Ulcerative gingivitis is an inflammation of the gums, which is accompanied by the appearance of ulcers and necrotic plaque on the gums. The disease can appear and develop on one jaw, but most often affects both the upper and lower jaws. Ulcerative-necrotizing gingivitis, as a rule, occurs in an acute form, although there are cases of development into a chronic form.
The main reason for the appearance of ulcerative gingivitis is insufficiently good oral hygiene, which leads to the spread of pathogenic microbes that cause this disease.
Teeth polishing with pastes - 1,200 rubles.
Polishing one tooth with paste - 50 rubles.
Coating with a fluoride-containing product (1 row of teeth) - RUB 1,500.
Coating with fluorine-containing varnish (1 tooth) - 250 rubles.
Retraction of hypertrophied gums in the area of 1 tooth - 600 rubles.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Classification of gingivitis according to intensity
- easy
- average
- heavy
The severity of the flow is determined3:
The degree of manifestation of general symptoms - weakness, fever, the presence of enlarged lymph nodes. Changes in condition are also reflected in blood tests. With a mild form, the temperature rises to 37.5°C, with a moderate form up to 38°C, with a severe form - up to 40°C.
About tooth loss and how to avoid it
Last year, we, at Star Smile, released a cartoon video in which the heroine was thinking about what to do - either start bite treatment when she was young, or wait until all the teeth begin to decay. Here he is, by the way
The video received quite a lot of views and responses, many patients asked us to continue the topic of consequences - to show readers what inattention and carelessness when caring for teeth and gums can lead to. Therefore, we will continue to educate you and hope that our articles will help you contact doctors in a timely manner and avoid most of the problems that we write about.
Causes of ulcerative-necrotizing gingivitis
Ulcerative-necrotizing gingivitis is caused by fusobacteria and spirochetes. Most often it develops as a complication of catarrhal gingivitis, but it can also be an independent disease. It develops with poor oral hygiene against the background of a sharp decrease in immunity.
General factors
Common factors leading to the onset of the disease are stress, severe fatigue, infectious diseases, and hypothermia. More often the disease is observed in people with diseases of the digestive, endocrine and respiratory systems, heart and vascular diseases. Inadequate and unhealthy diet also increases the risk of developing ulcerative gingivitis. Taking certain medications can also lead to this disease.
Local factors
- Poor oral hygiene In this case, plaque accumulates on the teeth and stones form. With ulcerative necrotic gingivitis, not only ordinary microorganisms accumulate, but also spirochetes.
- Presence of other oral diseases Ulcerative gingivitis can occur as a complication of catarrhal gingivitis and herpetic stomatitis.
- Permanent gum injury For example, old fillings, crowns, dentures.
- Wisdom teeth eruption
- Multiple caries, as it increases the number of pathogens in the mouth
- Injury to the gums by the sharp edges of a carious cavity
- Oral surgery, including complex tooth extraction4
Prevention of ulcerative gingivitis
Prevention of this disease is in many ways similar to prevention of other gum diseases. It consists of observing the following rules:
- timely treatment of chronic catarrhal gingivitis;
- smoking cessation;
- conducting regular thorough oral hygiene;
- Carrying out regular professional cleaning of the oral cavity;
- timely systematic preventive examinations at the dentist.
If you are faced with a disease such as ulcerative gingivitis, seek treatment at the dental department of the CELT clinic. We have everything necessary to successfully cope with even difficult cases.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Symptoms of necrotizing ulcerative gingivitis
The disease develops quickly and rapidly, its symptoms appear very clearly.5,6
- Severe pain that gets worse with the slightest touch or temperature changes
- Swelling of the gums
- Sensitivity of the mucous membrane
- Spontaneous bleeding gums
- The tongue is covered with a green, yellow coating
- Ulcers appear on the surface of the gums, covered with a gray coating.
- A sharply unpleasant, strong odor from the mouth that does not go away even when brushing your teeth
- Increased temperature, weakness, fever
- Necrosis of gum tissue
- Brushing teeth and eating food is difficult
- Lymph nodes are enlarged
- Aches, muscle pain
Publications in the media
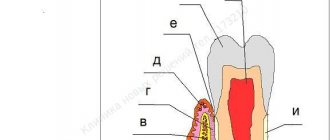
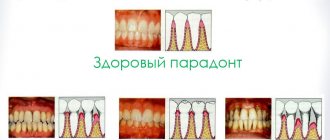
Gingivitis is an inflammation of the gums caused by the adverse effects of general and local factors, occurring without compromising the integrity of the periodontal attachment.
Etiology • Infectious factor (dental plaque) • Mechanical trauma • Chemical irritation, etc.
Risk factors • Malocclusion • Shallow vestibule of the oral cavity • High attachment of labial frenulum.
Pathogenesis. Catarrhal gingivitis develops as a reaction to irritation. Hypertrophic is caused by endocrine disorders and usually develops during puberty and pregnancy. Ulcerative gingivitis is associated with a decrease in the body's resistance and impaired trophism of gum tissue, often associated with immunodeficiency conditions (leukemia, radiation sickness, etc.). Vitamin C deficiency in the body and the use of certain medications (phenytoin, cyclosporine, etc.) are important.
Classification. According to the form, catarrhal, hypertrophic and ulcerative are distinguished, according to the course - acute, chronic, aggravated, remission. According to the severity of the process, mild, moderate, and severe gingivitis is distinguished; according to its prevalence, localized and generalized.
Clinical manifestations
• Chronic catarrhal gingivitis. The disease often occurs without pronounced subjective sensations, but sometimes patients complain of bleeding gums when brushing their teeth or eating solid food. During the examination, hyperemia and swelling of the interdental papillae and gingival margin are detected, which loses its natural pattern (scalloping disappears). Instrumental examination reveals bleeding gums, abundant soft plaque and pockets of subgingival tartar, and the absence of pathological periodontal pockets.
• Hypertrophic gingivitis. Hypertrophic gingivitis is characterized by an increase in gingival papillae, which can reach the cutting edge of the teeth. Hypertrophied gums can be hyperemic, swollen, bleed easily (granulomatous form) or be dense, pale pink in color with the formation of false pathological periodontal pockets (fibrous form).
• Ulcerative gingivitis (Vincent's ulcerative-necrotizing gingivitis). Against the background of hyperemic and edematous gums, foci of necrosis of the gingival papillae or the entire gum margin are determined. In severe cases, the mucous membrane of the retromolar space is involved in the pathological process (ulcerative necrotizing gingivostomatitis). Necrotic tissues are dirty gray in color, easily disintegrate, after which ulcerative surfaces are formed, covered with a dirty gray coating. Characterized by bad breath and enlarged regional lymph nodes. A disturbance in the general condition of the patient is observed, with an increase in body temperature, sometimes up to 39 °C.
Diagnostics. Diagnosis of gingivitis is carried out according to basic (clinical) and additional research methods. Particular attention is paid to oral hygiene, which is always broken (hygiene index more than 1 point). The depth of the gingival groove is determined with a special graduated probe from four surfaces of the tooth. Special research methods include the Schiller-Pisarev test, the Kulazhenko method and rheoparodontography to determine the functional state of blood vessels. An X-ray assessment of the condition of the bone tissue is required: no abnormalities are detected with gingivitis.
Differential diagnosis • Chronic periodontitis • Periodontal disease.
TREATMENT
Local treatment (carried out under anesthesia) includes the elimination of irritating and traumatic periodontal factors: removal of dental plaque, selective grinding of the occlusal surfaces of teeth, elimination of malocclusions, etc. Drug treatment includes antiseptics, antimicrobial and decongestant drugs, and agents that increase local immunity. Preference is given to long-acting preparations: gels, plates. For ulcerative gingivitis, treatment with proteolytic enzymes is carried out, for hypertrophic gingivitis - sclerosing therapy or diathermocoagulation of the gingival papillae; it is possible to use high-energy laser radiation. Physiotherapeutic means used include low-energy laser radiation, UV irradiation, electrophoresis of drugs and all types of gum massage (automassage, hydromassage, vibration massage, vacuum massage).
General treatment includes vitamin therapy (vitamins C, P, PP, etc.). For ulcerative gingivitis, antibiotics and metronidazole are prescribed. With hypertrophic, there is often a need to correct hormonal levels.
The prognosis is favorable, except for cases of hypertrophic gingivitis caused by taking anticonvulsants.
ICD-10 • K05 Gingivitis and periodontal diseases
Diagnosis of necrotizing ulcerative gingivitis
Diagnosis is made through the clinical manifestations of necrotizing ulcerative gingivitis.7,8
During the examination and questioning, the dentist identifies poor hygiene, bleeding gums, poor general condition and the absence of gum pockets (impaired attachment of the gum to the tooth). Be sure to take a panoramic photograph of all teeth to distinguish ulcerative gingivitis from periodontitis.
Additionally, bacteriological examination and the ELISA method can be carried out to confirm the diagnosis, determine the level of immunoglobulins and select appropriate treatment tactics.
It is important to distinguish ulcerative gingivitis from immunodeficiency conditions and blood diseases. For this purpose, if necessary, other tests may be prescribed.
It is important to start treating gingivitis as early as possible
Timely initiation of treatment for gingivitis allows you to completely restore the health of the affected areas of the gums, stop the further development of the inflammatory process and prevent the development of dangerous complications .
Seeking help from a dentist immediately after discovering gingivitis will prevent such a common complication as periodontitis, where not only the mucous membrane of the gums is exposed to the inflammatory process, but also the periodontal tissues that hold the teeth in the sockets: as a result of the onset of periodontitis, the teeth begin to become loose, then become pathologically mobile and subsequently, if treatment is not started in time, they will fall out.
Treatment of ulcerative-necrotizing gingivitis
At the first signs of illness, consult a doctor immediately!
Treatment of ulcerative gingivitis is always complex:
- Anesthesia of the oral cavity with sprays, gels, solutions. With ulcerative gingivitis, this stage is extremely important, since the pain is quite severe.
- Removing the inflammatory process. To do this, use gentle methods to remove plaque and tartar, and be sure to prescribe a course of rinsing with antiseptics for up to two weeks. It is during this visit to the doctor that material is taken for bacteriological examination.
- Removal of general symptoms - fever, headache, for this purpose analgesics and antipyretics are prescribed.
- Destroying pathogenic bacteria, for this purpose antibacterial or antimicrobial drugs are prescribed. (Important! Prescribed strictly by your doctor!)
- Vitamin therapy – to increase the body’s overall resistance to harmful factors.
- During treatment, it is recommended to eat non-irritating foods with sufficient calorie content and not to use spices.
- Treatment of general diseases together with a therapist, gastroenterologist and other specialists.
- After acute inflammation subsides, epithelializing drugs are prescribed (to stimulate tissue healing), professional hygiene, treatment of caries and its complications, removal of wisdom teeth, fillings and crowns (if necessary).
In case of ulcerative gingivitis, it is necessary to strictly follow all the doctor’s recommendations, otherwise complications may arise, and the disease may become chronic.
Removal of dental plaque is carried out under local anesthesia of the gums, using antiseptic drugs, only with the help of hand instruments.
Medicinal preparations containing metronidazole and chlorhexidine are applied to the ulcers, cleared of plaque with special enzymes. These drugs are designed to destroy pathogenic microorganisms, but they should be used only as prescribed by a doctor to avoid complications.
To relieve the inflammatory reaction, local applications with an NSAID solution can be applied for 10-15 minutes.
Symptoms of gingivitis
How does gingivitis manifest? Externally, it can be difficult to suspect the onset of this disease, since in the initial stages gingivitis can go unnoticed. In the initial stages, gingivitis is much easier to detect by a dentist; it most often occurs during routine examinations or when a patient visits a dental clinic with another problem. Due to the fact that many people are in no hurry to see a dentist on time and self-medicate, the disease starts and the pathology progresses.
Bleeding of the gum mucosa is the main, most common and most important sign of gingivitis. But at the initial stage of gingivitis, the gums bleed inconsistently; bleeding occurs after any impact on the gums, for example, when biting and chewing too hard food or while brushing your teeth.
Itching with gingivitis: severe pain in the gum area during the initial stage of the disease occurs quite rarely, but the feeling that they itch is quite common. As inflammation progresses, gum sensitivity increases.
Swelling with gingivitis: not only the mucous membrane itself swells, but also the interdental spaces, they increase in volume, their color changes (redness, cyanosis).
Plaque in gingivitis: soft plaque and tartar are found on both the outside and inside of the teeth. Plaque can penetrate under the gums. A white coating may also appear on the tongue.
If the symptoms of gingivitis were not noticed in time and treatment was not started on time, then the bleeding of the gums intensifies and the patient detects traces of blood on food when biting into it. Moreover, if at first when biting, blood remains only on hard foods, for example, on apples, then later, with the further development of the inflammatory process, blood begins to remain even on relatively soft food.
Treatment of necrotizing ulcerative gingivitis with Tantum® Verde
Effective treatment of ulcerative gingivitis is possible with the use of anti-inflammatory drugs, which include Tantum® Verde . Benzidamine in its composition has a complex effect on the gums: reduces swelling, relieves inflammation, reduces pain and kills microbes on the surface and inside the affected tissues. Benzidamine penetrates well into the mucous membranes, which allows you to quickly cope with the disease. Tantum®Verde allows you to quickly relieve pain9, which is especially important in the treatment of necrotizing ulcerative gingivitis. From the first minute, Tantum® Verde has an anti-inflammatory and local anesthetic effect on the symptoms of gingivitis, such as a burning sensation, swelling and swelling of the gums. After the acute effects have subsided, it is possible to dissolve Tantum® Verde , since they have an anti-inflammatory effect within 9 minutes, which will allow you to quickly cure gingivitis.10, 11, 12
What is gingivitis
Gingivitis is treated by a periodontist.
Gingivitis is an inflammatory process that occurs inside the gums, sometimes accompanied by symptoms such as pain, swelling, swelling of the affected area and a general rise in body temperature. Gingivitis can occur in patients under a variety of circumstances; Inflammation such as gingivitis can occur due to traumatic effects on the gums, penetration of pathogenic microbes into the gums, hypothermia of the body, a sharp drop in immunity, deficiency of certain vitamins, and for other reasons.
Prediction and prevention of necrotizing ulcerative gingivitis
If you consult a doctor in time and receive quality treatment, a full recovery is possible. Recurrence of the disease occurs with exacerbation of chronic diseases, a sharp decrease in immunity and poor oral hygiene.
If you postpone going to the doctor and do not follow the recommendations, ulcerative gingivitis can become chronic, which is less treatable, or develop into a more serious disease - periodontitis, which is accompanied by loss of bone tissue. Therefore, it is important to take a responsible approach to the treatment of this disease.
If a person has suffered ulcerative gingivitis, then a second visit is scheduled after 1-2 months, and then you should visit the dentist every six months.
Prevention of ulcerative gingivitis:
- Regular and adequate teeth cleaning
- Visit your dentist for examination and treatment (if necessary) twice a year
- Strengthening the immune system: you should pay attention to such simple things as physical exercise, proper nutrition, sleep patterns, hardening
- Stress management
- Treatment of existing chronic diseases: it is important to avoid exacerbations, otherwise relapses of the disease are inevitable
- Taking vitamins
Diagnosis of gingivitis and treatment strategy
The dentist’s tactics when identifying inflammatory periodontal pathology includes the following aspects:
- situational analysis of data from questioning, examination, assessment of the patient’s general condition;
- creating a diagnostic hypothesis (the so-called preliminary diagnosis);
- refusal of early prescription and use of systemic drugs until the diagnostic hypothesis is confirmed (or excluded) and a clinical diagnosis is established;
- establishing a clinical diagnosis;
- development of a plan of treatment and preventive measures;
- informed choice of systemic and locally acting drugs, taking into account the nature of periodontal pathology and their clinical manifestations;
- medical examination of the patient.
At the stage of treatment of patients with inflammatory periodontal diseases, a sequence of measures is necessary, including:
- teaching patients the rules of individual oral hygiene;
- measures for professional oral hygiene;
- local use of drugs that have antibacterial and anti-inflammatory effects, affecting microcirculation in the periodontium (Table No. 1);
- elimination of factors that adversely affect the periodontium and aggravate the pathogenic effect of the microflora of the oral cavity and periodontal pockets on it.
Table No. 1. Antibacterial drugs, doses for adults and duration of use [18, 22].
Antibacterial drug | Doses for adults (body weight 70 kg) | Duration of use |
| Tetracycline | 4 times a day 250 mg | 14-21 days |
| Doxycycline | 1 time per day 200 mg per day, then 100 mg per day | 1, 13-20 days |
| Monocycline | 200 mg first dose, then 100 mg 2 times a day | 2-3 weeks |
| Amoxicillin with clavulanic acid (Augmentin, Amoxiclav) | 3 times 625 mg | 7-10 days |
| Ciprofloxacin | 2 times 500 mg | 7 days |
| Azithromycin | On the 1st day 500 mg, on subsequent days 250 mg | 7 days |
| Lincomycin | 2 times a day, 500 thousand units | 10-15 days |
| Clindamycin | 4 times 300 mg | 10 days |
| Amoxicillin | 1 time per day 500 mg per day | 7-10 days |
| Sumamed | 1 time per day 500 mg | 3-5 days |
| Rulid | 2 times a day 150 mg | 10 days |
| Metronidazole | 3 times a day 250-500 mg | 7-10 days |
| Metronidazole + amoxicillin | 3 times a day 250-500 mg metronidazole + 250 mg amoxicillin | 8 days |
| Ampicillin | 4 times a day, 500 mg in combination with metronidazole, 200-250 mg 3 times a day | |
| Erythromycin | 4 times a day, 500 mg in combination with metronidazole, 200-250 mg 3 times a day | |
| Roxithromycin | 2 times a day |
Modern tactics of media treatment of inflammatory periodontal diseases are carried out taking into account the role of oral microflora, biofilm, the presence of periodontal pockets and must necessarily include mechanical removal of supra- and subgingival dental deposits and other measures included in the treatment complex (Table No. 2).
Table No. 2. Antiseptic preparations used for rinsing the mouth and treating periodontal pockets [10].
Name of the drug | Breeding |
| Potassium permanganate | 1:1000—1:10000 |
| Furacilin | 1:5000 |
| Etonium solution | 0,5 % |
| Chloramine | 0,25 % |
| Chlorhexidine bigluconate (Corsodil mouthwash) | 0,05-0,12 % |
| Dioxidine | 1 % |
| Hydrogen peroxide solution | 0,5—1 % |
| Iodine solution | 0,1—0,5—1,0 % |
| Sodium hypochlorite solution | 0,1 % |
| Miramistin solution | 0,01 % |
The choice of medications for periodontal diseases depends on the severity of the inflammatory process, tissue swelling, gum bleeding, the presence of epithelial defects, the stage of the process and destructive changes in the lesion [3]. In modern dentistry, in case of inflammatory periodontal diseases, great importance is attached to maintaining a balance between the microflora and the protective systems of the oral cavity.
In order to correct the composition of microflora, broad-spectrum antiseptics have been proposed: chlorhexidine, triclosan, hexetidine, which are included in many oral hygiene products - rinses, gels, balms, toothpastes (Table No. 2). Many of them also contain herbal medicines. An example of such a combination is eucalyptus gel immobilized on polysorb. Local application of this drug is carried out in the form of applications on thin cotton wool, inserted into periodontal pockets for 20 minutes.
In the last decade, the modern development of the pharmaceutical industry has ensured the constant supply of new antiseptics to the consumer market, but products potentially evaluated for use in dental practice must meet the necessary requirements: have a wide spectrum of antibacterial action, low toxicity, and a low likelihood of developing microbial resistance [8].
Treatment of catarrhal gingivitis
In the presence of a pronounced inflammatory process, it is necessary to apply local antimicrobial and anti-inflammatory drugs in the form of applications, irrigations, medicinal dressings at a doctor's appointment (for example, Metrogyl-Denta - a gel with metronidazole and chlorhexidyl) and mouth rinses at home (for example, Corsodil "- a concentrated solution of chlorhexidine for preparing liquid before rinsing the mouth; infusion of chamomile, sage, etc.).
To improve epithelization processes, keratoplasty agents are used: fat-soluble vitamins A, E, sea buckthorn and rosehip oil, caratolin, solcoseryl.
General treatment. To normalize metabolism, the general reactivity of the body and its antioxidant protection, and stimulate tissue regeneration processes, vitamins and adaptogens can be used. The most commonly used vitamins are A, C, P, E, B vitamins and vitamin complexes (Multitabs, Aevit, Duovit, Complivit, Tetravit, Vitrum, Spectrum, etc.), combined preparations containing vitamins and microelements, other substances (olazol, aekol). It is necessary to remember the side effects and contraindications to the use of these drugs [10].
Complications and consequences of gingivitis
Proper treatment and compliance with the doctor’s recommendations leads to complete recovery and elimination of the inflammatory process. But if gingivitis is ignored and delays in visiting a doctor, then over time the disease will begin to progress and affect neighboring tissues. The most common complication of the pathology is periodontitis, which entails loosening of teeth and their complete loss.
In addition, possible consequences of gingivitis are:
- gum abscess;
- infectious diseases of the jaw bones;
- transition of a simple catarrhal form of gingivitis to ulcerative-necrotic;
- hematogenous infections (glomerulonephritis, endocarditis).
Diet for gingivitis
Since in most cases, gingivitis develops as a result of a lack of nutrients in the body, patients need to undergo vitamin therapy with the consumption of large amounts of fruits and vegetables. The greatest effect in treatment is provided by vitamins A, B, C and D, which are found in pineapples, broccoli, onions, kiwi, carrots, citrus fruits, and blackberries.
Products of plant origin that promote natural salivation and natural cleaning of teeth are beneficial for the oral cavity. To strengthen the gums and clear them of the accumulation of microbes, patients suffering from gingivitis are recommended to consume ginger, celery, sesame seeds, parsley, and dill.
During treatment, the following foods should be completely excluded from the diet:
- alcoholic and carbonated drinks;
- sour, hot and spicy dishes;
- too hot or cold food;
- solid foods (nuts, crackers and other similar products that can damage the mucous membrane).
Dental devices used in the treatment of gingivitis
Treatment of gingivitis at the Telo's Beauty clinic is carried out using modern dental devices, which allow professional diagnostics, teeth cleaning and periodontal therapy without pain and damage to tooth enamel. Thanks to the latest technologies and improved devices, the patient calmly endures any manipulation and receives quality care that previously could only be dreamed of.
| Name | Device functions |
| Estetica E50 | The dental unit is safe to use and is equipped with a wide range of attachments that allow the doctor to perform a variety of manipulations for gingivitis - teeth cleaning, restoration, restoration, caries treatment. |
| Kavo Gendex expert DC | An X-ray machine from the American company Gendex is an improved device that is highly efficient in operation and the ability to take high-quality images of the dentition. Its main advantages include a low dose of radiation and the availability of individual settings that allow the doctor to choose the shooting mode. |
| Kavo Gendex GXDP-700 | The digital x-ray system is used to diagnose gingivitis and obtain dental images in various formats, including 3D. The tomograph allows you to solve any problems in dental imaging and provides focused radiation, which significantly reduces the level of radiation received. |
| Waterlase | A dental laser is a universal device for the treatment of gingivitis, providing high-quality restoration and therapy of diseased teeth - sterilization of canals, treatment of furcation, excision of the gingival margin, etc. |
Folk remedies for Vincent's stomatitis
The disease can only be treated with traditional dental medicine. Folk remedies will help complement the main treatment and speed up healing.
To relieve inflammation after dental procedures, rinsing with decoctions and tinctures based on:
- calendula;
- oak bark;
- St. John's wort;
- daisies.
Oak bark decoction
Causes of gingivitis and provoking factors
The infectious factor plays a fundamental role in the development of gingivitis. Caries, tooth deformation or malocclusion provide favorable conditions for the appearance of plaque and the proliferation of microbes in the oral cavity. Subsequently, the pathogenic microflora that accumulates in the dental plaque leads to a destructive effect on periodontal tissue and, as a result, causes inflammatory processes.
The bacterial etiology of gingivitis should be considered in combination with the individual characteristics of the organism and the influence of the external environment, which provides predisposing conditions for the development of the disease. The main causes of gingivitis include:
- poor oral hygiene;
- gum injury;
- decreased immunity;
- lack of vitamins or minerals in the body;
- tartar (supragingival and subgingival);
- poor quality dental treatment;
- the presence of braces or dentures, which complicate dental care.
In addition to the main reasons, there are a number of factors that can provoke the development of gingivitis. These are smoking, diabetes, depression, infectious or viral diseases (ARVI, tuberculosis, AIDS, etc.), malnutrition, chemical poisoning. Most often, pregnant women and children aged 3–6 years, as well as people with nasal breathing problems, suffer from gingivitis.
Prices for gingivitis treatment in our clinic
The cost of services at the Telo's Beauty clinic depends on the form and degree of the disease - the sooner you seek help, the cheaper and easier it will be to cure gingivitis. In the initial stages of pathology, it is enough to get by with ultrasonic cleaning and polishing of teeth, while in later stages a complex and long-term therapeutic course will be required. In the table below, you can familiarize yourself with our prices and calculate the upcoming costs of treating gingivitis.
| Service | Cost, rub.) |
| Superficial anesthesia | 350 |
| Anesthesia using the Sleeper One device | 800 |
| Plasma injection I-PRF/ 1 tube | 5000 |
| Bone bioreconstruction /fibrin membrane APRF/ 1 tube | 6000 |
| Excision of the gingival margin (1 tooth) | 2000 |
| Relieving enamel hyperesthesia | 1500 |
| Scaling (1 tooth) – removal of hard plaque | 350 |
| Polishing restoration | 700 |
| Whitening with the Beyond Polus system | 22 000 |
| In-canal whitening | 1500 |
Professional treatment of gingivitis at the dentist of our clinic will help you quickly get rid of the disease and regain your beautiful and healthy smile!