitis should be comprehensive. The first stage eliminates the causes that contributed to the occurrence of the disease, and the second stage is aimed directly at treating the lesion itself. General treatment for focal periodontitis is not required, since the process is local in nature.
Elimination of the causes of the disease includes the removal of traumatic crowns and overhanging fillings, removal of dental plaque and antibacterial therapy. With a deep bite, deep incisal overlap, or progeny, selective grinding of the tooth tissues is performed. Antibiotic therapy is prescribed to eliminate the source of infection; the choice is made in favor of broad-spectrum antibiotics, which can be tetracycline or metronidazole.
Surgical methods are used when identifying an abscess and deep periodontal pockets: opening the suppuration, cleaning the damaged surfaces and subsequently treating the periodontal pockets.
Next, the patient is referred to dentists - orthopedists, where the design of medical orthopedic devices is selected.
Juvenile periodontitis
Juvenile periodontitis is characterized by the rapid destruction of periodontal tissues with the subsequent formation of periodontal pockets, displacement and pathological mobility of teeth. The process can begin almost asymptomatically, without the presence of a large amount of plaque and pain. At the onset of the disease, symmetrical periodontal damage occurs in the area of the incisors and first molars. Displacement of the first incisors and molars occurs in the labial, buccal and distal directions. Diastemas appear.
Juvenile periodontitis, in the absence of proper treatment, can also take a generalized form, when the entire dentition is involved in the pathological process.
When treatment for desmodontosis is started, it opens up the possibility of preserving teeth in patients. Treatment of juvenile periodontitis is currently carried out using antibiotics in combination with local treatment: curettage, gingivotomy with preliminary depulpation of teeth and the introduction of drugs that enhance reparative regeneration of bone tissue. With already developed stages, it may be necessary to remove damaged teeth and carry out orthopedic treatment.
Refractory periodontitis
Refractory periodontitis is a type of periodontitis that continues to develop despite ongoing therapeutic measures.
The disease occurs with a large number of complications and is accompanied by loss of bone tissue in several areas simultaneously.
After massive loss of supporting tissues, tooth loss occurs. Antibacterial therapy is used in treatment. The prognosis is not favorable. The lack of remission and cure is caused by poor oral hygiene, irregular visits for repeated examinations and, accordingly, lack of maintenance treatment.
Prepubertal periodontitis
Occurs after the eruption of baby teeth. The disease is characterized by almost complete premature tooth loss in children at an early age due to disruption of the attachment of the gums to the teeth and severe destruction of the alveolar bone. In this case, the gum tissue shows pronounced signs of inflammation. Sometimes gum retraction occurs with the formation of cracks. The process, starting with the loss of baby teeth, extends further to the rudiments of permanent teeth. The first sign of the disease is the coating of teeth with a soft coating. Then extreme tooth mobility occurs. At the same time, the child does not feel pain.
Non-surgical methods for treating the inflammatory process of periodontal tissue are the same as in adults - these are professional oral hygiene and various physiotherapeutic procedures. Surgical interventions, such as lip frenulum correction, may also be required.
Rapidly progressing periodontitis
The pathological process is localized simultaneously in the area of several teeth. Sometimes rapidly progressing periodontitis can be accompanied by systemic diseases such as diabetes [7, 9, 12], or Down syndrome. In this form of the disease, immediate destruction of bone tissue occurs, with active periods alternating with periods of remission. During the active period, there are pronounced signs of periodontal inflammation, the release of purulent exudate from periodontal pockets, which entails extensive damage to bone tissue. During periods of remission, the gums are slightly inflamed, bone tissue destruction does not progress.
Rapidly progressing periodontitis can be stopped as a result of therapy, but it is known that the disease often recurs.
Treatment is carried out in several stages:
o Conservative treatment includes removal of dental plaque, physiotherapeutic procedures, antiseptic treatment and anti-inflammatory applications.
o Antibiotic therapy to suppress pathological microorganisms that cause inflammation.
o Surgical treatment includes the elimination of periodontal pockets with treatment of tooth roots and bone defects of the alveolar process, which are filled with a synthetic graft, and subsequently the periodontal tissues are sutured. In case of pronounced destruction of bone tissue and alveolar process after flap operations of pathologically changed tissues and filling of bone pockets with a drug for filling bone cavities - “Kollapan”, 10-12 days after surgical treatment there should be a stabilization of the process and a significant decrease in the pathological mobility of teeth in the area of the performed surgical intervention. This will allow you to preserve and strengthen mobile teeth as much as possible, and subsequently use them as a support for various types of dentures at the stages of orthopedic treatment.
Ulcer – necrotizing periodontitis.
It has an acute onset; the preceding period can last up to two days. During this period, general symptoms appear. In parallel with them, catarrhal phenomena are observed in the form of swelling, redness of the gums, itching and pain appear. When brushing your teeth or chewing, your gums begin to bleed. Over time, ulcers form in the upper part of the gum edge, which are surrounded by a white-gray border and represent areas of tissue necrosis. When trying to remove plaque, bleeding will occur.
As a result of tissue necrosis, a putrid odor appears from the mouth. Even regular brushing of your teeth does not get rid of this unpleasant odor. In such patients, there is often an accumulation of food debris between the teeth. The disease can occur in mild, moderate and severe forms.
The main symptoms are general intoxication, dyspepsia, sleep disturbance, enlarged lymph nodes, bad breath, bleeding and sore gums, itching, and the appearance of viscous and viscous saliva.
Treatment of necrotizing ulcerative periodontitis can be both general and local. The main methods of treating this disease include: professional teeth cleaning to remove plaque and tartar, grinding sharp edges of teeth, using local anesthetics (Lidocaine or Novocaine), using antibacterial agents in the form of solutions and suspensions, and following a diet.
Painkillers should be used to lubricate the ulcerated areas in the gum area. The most commonly used antimicrobial drugs are chlorhexidine solution, hydrogen peroxide or Metronidazole in the form of a suspension.
It can be treated by applying proteolytic enzymes (trypsin). To eliminate inflammation of the gums, applications are used or rinsing is performed.
Of no small importance in the treatment of ulcerative-necrotic form of gingivitis are physiotherapeutic methods, which include laser therapy, ultraphonophoresis, and ultraviolet irradiation. To strengthen the body, it is advisable to prescribe vitamins. The diet involves excluding from the diet foods that can irritate the mucous membrane of the gums.
If conservative therapy is ineffective, when there are extensive necrotic areas, surgical intervention may be required. Necrotic tissue is removed. To prevent relapses of the disease, thorough sanitation of the oral cavity is organized after treatment. With adequate and timely treatment, the patient’s well-being improves within a few days. During drug therapy, epithelization of ulcers occurs.
Forecast and preventive measures
If treatment is started in the early stages of the pathology, this leads to remission and the possibility of its extension. In restoration measures and in the process of preserving tissue functions, compliance with recommendations related to the implementation of preventive measures plays an important role. If the disease is advanced, the prognosis is unfavorable. This may be due not only to the loss of almost all teeth, but also to the fact that severe systemic complications will begin to develop, especially in the cardiovascular system.
The preventive complex involves compliance with a number of care and hygiene measures:
- timely brushing of teeth;
- a competent choice of cleaning products and tools - toothpastes, powders, brushes, threads;
- regular implementation of professional hygiene;
- timely treatment of emerging diseases;
- removal of deposits from the teeth;
- carrying out treatment of concomitant pathologies.
With these simple measures you can prevent illness and feel great.
Thus, generalized periodontitis is a serious disease that tends to constantly develop and progress. In this regard, it is necessary to diagnose it in a timely manner and take therapeutic measures. This approach will prevent complications and keep all teeth normal, eliminating unpleasant symptoms and improving the patient’s well-being.
Catarrhal and hypertrophic gingivitis symptoms and treatment in adults
Splinting teeth for periodontitis with fiberglass and tape
Laser gingivectomy in the area of one tooth
Treatment of generalized moderate and severe periodontitis
The roots of the teeth are exposed - what to do and how to treat them
Open and closed curettage of periodontal pockets
Treatment
When the pathological process has taken the form of chronic generalized periodontitis, it is more difficult to carry out effective treatment. It is important to address the underlying cause of the disease. In this regard, the generalized form of periodontitis requires consultation with dentists in related fields to identify the source of the pathology. The general dentist/periodontist can provide recommendations for consultation with an endocrinologist, hematologist, immunologist, etc. After general interaction and identification of the cause of periodontitis, the attending physician prescribes the necessary therapy.
Treatment of the pathological process consists of the following measures:
- Professional oral cleaning and hygiene training. A specialist removes soft and hard dental deposits, including those under the gums. The tooth enamel is polished with special brushes with paste and coated with a protective gel with fluoride. Oral care products are selected and instructions on their use are provided.
- Treatment of associated dental problems. To cure periodontitis, it is important to treat caries, pulp disease, and pathological processes in the gums and bones.
- Drug therapy. Oral baths with solutions, application ointments, NSAIDs and painkillers, and sometimes antimicrobial drugs are used.
- Removal of subgingival pockets by a dental surgeon. In case of moderate and severe severity, it is possible to perform open and closed curettage of pockets, as well as gum plastic surgery.
- Treatment using orthopedic structures. As part of complex measures, temporary splinting of mobile units is performed with an orthodontic retainer or fiberglass; selective grinding of the chewing surfaces of teeth; prosthetics of large dental defects to redistribute chewing pressure.
- Physiotherapeutic manipulations. Many physiotherapy procedures have a positive effect on recovery: UHF, infrared radiation, magnet and laser therapy, electrophoresis, direct and alternating current, vacuum and acupressure massage, paraffin therapy, mud therapy.
For effective treatment of pathology and the occurrence of remission of the process, it is important to fully comply with the specialist’s instructions.