Composition and properties of tooth enamel
The composition of tooth enamel consists mainly of inorganic substances (more than 95%). Organic substances are represented by proteins, lipids and carbohydrates. The hardness of the enamel layer is determined by the increased content of inorganic substances in it. About 3% of the composition is water. This is where such high strength is achieved. The chemical composition of enamel is unique. The high content of inorganic substances in it ensures that it performs its main functions - protecting the deeper layers of the tooth. Inorganic substances include hydroxyapatite crystals. It is a mineral that contains various elements, including fluorine, magnesium and others. It is because of these crystals that the enamel is so sensitive to the effects of acids. The integrity and density of the enamel layer depend on calcium ions. Calcium is also part of the enamel of teeth and bones. Enamel, consisting of many elements, has a rich composition, which determines its properties.
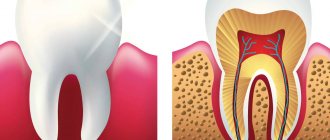
Unlike other hard tissues of the body, enamel does not have a cellular structure (Fig. 1).
Figure 1. Enamel
Structure and properties of enamel
The bulk of inorganic components are represented by crystals of hydroxyapatite (75%), carbonate apatite (12%), fluorapatite (1%) and other forms of apatite, firmly associated with the organic matrix. Thin, long crystals of enamel hydroxyapatites range in size from tens to hundreds of nanometers and differ from crystals of other dense tissues in their size (Fig. 2).
Figure 2. Crystals of hydroxyapatite
The main function of enamel is to protect dentin and dental pulp from external irritants surrounded by a large number of bacteria without catastrophic consequences for the body.
Figure 3. Protective function of enamel
In mature enamel, up to 3.8% water is determined, of which approximately 3.0-3.3% is bound water present in the hydration shell on the surface of the crystals. In immature enamel, the amount of water reaches 20%; with age, its quantity decreases. About 0.5% is free water located in microspaces. The liquid present in the enamel and containing ions is called “enamel liquor”, or “interprismatic spaces” (Fig. 4).
Hydroxyapatite crystals create the effect of a molecular sieve in the enamel, through which small organic molecules and mineral ions penetrate into the enamel fluid. The enamel fluid is distributed unevenly. There is little liquid in the superficial areas of the enamel and its amount increases towards the enamel-dentin border.
Figure 4. Structure of enamel on a cut
Unlike the water in the hydration shells of crystals, the enamel liquid is more mobile and can be removed by heating the dental tissues at relatively low temperatures. The movement of liquid is due to the capillary mechanism, and ions and molecules diffuse through the liquid. Although enamel does not contain cells and is not capable of regeneration, metabolism constantly occurs in it. Ions enter the enamel, mainly from saliva, and also through dentin from the pulp of the tooth.
Chemical composition of enamel
Inorganic substances of mature enamel make up 94-95%, in immature developing enamel they are much less - only 5%, and in the enamel of baby teeth - 80%. (Figure 5)
Once the mineral components are removed, a fine network of organic matrix remains.
In addition to calcium phosphate salts, over 30 different elements were found in the enamel. Mg2+, Na+ ions are present in relatively large quantities, as well as Cl-, K-, Zn2+ and Fe2+. The mineral composition of enamel can fluctuate depending on the nature of nutrition, but the percentage of calcium, phosphorus and carbonate is fairly constant. The content of Sr2+, Pb2+ and some other microelements in enamel varies significantly and depends on their amount in the soil of a given area.
Minerals in enamel are distributed unevenly. The denser surface layers contain less water, carbonates and more fluorine. The amount of inorganic components decreases in the direction from the surface to the zone of transition of enamel to dentin.
The content of calcium and phosphorus in the enamel is respectively 33.6-39.4 and 16.1-18.0% in relation to the remaining elements of the enamel and in the direction from the tooth surface to the dentin their content decreases. Typically, outside it is 37.8 for Ca2+ ions, and inside it is 34.5%, and for phosphates it is 18 and 15%. On the contrary, the content of carbonates, sodium, magnesium and iron in the enamel increases towards the dentin. Lead is present in low concentrations. It accumulates in the surface layers of the enamel, while copper and strontium are evenly distributed throughout the entire thickness of the enamel.
Figure 5. Chemical composition of tooth enamel
To strengthen the enamel, it is important to maintain the balance of calcium and phosphorus in its surface. To do this, it is important to regularly carry out professional hygiene - remove soft and hard plaque, which provokes the appearance of caries. And then apply fluoride-containing preparations to the cleaned surface of the teeth - perform remotherapy.
What is included in the structure: basic elements
The structure of the tooth is complex, it includes not only the enamel. Dentists divide this layer into three components that are connected to each other:
- Prism. Consists of one ameloblast cell. These elements are a kind of foundation of the enamel, running across its entire thickness perpendicular to the connection of the protective layer with dentin. According to their shape, prisms are divided into oval, arched and polygonal; their thickness ranges from 3 to 5 microns.
- Interprismatic substance. This is a kind of binding component that tightly envelops all enamel prisms. The level of mineralization of this substance is slightly lower than that of prisms, and its thickness cannot exceed one micron. The spindles are located in the interprismatic space. These are a kind of processes of odontoblasts, the bodies of which are enclosed in the nucleus pulposus. The spindles grow from the area where the pulp is located, penetrating the enamel and reaching its surface. The processes are responsible for the ability to recognize toothache.
- The cuticle is the most important component of the composition; it is the surface shell of the enamel, which, after eruption, is erased in the area of their chewing surface and is partially preserved in the lateral areas.
Many studies have been devoted to the characteristics of the chemical composition of tooth enamel. Scientists have studied this component in detail in order to create new, more effective methods of dental treatment. Knowing exactly the composition of enamel, it is possible to develop highly effective means for strengthening and restoring it.
In addition to the main components of the enamel layers, it also contains others:
- Neonatal line - visually looks like a dark stripe, present only on milk units. This strip is located in places where two types of enamel intersect: the layer formed before the birth of the child, and the layer that formed immediately after the baby was born.
- Bundles and plates are specific formations that contain hypomineralized prisms; between them there is an interprismatic substance consisting of the same material as the prisms themselves. Chemical analysis demonstrates that, in terms of molecular structure, this material contains a huge amount of protein compounds. Many dentists unanimously claim that it is through the tufts that various bacteria enter the inner layers of enamel from the oral cavity. Then they make their way further, getting into the layers located inside the tooth, thereby causing caries.
- Gunter-Schräger stripes are stripes that stand out in shades on the enamel surface. The shade can be light or dark. Located in a perpendicular position relative to the surface of the enamel, they are formed as a result of opening the prisms.
- Retzius lines are shaped like slightly offset arches, located symmetrically to each other.
Tooth enamel. Its microscopic and ultramicroscopic structure, physicochemical properties.
Formed by: enamel prisms, interprismatic substances, covered with cuticle. The thickest layer of enamel is in the area of the tubercles. Towards the cervical region, the thickness of the enamel gradually decreases. 96% of the enamel consists of inorganic compounds (hydroxyapatite, fluorapatite, carbonate apatite), 4% is an organic base and water. Organic substances are represented by proteins (53%), lipids (42%), and traces of carbohydrates were also detected. The cells that form enamel are enameloblasts; they arise as a result of the transformation of pre-enameloblasts, which differentiate from the cells of the inner enamel epithelium. Enamel is formed by enamel prisms and interprismatic substance. The main structural and functional units of enamel are enamel prisms. They pass through the thickness of the enamel radially, mainly perpendicular to the enamel-dentin border, curved in the shape of the letter S. Enamel prisms are arranged in bunches, 10-20 prisms each. In the neck area, the prisms are positioned horizontally. The cross-sectional shape of the prisms is oval, polygonal, more often arched (in the form of a keyhole). Enamel prisms consist of densely packed and ordered hydroxyapatite crystals. On the surface of the enamel there is a cuticle with a thickness of 0.6-1.5 microns, it represents a structureless organic shell, which is subsequently preserved only on the lateral surfaces of the tooth crown. The enamel cuticle consists of an internal glycoprotein layer (primary cuticle, Nasmyth's membrane) - the last secretory the product of ameloblasts, and the inner layer formed from the reduced epithelium of the enamel organ - the secondary cuticle; on most of the tooth the cuticle is erased; Pellicle - an organic film of precipitates of organic substances of saliva; forms within a few hours after brushing your teeth; dental plaque - is formed as a result of the colonization of the pellicle by microorganisms within 1 – 2 days; tartar - mineralized dental plaque; forms within about a week and a half.
48.Dentin, its microscopic and ultramicroscopic characteristics.
Dentin is the calcified tissue of the tooth, forming its main mass and definition. Its shape. Considered as specialized bone tissue. In the crown area it is covered with enamel, in the root - with cement. Primary dentin. It is formed during the period of tooth formation and eruption, making up the main part of this tissue. It is deposited by odontoblasts at an average speed of 4-8 µm/day, periods of their activity alternate with periods of rest. This periodicity is reflected by the presence of growth lines in dentin. Types of growth lines: Owen's contour lines - directed perpendicular to the dentinal tubules. Ebner's growth lines are located with a periodicity of 20 microns. Between the Ebner lines, with a periodicity of 4 microns, there are lines corresponding to the daily rhythm of dentin deposition. Ebner lines correspond to a 5-day cycle. Secondary dentin (physiological). It is formed after tooth eruption and is a continuation of primary dentin. The rate of deposition of secondary dentin is less than that of primary dentin. As a result of its deposition, the contours of the tooth chamber are smoothed. Tertiary dentin (replacement). It is formed in response to irritating factors only by those odontoblasts that respond to irritation.
49.Cement, its location and histophysiology. Cement is referred to as the supporting apparatus of the tooth. Included in the periodontium.
Cementum is one of the mineralized tissues of the tooth. The main function is participation in the formation of the supporting apparatus of the tooth. The thickness is minimal in the area of the tooth neck and maximum in the root area.
There are acellular and cellular cementum.
Acellular (primary) does not contain cells and consists of calcified intercellular substance, which includes collagen fibers and ground substance. Cementoblasts, which synthesize the components of the intercellular substance during the formation of this type of cement, move outward, towards the periodontium, where the vessels are located. Primary cementum is slowly deposited as teeth erupt and covers the 2/3 of the root surface closest to the neck.
Cellular cement (secondary) is formed after tooth eruption in the apical third of the root and in the area of bifurcation of the roots of multi-rooted teeth. Cellular cement is located on top of acellular cement or is directly adjacent to dentin. In secondary cementum, cementocytes are immured in calcified intercellular substance.
The cells have a flattened shape and lie in cavities (lacunae). The structure of cementocytes is similar to osteocytes of bone tissue. But, unlike bone, cement does not contain blood vessels, and its nutrition is diffuse from the periodontal vessels.
№50
According to the morphological structure, the pulp is represented by loose connective tissue, which contains many cells, intercellular substance, blood vessels and nerve fibers. Its peculiarity is that, along with cellular elements, it contains a large amount of gelatinous ground substance. The fibers are represented by collagen and reticular (argyrophilic), elastic fibers were not detected in the pulp. The main cellular elements of the pulp are odontoblasts, fibroblasts, poorly differentiated cells (stellate, pericytes), sedentary macrophagocytes and others. These cells are distributed unevenly in the pulp, forming a certain pattern. Conventionally, this allows us to distinguish three layers in it: the odontoblast layer, or peripheral, subodontoblastic, or cambial, central. Each of them performs a specific physiological function or exhibits one or another reaction during the development of various processes. 1 - primary dentin; 2 - secondary dentin; 3 - predentin; 4 - layer of odontoblasts; 5 - subodontoblastic layer; 6 - central layer. In the peripheral layer of the pulp, which is directly adjacent to the dentin, odontoblasts are located in several rows. These are highly specialized pear-shaped cells with dark, basophilic cytoplasm. The cell body is rich in cellular organelles: a well-developed intracellular mesh apparatus, a lamellar complex - the Golgi apparatus, numerous mitochondria, the nucleus contains a lot of chromatin and several nucleoli. Towards the apex of the tooth root, the size of cells and the number of rows of odontoblasts in the peripheral layer of the pulp decrease. The subodontoblastic layer consists of small, poorly differentiated stellate cells, from the body of which numerous processes extend, which are closely intertwined. The cells are located directly under the odontoblasts, connect with their elongated body and processes to the odontoblasts and enter the spaces between them. The cells of this layer have the ability, if necessary, to transform into odontoblasts. The central layer of the pulp contains cells such as fibroblasts, which are spindle-shaped. For pulp cells of the fibroblast type, a characteristic functional feature is their differentiation into specific pulp cells, preodontoblasts and odontoblasts. In addition to fibroblasts, this layer contains a large number of sedentary macrophagocytes (histiocytes). The presence of these reticuloendothelial cells in the pulp provides its protective role. Both the subodontoblastic and central layers of the pulp contain a large number of adventitial cells
№52
The cuticle covers the surface of the enamel of teeth after their eruption in the form of a thin shell consisting of two layers and designated as primary and secondary cuticle. Primary cuticle
- an internal thin (about 0.5-1.5 μm) homogeneous layer of glycoproteins, which is the last secretory product of enameloblasts.
The secondary cuticle
is formed by the outer (about 10 µm) layer of the reduced epithelium of the enamel organ. After teething, the cuticle is erased and can partially remain on the proximal surfaces.
Unlike the cuticle, tooth pellicle and dental plaque can form on the surface of the enamel throughout life. Pellicle is an acquired thin organic film that is formed from salivary glycoproteins on the surface of the tooth. The thickness of the pellicle is 1-4 microns. It is a structureless formation that does not contain bacteria and is tightly fixed to the surface of the tooth. The formation of acquired pellicle is influenced by the pH of saliva. The pellicle is formed within 20-30 minutes and its formation begins with the adsorption of specific salivary proteins on enamel hydroxyapatites. Ionic bonds and hydrophobic interactions are formed between the enamel surface and the deposited proteins. Tartar Calcium phosphate crystals are deposited within dental plaque and bind closely to the enamel surface.
The process of deposition of inorganic substances in dental plaque takes about 12 days and after mineralization, the stone is no longer so easily removed by mechanical action or flow of saliva. Bacteria continue to accumulate on the surface of the resulting tartar, promoting its growth. Depending on the location on the surface of the tooth, supra- and subgingival tartar are distinguished. The composition of supra- and subgingival dental calculus is similar, but they differ in the sources of phosphorus-calcium compounds. They enter supragingival tartar from saliva, and subgingival tartar from gingival fluid. Inorganic substances in tartar are associated with proteins, the amount of which is 0.1-2.5% and depends on the type of tartar. The largest amount of protein (2.5%) is present in light supragingival calculus. In dark supragingival calculus, the protein content is reduced to 0.5%, and in subgingival calculus it is only 0.1-0.3%. In addition to proteins, various amino acids are found in tartar. Residues of alanine, leucine, glycine, glutamic and aspartic acids, as well as proline, lysine, serine and threonine are detected in the greatest quantities. Glutamate and aspartate are able to bind Ca2+ ions, and serine, threonine and lysine residues - PO43-, which is very important for the initiation of plaque mineralization and further formation of tartar. No. 51
The periodontium is a complex of tissues that surround the tooth and ensure its fixation in the jaw bones. This complex includes the gum, periodontal ligament connecting the tooth root to the bone socket, bone tissue of the alveolar processes and cementum of the tooth root. Gums . The mucous membrane is represented by two layers: flat stratified highly keratinized epithelium and the lamina propria. There are no glands, lymph nodes and submucosal layer. The mucous membrane fuses with the periosteum of the jaw bone. In the area of the horny ridges of the upper jaw, the stratum corneum of the epithelium reaches its greatest development in ruminants. The main plate is rich in elastic fibers and blood vessels. The main structures of the tooth are: dentin, enamel, cement, pulp. The tooth cavity and the root canal are filled with pulp in the form of fine fibrous connective tissue. Its surface layer contains several rows of cells of mesenchymal origin. They are called odontoblasts and have a pear-shaped shape, basophilic fine-grained cytoplasm, and a basally located nucleus. A long process extends from the outer surface of the odontoblast. It penetrates into the dentin located outside the pulp and lies there in the dentinal tubule (Fig. 253). Odontoblasts are similar in structure and significance to osteoblasts of bone tissue. Thin collagen fibers pass between the odontoblasts, which become the collagen fibers of dentin. Deeper than the layer of differentiated odontoblasts lies a layer of poorly differentiated cells, from which odontoblasts develop. The next layer of pulp consists of loose connective tissue rich in blood vessels and nerve fibers. Dentin makes up the main part of the crown of the neck and root of the tooth. This is a type of bone tissue characterized by significant hardness. As the root of a developing tooth forms and cement is deposited on its surface, the periodontal ligament develops from the surrounding mesenchyme. It consists of wide bundles of collagen fibers, which are located in the form of a suspensory ligament between the cement covering the root of the tooth and the bone wall of its alveoli. The fibers at both ends are immersed in dense fabric. This indicates that the bone matrix of the alveoli, on the one hand, and the cementum matrix, on the other, are deposited around the previously existing collagen fibers. Nevertheless, the rate of collagen renewal in the periodontal ligament is exceptionally high, therefore, during life, significant restructuring of the ligament occurs, at least those parts of it that are not enclosed in dense tissue. Collagen fibers in the bundle run slightly wavy. due to this arrangement, the displacement of the tooth in the bone alveolus is very slight. The periodontal ligament contains a large number of nerve endings that are sensitive to pressure; thus, for example, foreign solids are easily detected in soft foods. The alveolar process is the part of the lower or upper jaw that extends from their bodies and surrounds the roots of the erupted teeth. There is no sharp boundary between the body of the jaw and its alveolar process. It develops along with jaw growth and teething, and after tooth loss it almost completely resolves. The alveolar process is formed by two walls - the outer (buccal or labial) and the inner (lingual). On the outside, the walls are formed by the so-called cortical plates, which are built from compact bone substance. Between the cortical plates of the alveolar process is the labial bone, formed by a system of intertwining bone beams. The spaces between the trabeculae of cancellous bone are filled with bone marrow. The cortical plate provides strength and protection to the underlying bone and serves as an attachment site for skeletal muscles. The cortical plate is denser in the lower jaw than in the upper jaw and has fewer openings for the passage of neurovascular bundles. At the edge of the alveolar process, the cortical plate passes into the wall of the dental alveolus (ethmoid bone), which is a relatively thin perforated plate adjacent to the root of the tooth. Through its numerous openings, blood vessels and nerves penetrate into the periodontium. The space between the two walls of the alveolar process is divided transversely by bony septa, resulting in the formation of a number of individual pits, or alveoli, in which the roots of the teeth are placed.
№53
The glands of the oral cavity include large salivary glands (submandibular, sublingual) and small glands of the hard and soft palate, as well as glands of the tongue. Based on the nature of the secretion that the glands secrete into the oral cavity, mucous, protein and mixed glands are distinguished. Mucous and mixed glands are present in the cheeks and lips. In the area of the hard and soft palate and uvula, mucous glands are secreted. The glands of the tongue are mixed, protein and mucous.
The parotid salivary gland (glandule parotis) is a paired organ located in the parotid-masticatory region of the head. This is a complex branched alveolar gland with a protein type of secretion. The mass of each gland is 20-30 g, the shape is polygonal, the dimensions are 5x4x3 cm. The connective tissue capsule forms an ingrowth into the organ, which divides the parenchyma of the gland into lobules. The terminal secretory sections are protein, in structure they resemble similar structural components of the submandibular salivary gland; in the center of the acinus there are secretory cells - serocytes; myoepithelial cells are located on the periphery; Externally, the acini is surrounded by a basement membrane. The system of excretory ducts of the parotid salivary gland includes insertion, divided, interlobular and common excretory ducts. The named structures do not differ significantly from similar formations of the submandibular gland. The common excretory duct of the parotid salivary gland passes through the buccal muscle and flows into the vestibule of the oral cavity on the inner surface of the cheek at the level of the upper molar.
№54
The glands of the oral cavity include large salivary glands (submandibular, sublingual) and small glands of the hard and soft palate, as well as glands of the tongue. Based on the nature of the secretion that the glands secrete into the oral cavity, mucous, protein and mixed glands are distinguished. Mucous and mixed glands are present in the cheeks and lips. In the area of the hard and soft palate and uvula, mucous glands are secreted. The glands of the tongue are mixed, protein and mucous.
The submandibular salivary glands (glandula submandibulars) are a paired organ located on the inner surface of the lower jaw. The mass of each gland is 10-15 g, the shape is oblate-ellipsoid, dimensions 4x2x1.5 cm. This is a complex alveolar-tubular branched gland with a protein-mucosal type of secretion. Connective tissue septa extend from the connective tissue capsule into the gland, dividing the parenchyma into lobules. The terminal secretory sections of the submandibular salivary gland are of two types - protein and mixed. Protein acini make up the vast majority of the parenchyma of the gland. Each protein acini is built with 10-15 serocytes; myoepithelial cells surrounded by a basement membrane are located on its periphery. Serocytes are conical cells with basophilic cytoplasm, a round nucleus, well-developed elements of the granular endoplasmic reticulum and the Golgi complex. Intercellular tubules are located between neighboring serocytes, which remove the products of the secretory activity of serocytes. Part of the secretion leaves the cells due to their apical surface. Myoepitheliocytes or basket-shaped cells have processes that cover the bases of serocytes. Contraction of the processes of myoepithelial cells promotes the removal of secretions from the terminal secretory sections into the system of excretory ducts.
№55
The glands of the oral cavity include large salivary glands (submandibular, sublingual) and small glands of the hard and soft palate, as well as glands of the tongue. Based on the nature of the secretion that the glands secrete into the oral cavity, mucous, protein and mixed glands are distinguished. Mucous and mixed glands are present in the cheeks and lips. In the area of the hard and soft palate and uvula, mucous glands are secreted. The glands of the tongue are mixed, protein and mucous.
The sublingual salivary gland (glandula sublingualis) is a paired organ of a flattened-elliptical shape, located under the mucous membrane of the lingual area, above the diaphragm of the mouth. The mass of each gland is about 5 g, dimensions - 2x1x0.7 cm. In structure, it is a complex branched alveolar-tubular gland with a mucous-protein type of secretion. Unlike the submandibular and parotid glands, the connective tissue capsule around the sublingual gland is poorly defined. The parenchyma of the gland is divided into segments by connective tissue septa. The terminal secretory sections of the sublingual salivary gland are formed mainly by mucocytes. A small part of the acini also contains Gianuzzi's protein crescents, the cells of which synthesize lysozyme, an enzyme that can dissolve the membrane of some types of bacteria. The base of the acini of the sublingual salivary gland is covered by processes of myoepithelial cells. The inserted and divided straits in the sublingual salivary gland are less developed compared to the parotid and submandibular glands. The excretory ducts of the sublingual salivary glands (straits of Rivinus) flow into the oral cavity at the ducts of the submandibular gland along the sublingual fold. When comparing the parotid, submandibular and sublingual salivary glands, one should pay attention to the uniformity of the structure of the acini of the parotid salivary gland (the presence in its composition of only proteinaceous final secretory sections), the presence of two types of acini (proteinaceous and mixed, with a predominance of proteinaceous) in the submandibular gland and two types of acini (mucous and mixed, with a predominance of mucous) in the sublingual salivary gland.
№56
The following layers of the esophageal wall are distinguished: adventitia, muscular layer, submucosal layer and mucous membrane. The most massive layer is the muscular layer (tunica muscularis), which consists of an outer layer of longitudinal fibers and an inner circular one. The layers are separated by a thin connective tissue layer. The intermuscular autonomic nerve plexus is also located here. Part of the muscle fibers of the esophagus that pass to the mediastinal pleura is called the pleuroesophageal muscle (m. pleurooesophageus). The muscles of the upper third of the P. are striated, and the lower third are smooth. The middle third of the P. contains mixed muscles. The movement of food masses through the esophagus occurs due to active peristaltic contractions of muscle fibers. The mucous membrane of the esophagus (tunica mucosa) is covered with multilayered squamous epithelium, extending from the pharynx. In adults, it consists of 20-25 cell layers 0.5-0.8 mm thick. The epithelium of the esophagus lies on thin fibrillar tissue, which is separated from the submucosal layer by a layer of muscle tissue (tunica muscularis mucosae). There are many mucous glands scattered throughout the mucous membrane. In the caudal part of P., in the mucous membrane itself, there are cardiac glands that produce pepsin. The submucosal layer (tela submucosa) consists of loose connective tissue penetrated by vessels and nerves. There are also many small glands and lymph nodes, especially in the ventral wall of the upper third of the P. The submucosal layer is the least extensible, which is important to consider when suturing the P. The outer connective tissue membrane (tunica adventitia) of the P. consists of intertwined bundles of collagen and elastic fibers and cellular elements. Penetrating between the muscle bundles, adventitia fibers penetrate other layers of the esophagus and form its frame. The most superficial layers of the adventitia, more loose, imperceptibly pass into the periadventitial tissue and connect with the fascial layers of the neck and posterior mediastinum. Fibrous fibers of the adventitia fix P. to the spine. Loose fiber separates P. and forms layers between the organs of the posterior mediastinum.
Specifics of enamel of baby teeth
The main feature of the enamel of the first dental units is that this layer is not as strong as that of permanent teeth. This can be justified by the fact that much fewer mineral compounds are concentrated in baby teeth. If you study the composition of children's enamel in detail and examine it under a microscope, you can draw the following conclusions:
- The Retzius lines, which we mentioned above, are not as pronounced as on constant units.
- The prisms are placed in a horizontal direction.
- There are many microscopic cracks in the enamel of a baby tooth, hence the porosity of its structure.
Given this information, pediatric dentists claim that children's enamel is more susceptible to wear and destruction. For this reason, caries progresses at an intensive rate in children.
Damage to enamel: what to do
One of the most common phenomena is damage to the enamel. There are several types of lesions. It is worth considering that all types of lesions can be classified into two groups: those that formed before the eruption of baby teeth, and those that arose after. The first category includes the following pathologies:
- Dysplasia – there are a lot of symptoms of the disease: the formation of spots, thinning of the enamel layer. Most often, this pathology is associated with genetics and is often accompanied by problems with bone development. Teeth affected by dysplasia erupt with an initially irregular shape.
- Hypoplasia. Tooth tissues atrophy or are absent altogether. The formation of spots, changes in shade, thinning of the enamel are the main signs of the disease. To treat this problem, medications are prescribed that help restore mineral balance.
- Hyperplasia is excess tissue growth. It can also be caused by a mineral imbalance. Various blood diseases and hormonal imbalances can lead to the development of hyperplasia of the tooth buds. Enamel “drops” appear on the tooth surface. In rare, particularly difficult cases, hypertrophied areas can be filled with dentin or pulp.
- Fluorosis. The disease is characterized by the appearance of spots and furrows. Small pits or streaks may appear. Pathology is caused by excess fluoride content in the body. Often the disease affects baby teeth.
Below we will consider pathologies that are not associated with genetics and congenital anomalies:
- Erosion refers to non-carious lesions of the enamel layer and dentin. Erosion can be triggered by gastrointestinal diseases, excessive consumption of too acidic foods, and taking certain types of medications. Drug treatment is prescribed.
- Hypersensitivity. When a person reacts painfully to too cold or hot, this indicates the development of tooth sensitivity, which is often accompanied by thinning of the enamel. In this case, the task is to strengthen the layer. Minerals and vitamins are prescribed.
- Wedge-shaped defect. The pathology is that the neck of the tooth is gradually exposed, and the base is destroyed. The disease can be triggered by thyroid disease, gastrointestinal problems, and gum disease.
- Caries. If the carious lesion of the enamel layer is not eliminated in a timely manner, the disease will spread to the dentin and soon reach the pulp. The disease is treated by cleaning the cavity and installing a filling there.
- Impacts of a mechanical nature. Chips and cracks often form on the enamel. Modern dentists, using advanced equipment, can restore the damaged area.
Damage to enamel after tooth formation
This section describes in detail the causes of diseases and destruction of tooth enamel that are not caused by genetic factors and congenital diseases at the stage of formation of tooth germs.
| Disease | Description | Prevention and treatment |
| Erosion | Non-carious damage to enamel and dentin, which can be caused by eating foods with high acidity, as well as diseases of the gastrointestinal tract, taking certain types of medications and using highly abrasive toothpastes or powders. | Therapy using calcium tablets or solution, mineralization of tooth enamel. |
| Sensitive tooth enamel | Acute reaction to cold and hot. Often associated with thinning of the enamel layer. Thin tooth enamel is also more vulnerable to caries bacteria. | Taking minerals and multivitamins to strengthen enamel. In some cases, orthodontic or orthopedic treatment is required. |
| Wedge-shaped defect | Exposure of the neck of the tooth and gradual destruction of the base. It is characterized by a change in color, a painful reaction to cold and hot in the affected area. | A wedge-shaped defect can be caused by both gum disease and problems with the thyroid gland and gastrointestinal tract. Depending on the cause, treatment is prescribed. The enamel is strengthened by taking medications, electrophoresis and installing fillings in the affected area. |
| Necrosis | Necrosis of tooth tissue begins with the appearance of light spots, which over time become brown or brown. In the vast majority of cases, necrosis is associated with metabolic disorders. | Elimination of the root cause coupled with therapeutic procedures. |
| Tooth enamel caries | First of all, caries affects tooth enamel. If treatment is not started in time, the disease will inevitably affect the deeper tissues of the tooth. | Treatment of the carious area and installation of a filling. In the early stages, today it is possible to treat caries without a drill, followed by restorative procedures for the enamel. |
| Mechanical injuries | Chips, bruises and dislocations of the tooth, as a result of which the integrity is disrupted and cracks form in the tooth enamel. | Therapeutic or orthopedic treatment depending on the type of injury. |
Methods of strengthening
To eliminate pathologies associated with tooth enamel, dentists use various techniques, both therapeutic and orthopedic. For severe lesions, crowns or veneers are used. But the best option for every person is to try to preserve their own healthy teeth. What options for strengthening enamel are suitable for an adult:
- Take vitamins and minerals regularly.
- Use preventive and therapeutic agents – gels and pastes containing calcium and fluoride.
- Regularly visit the dental office for preventive examinations and professional cleanings. This will not only protect the enamel, but also prevent the development of caries.
- If the enamel is damaged and visual appeal is lost, you can undergo a whitening procedure, but only after prior consultation with your doctor.
For children, dentists recommend fluoridation, fissure sealing and other procedures aimed at comprehensively strengthening teeth. Parents should pay attention to their child's diet. It should not contain sweet soda or excessive amounts of sweets. Since tooth enamel contains a large number of microelements, it is worth taking vitamins periodically, after consulting with a pediatrician and pediatric dentist.
How to strengthen tooth enamel?
The level of modern dentistry makes it possible to successfully eliminate tooth enamel defects through therapeutic and orthopedic techniques. In case of serious problems, it is necessary to use crowns, composite or ceramic veneers, but the best option is to preserve healthy and natural teeth. Today, many manufacturers offer various products that help avoid problems such as softening, erosion and thinning of tooth enamel.
Strengthening tooth enamel in adults
- Regular intake of vitamins B6 and B12, group D, as well as drugs that promote the absorption of calcium and fluoride.
- Therapeutic and prophylactic gels and toothpastes. Cleaning tooth enamel with non-abrasive products that contain calcium, fluoride and other components to strengthen the enamel.
- Mineralization of tooth enamel and regular preventive teeth cleaning. If you have naturally weak tooth enamel, these procedures are necessary to prevent the development of caries and other diseases. Tooth enamel whitening can be carried out only after consultation with your doctor, who will confirm the absence of contraindications.
- Prevention at home. Massage the gums, eat vegetables, fruits and legumes.
Remember that tooth enamel does not deteriorate in one day, but over many years, so the sooner you start caring for it, the longer you will maintain an attractive smile.
Strengthening tooth enamel in children
- Fluoridation. Application of special fluoride-containing varnishes to the surface of tooth enamel. After teething, the procedure is recommended to be carried out twice a year.
- The use of preventive mouth guards and application gels containing calcium, fluoride and vitamins.
- Fissure sealing to protect chewing teeth from caries.
Prevention and protection of tooth enamel in children will help to avoid serious problems in the future, so taking care of teeth should begin from the moment they erupt.