Causes
Unlike ordinary sore throat, herpetic sore throat is caused by viruses. Among the main provocateurs, it is worth highlighting the Coxsackie virus type A or B, serovars, and ESNO viruses. They can be infected by droplets, fecal-oral routes, through bodily contact, and unprocessed food.
The pathogen, entering the body, multiplies in the intestines and lymph nodes. The pathogen spreads through the lymph and blood and intensively accumulates in the pharyngeal ring and tonsils. On the third day, the condition of the infected person deteriorates sharply.
Possible complications and prevention
Severe herpes sore throat can lead to the spread of infection throughout the body and damage to internal organs - so-called complications arise. The most common complication after suffering herpes sore throat is serous meningitis, or inflammation of the brain. The disease can lead to disturbances in the functioning of the heart and cause myocarditis, which is diagnosed by an electrocardiogram. Kidney diseases (pyelonephritis), liver, hemorrhagic conjunctivitis - this is just an incomplete list of complications with late diagnosis of the disease and delayed treatment. If you have the slightest suspicion of a disease, do not delay visiting a doctor!
To date, no vaccines have been developed to prevent herpangina disease. During an epidemic, if possible, do not take your child to kindergarten or school. Adults should try to avoid places with a lot of people and remember the rules of hygiene. Both children and adults need to strengthen their immune system in general, eat healthy and balanced, take vitamins and harden themselves.
If there is a sick person at home, it is necessary to ventilate the room frequently, and provide the sick person with individual dishes, linen and a towel.
Symptoms
The following clinical picture appears sharply, acutely and violently:
- Within a few hours the temperature rises to 40°C.
- Chills and general weakness of the body appear.
- My head starts to hurt.
- When swallowing saliva or liquid, an unbearable sore throat develops.
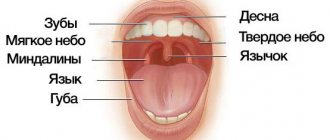
- The color of the mucous membrane of the nasopharynx changes. After a few hours, the throat turns red, and the next day it becomes covered with many reddish blisters.
Acute symptoms last for 2-3 days, and then their intensity decreases.
Preventing tongue ulcers
No one is immune from microtraumas to the mucous membrane and the appearance of minor wounds on its surface. However, provided you have good health, good immunity and good hygiene, such a minor nuisance is unlikely to lead to serious problems. To protect yourself from diseases of the teeth and soft tissues of the oral cavity, it is enough to maintain hygiene, regularly brush your teeth, visit the dentist for preventive maintenance and professional dentistry. hygiene at least once every six months.
Preventive examinations at the dentist will help to recognize pathology in time
It is also advisable to monitor the health of the body as a whole, give up cigarettes and alcohol, diversify your diet with healthy foods, take vitamins from time to time to strengthen the immune system, and try to lead an active lifestyle.
Symptoms of herpetic sore throat in children
Children attending nurseries or kindergartens, as well as schoolchildren, get sick most often. In children in the first three years of life, herpetic sore throat is extremely difficult, since the first signs of the disease are similar to the flu.
In addition to the general signs of intoxication, children appear:
- Temperatures up to 41°C.
- Pronounced hyperemia of the mucous membranes of the mouth and pharynx. During examination, the tissues appear to be filled with blood.
- A day later, 1-2 mm papules in the mouth, surrounded by a red rim. The next day they open, forming ulcers with crusts.
- Runny nose.
- Decreased appetite due to impossible pain.
- Enlarged lymph nodes located in the neck and ears.
If children have weak immunity, then sore throat occurs in waves, i.e. The deterioration of the condition is recorded after a few days, then it improves noticeably.
In addition, children experience stomach upset due to the fact that viruses irritate the mucous membrane of the digestive tract. The child complains of diarrhea and nausea.
How to cure stomatitis on the tongue?
At the first signs of stomatitis, specialists at the LeaderStom clinic recommend contacting a dentist for diagnosis and prescribing appropriate treatment. A person’s attempt to cope with a stomatitis disease that appears on the tongue on his own may not only not lead to the desired result, but on the contrary, increase the symptoms of the disease. The drugs that are used to treat stomatitis on the tongue can be divided into local therapy drugs and medicinal formulations that have a general effect on the human body. Let's take a closer look at each of these forms.
Treatment of stomatitis with local therapy:
- Treatment of stomatitis ulcers on the human tongue with antiseptic gels, ointments and sprays.
- Rinsing the mouth with antiseptic solutions, which can be purchased at the pharmacy (chlorhexidine, miramistin, etc.) or prepared yourself using medicinal herbs such as chamomile or calendula.
- In order to relieve the pain symptom, doctors recommend using local preparations containing lidocaine for a person with stomatitis formations on the tongue.
General therapy for stomatitis:
Depending on the cause that provoked the stomatitis disease, antibacterial, antiviral, antifungal or antihistamines are used. Such drugs are prescribed to a person only by a dentist or therapist. To relieve the symptoms of stomatitis, modern antipyretic and painkillers are used.
Taking vitamin complexes allows you to compensate for the lack of essential microelements in the body, which for one reason or another a person does not receive with food, and vitamin deficiency, as is known, is one of the factors that can provoke stomatitis on the oral mucosa and tongue.
For stomatitis, immunomodulatory drugs are also used - drugs that increase human immunity. They can be of both plant and medicinal origin. All patients, regardless of the reasons that caused stomatitis on the tongue, are recommended by doctors to take these medications.
Drugs are also used to treat somatic diseases. The use of such remedies is necessary if the cause of stomatitis on the tongue lies inside the body. Chronic diseases of certain systems, and especially the human gastrointestinal tract, weaken the body and contribute to the launch of an immune reaction, manifested in the formation of stomatitis ulcers on the palate and tongue.
Diagnosis and treatment
At the appointment, the ENT doctor will examine the patient and conduct an examination. Based on the diagnostic results, drug therapy is prescribed, including:
- Taking antipyretics based on paracetamol or ibuprofen.
- Taking antiviral drugs prescribed after identifying the exact pathogen.
- Taking antihistamines. The active substance helps relieve swelling and ease breathing.
- Resorption of lozenges, lozenges, use of local sprays. Their antiseptic and bactericidal properties reduce sore throat.
- Local use of antiviral ointments based on interferon.
- Taking immunostimulants to activate the body's defenses to fight the pathogen.
It must be emphasized that antibiotics are powerless for this type of tonsillitis, because they do not affect the reproduction of viruses.
Important to remember! Do not apply heat compresses to the throat. Heating promotes the further spread of viruses throughout the body.
In addition to taking medications, the patient must be isolated from others and observe strict quarantine. The infectious period lasts two weeks. You need to follow a diet and eat pureed liquid food, drink more liquid. Water not only prevents dehydration, but also relieves symptoms of intoxication. If you are sick, you should not smoke, drink boiling water or water from the refrigerator.
Since the throat is constantly injured, healing occurs within 10-14 days. Crusts and sores are washed off with saliva without any residue.
It is important to know! Do not touch the bubbles with your hands or try to squeeze them out.
Which doctor treats glossitis and when should you contact him?
When suspicious ulcers are discovered on the tongue, many begin to ask a completely logical question regarding which doctor to turn to for help. In such a situation, you can, of course, immediately make an appointment with a dentist, but it is not a fact that the pathology was caused by a dental problem, and this specialist will be able to provide the necessary assistance. It is better to first consult with your attending physician - after a visual examination, he can send the patient for additional examination, the necessary tests, or immediately refer him to a highly specialized doctor: a gastroenterologist, endocrinologist, immunologist, or again to a dentist.
The formation of strange suspicious spots, plaque and ulcers on the surface of the main speaking organ, the occurrence of obvious pain, burning and tingling sensations - all these are signs of tongue pathology. If we are talking about glossitis, then it can be an independent disease, since it is a secondary sign of disturbances in the functioning of internal organs and systems. In any case, the problem requires an immediate solution, so in such a situation the only correct instruction for action is to urgently consult a doctor.
- Kharitonova, M. P. Burning tongue syndrome (Etiology, clinical picture, differential diagnosis, treatment), 2000.
Specific features of herpetic sore throat
Herpetic tonsillitis can be distinguished from other types of sore throat by the following characteristics:
- A rash appears on the upper and lower extremities and face if not treated in a timely manner.
- Numerous red blisters appear on the pharynx, adenoids, tongue, and palate. Gradually they develop into ulcers and open. A light transparent exudate emerges from the bubbles. Typically there are from 5 to 20 ulcers in the mouth. If treatment is not started in time, the ulcers merge with each other, forming large areas of damage to the mucous membrane of the throat and mouth. In this case, there is a high risk of complications.
Often, parents mistake herpangina for another disease and try to cure it on their own. Herpetic sore throat should not be confused with:
- Thrush. Candidiasis in the mouth appears as a cheesy coating.
- Herpetic stomatitis. Papules are similar, but with stomatitis they are localized on the gums and tongue.
- Purulent sore throat. Formations accumulate only on the tonsils and lacunae, and with herpetic disease they cover the entire nasopharynx. In addition, a runny nose is a distinctive symptom. With purulent tonsillitis there is no runny nose.
How is the treatment carried out?
Treatment of ulcerative glossitis in both adults and children should begin with eliminating the root cause of the problem, and this requires a thorough diagnosis. Only after identifying the source of the pathology can the doctor offer effective therapy. As for symptomatic treatment, to relieve acute inflammatory processes, specialists usually prescribe the drugs Hydrocortisone and Prednisopon. At an advanced stage and the presence of keratinized areas, they are removed surgically. Remember: only your doctor can prescribe medications; any attempts at self-medication can result in very unpleasant consequences.
To restore organ tissue, doctors usually prescribe rinse solutions with an antiseptic effect. These include “Furacilin” and “Chlorhexidine”. But to cope with pain, doctors usually prescribe drugs that have both anesthetic and antiseptic properties - Ledocaine and Kamistad. When answering the question of how to treat other forms of glossitis of the tongue, it is important to note that therapy is selected taking into account the type of pathology and the individual characteristics of the clinical picture.
Desquamative form of pathology
This form is widely known as “geographic language”. On the back of the organ, irregularly shaped light spots appear framed by a whitish coating. From the outside, the drawing somewhat resembles a map of the world, which is why the disease received its name among the common people. Most often, this type of glossitis becomes a consequence of pathological processes in internal organs and systems.
This is what geographic language looks like
Treatment is primarily aimed at achieving stable remission without exacerbations, since the desquamative type of the disease itself most often has a chronic form. Regular treatment of the organ and tissues of the oral cavity is required using anti-inflammatory gels and solutions, such as Chlorophyllipt or Karotolin. If the patient complains of severe pain, novocaine blockades and phonophoresis (ultrasound exposure simultaneously with drug therapy) are prescribed. The patient will also have to follow a special diet and take B vitamins.
Folded tongue
Quite deep and noticeable longitudinal and transverse grooves are formed on the back of the organ. Most often this is a congenital phenomenon, but there are cases when the pathology becomes a consequence of injuries, burns and infections. Symptomatic treatment of the folded form of glossitis is prescribed in the presence of severe discomfort, burning sensation, pain and breathing problems. In this case, antiseptic rinse solutions are prescribed, for example, Chlorhexidine, as well as anti-allergenic drugs if acute symptoms were provoked by an allergic reaction. During therapy you will have to give up salty and spicy foods.
This pathology is treated when causing inconvenience
Catarrhal type of disease
The development of the pathological process is accompanied by the formation of swelling, redness of individual parts of the organ, and the appearance of a dense white coating over the entire surface of the back. The cause of the problem may be a thermal or chemical burn or mechanical injury. As part of therapy, rinses with antiseptic and anti-inflammatory solutions are prescribed, nutrition is adjusted and vitamin complexes are prescribed.
Some problems can be solved by rinsing
Candidal glossitis
The distinctive symptoms of this pathology are a thick cheesy plaque and bad breath. In this case, patients usually do not experience significant discomfort or pain. Candidiasis infection, caused by too intense proliferation of yeast-like fungi Candida, can be triggered by an imbalance of microflora in the oral cavity after long-term drug therapy, taking antibiotics or insufficient hygiene.
Therapy in this case is aimed at restoring the balance of microflora. To do this, a complete sanitation of the oral cavity is carried out, antifungal drugs are prescribed, such as Nystatin or Fluconazole, and vitamin complexes are recommended to strengthen the immune system.
Diamond shape
The epithelial layer noticeably thickens and becomes thicker, taking on the shape of a diamond or rectangle, and a characteristic plaque appears. This type of illness usually indicates a malfunction of the gastrointestinal tract. Since most often this is only a symptom and not an independent disease, treatment should be aimed at eradicating the source of the problem, and rinsing with antiseptics and anti-inflammatory solutions is usually prescribed to relieve symptoms. If the patient complains of pain, painkillers are prescribed.
Purulent-phlegmous type of pathology
The lesion spreads to the deeper layers of the epithelium and may affect adjacent areas of the oral cavity. This is one of the most severe forms, during the development of which the patient’s temperature rises and all signs of intoxication of the body are noted. In such a situation, antibiotics are usually prescribed: Doxycycline, Ceftriaxone, Rocephin and others. In particularly severe clinical cases, surgical removal of the purulent neoplasm is performed, followed by monitoring the patient’s condition during the rehabilitation period.
Gunter's glossitis
This form develops against the background of serious pathological conditions associated with the functioning of the hematopoietic system. The disease is considered a frequent companion to anemia. In this case, the surface of the organ becomes unnaturally smooth and acquires an overly bright red or crimson color. It is necessary to treat first of all the anemia or pathology that has become the root cause of such symptoms. Vitamin B12 is often prescribed as part of therapy.
The photo shows Gunter's glossitis
"Hairy" tongue
Due to the thickening and keratinization of the filiform papillae covering the back of the tongue, the surface of the organ acquires a dark brown or even black color, its texture becomes rough, visually reminiscent of hard stubble. This type of pathology has been studied much less than others. Until now, experts cannot establish the exact prerequisites for its formation. Possible causes include genetic predisposition, infections, taking powerful medications and bad habits.
This pathology is eliminated surgically
To eliminate the defect, it is usually necessary to surgically remove the hypertrophied filiform papillae, after which antiseptic treatment of the oral cavity and anti-inflammatory therapy are prescribed.
Complications
Unfortunately, this type of tonsillitis has dangerous negative consequences if the disease is started and left to chance. The greatest danger is from complications of the kidneys, brain and heart. Since the sore throat virus spreads through the flow of lymph and blood, inflammation can overtake certain parts of the brain, causing meningitis and encephalitis. Convulsions, persistent headache, increasing temperature are reasons to seek medical help again.
At the ENT CLINIC in Chertanovo, ENT doctors with extensive experience will carefully examine an adult and a small patient and immediately perform a serological and virological analysis to determine the causative agent. The technical equipment of our medical center allows us to obtain diagnostic results within a couple of hours. Thanks to this, therapeutic therapy is prescribed in a timely manner, with positive dynamics occurring the very next day.
Diagnostic features
To determine the form of the pathology and the cause of its development, it is necessary to conduct a differential diagnosis. The specialist must conduct a visual examination of the surface of the tongue, teeth and gums, talk with the patient about recent diseases, injuries and mechanical damage, and allergies. In more severe cases, blood tests may be required - general, cytological, histological or bacteriological. Sometimes microscopy of scrapings and PCR diagnostics are required to identify pathogens.
Tests are required for diagnosis