How to squeeze out pus from the tonsils yourself
It is possible to remove purulent plugs from the tonsils at home if they are shallow and there is no swelling with hyperemia of the surrounding tissues.
Facilitates the process of assistance from an adult - a relative, a spouse, if it is impossible to seek professional cleaning from a doctor. Algorithm for step-by-step home elimination of bacterial plaque from the tonsils:
- Wash your hands with soap and water, treat with an antiseptic solution, and if necessary, use sterile gloves.
- Prepare a mirror, targeted home lighting from a lamp, a spoon, a plastic or metal flat stick, and a bandage. It is permissible to use a special sterile spatula, which is convenient and safe to remove pus, without the risk of infection from the outside.
- All objects and instruments for manipulation should be pre-treated with antiseptics and a mirror should be installed so as to see the deposits on the tonsils as much as possible. For disinfection, medications are used: Lugol's solution, Chlorhexidine, Chlorophyllipt, Furacilin solution, potassium permanganate.
- You should take a clean household spoon in one hand and press your tongue, which can reflexively prevent you from clearing your tonsils. In the other hand is a spatula, at the end of which a bandage with an antiseptic is tightly wound.
- Carefully, without strong pressure, try to squeeze out plugs or remove films from the surface with a bandage, scraping without damaging the mucous membrane.
- You should not leave particles of pus or not completely remove bacterial deposits - this can cause new plugs to appear and the development of a sore throat with full-blown clinical symptoms.
- At the end of the home procedure for cleansing the tonsils, it is necessary to rinse your mouth with an antiseptic or chamomile decoction with calendula to disinfect, accelerate healing after manipulation, and prevent relapse.
You can squeeze pus out of your tonsils at home and avoid complications afterwards by following all the above rules. During the day after cleansing, you may experience a feeling of discomfort, soreness, hypersensitivity to cold or hot food, which is a normal reaction. You can relieve discomfort with throat tablets.
How to treat plaque on the tonsils?
To quickly restore health, as well as to prevent the development of complications and the disease becoming chronic, it is necessary as soon as you notice white on the tonsils
Depending on what microorganism provoked the inflammation, he may recommend the use of:
1
Antiviral medications. Drugs of this type are the first means that can be used when the first signs of a cold occur.
They help increase the body’s defenses, so pathogens die much faster and do not have time to cause serious disorders.
The most effective antiviral agents include:
Interferon, Nazoferon, Oscilococcinum, Isoprinosine, Aflubin, Anaferon, Viburkol, Proteflazid, etc.
2
Antiseptic solutions. If you start gargling with antiseptics in a timely manner, it is possible to suppress the development of infection in the early stages.
However, they are also used in later stages of disease progression, as they help eliminate the purulent film.
As a rule, for this purpose it is used
: Rotocan, solution of Furacilin, Streptocide, Chlorophyllipt, Miramistin. If you don’t have them on hand, you can simply rinse your mouth with a weak solution of baking soda. More details about the methods:
3
Antibiotics. Since the main reason that the tonsils are covered with a white coating is bacterial flora, the main method of combating it is considered to be taking antibacterial drugs.
They destroy the cells of microorganisms and thereby lead to their death. Initially, they try to cope with the problem using local agents, for example, with the help of Polydexa or Isofra.
However, in severe cases it is impossible to do without the use of systemic drugs.
For respiratory infections, antibiotics of the penicillin group (Augmentin, Ampicillin), macrolides or cephalosporins are most often prescribed.
4
Fungicides. Antifungal drugs are prescribed exclusively for oral candidiasis. Initially, it is recommended to treat the affected areas with special local agents, for example, Candide.
But in the absence of the desired effect, they are replaced with systemic drugs:
Fluconazole, Itrungal, Nizoral, Orungal, Mikosist, Diflucan and others.
5
Tablets, lozenges and sprays. Such medications help eliminate pain and have a local anti-inflammatory effect.
They are present in a huge variety on the modern pharmaceutical market: Strepsils, Lisobakt, Faringosept, Septolete, Trachisan, Tos-Mai, Isla-Moos, Septefril, Lizak and others.
6
Antihistamines, usually used in conjunction with antibiotic therapy. These are: Loratadine, Eden, Erius, Diazolin, Suprastin, Fenistil.
Patients are also often prescribed professional film removal, carried out in the ENT doctor’s office.
It involves mechanical rinsing with a special solution supplied into the oral cavity from a syringe with a special type of tip. The procedure is quite unpleasant, but effective.
Mistake 1 - going to work
Sore throat is an acute infectious disease that is transmitted from person to person by airborne droplets, so you should not infect others.
But even if you don’t care about the health of your colleagues, you still need to stay home. After all, with a sore throat, strict bed rest is necessary. If you lead an active lifestyle during illness, the body simply does not have enough strength to resist bacteria, and microbes begin to multiply especially actively. They no longer have enough space on the surface of the tonsils, and then, through the bloodstream, pathogenic microorganisms enter other organs - the heart, kidneys, joints. The result is serious complications such as myocarditis and endocarditis (inflammation of the heart muscle and inner lining of the heart), rheumatoid arthritis, glomerulonephritis and other inflammatory kidney diseases. But, even if complications can be avoided, you should know that a sore throat suffered on the legs easily turns into a chronic form.
Disease starting with the letter "A". How to recognize a sore throat and avoid complications Read more
Prevention
In order not to fight white plaque during the period of sore throat, it is necessary to strengthen the immune system in a timely manner. The body's defenses do not prevent the entry of harmful pathogenic microorganisms, so treatment of a disease with weak immunity may be delayed. For prevention purposes it is appropriate:
- Do not overcool;
- Eat properly;
- Temper yourself;
- Carry out immunotherapy during epidemics;
- Undergo preventive examinations with doctors;
- Take vitamin complexes;
- Completely cure dental caries;
- Avoid stressful situations;
- Walk in the fresh air at least 1 hour a day;
- Engage in moderate physical activity.
Do not forget to visit a doctor at the first manifestations of the disease. If you self-medicate, there is every chance of developing the disease.
White plaque on the tonsils is only a symptom that needs to be dealt with. A competent and professional approach to treatment will help you forget about a sore throat within a week. If you ignore the advice of doctors, a sore throat will lead to a number of complications.
Symptoms of lacunar tonsillitis in children
The signs of a sore throat in a child are the same as in adults, only they appear more acutely. The disease progresses rapidly, because The child’s immunity is not fully formed and the defenses cannot resist infection.
Already from the first day, the temperature rises to 40-40.5 ° C, against this background diarrhea and vomiting appear. Some parents believe that there is no need to lower the temperature, because the body fights the infection on its own. This statement is completely false. It is important to immediately reduce the temperature if it rises above 38°C, otherwise convulsions may begin.
When caring for a baby, relatives need to respect communication boundaries and wear a medical mask. Fortunately, lacunar tonsillitis in children rarely leads to complications.
Often this disease in children is treated in a hospital setting. If the condition worsens within 3-4 days, the child is hospitalized. In the hospital, instrumental washing of the tonsils, droppers, intravenous and intramuscular injections quickly improve the baby’s condition.
Treatment of white plaque on tonsils and tonsils
When plaque appears on the tonsils, both with and without pain, it should be taken into account that this is only a symptom. It will not be possible to get rid of it with solely symptomatic therapy; complete treatment of the disease is necessary, which includes:
- Antibacterial therapy for diphtheria, bacterial sore throat, stomatitis of bacterial origin.
- Antiviral therapy for acute respiratory infections, sore throats and stomatitis of viral origin.
- Antifungal therapy for pharyngomycosis or thrush.
- Rinsing with disinfecting solutions to remove film from the tonsils and oral cavity.
- Washing off the purulent film from the tonsils using a special syringe with a solution (this is how plaque is removed only in a hospital).
- Antipyretics for fever.
- Painkillers for severe pain in the tonsils.
- Immunomodulators.
- Maintain a gentle regimen for the throat: avoid spicy foods, loud and long conversations.
- Drink plenty of fluids.
- Taking multivitamins if you have a weak immune system.
It is prohibited to independently select medications to remove the accumulation of pus from the tonsils. At home, without diagnosis and consultation with a specialist, it is impossible to determine the type of pathogen, and therefore the direction of treatment.
Washing and rinsing
Washing of the tonsils is performed by specialists only on an outpatient basis.
The procedure requires special care to avoid injury to the tonsils. It is unpleasant and a little painful, so it is especially difficult to wash off the white coating from the child’s throat. There are also contraindications for this procedure: it cannot be done during pregnancy, cancer, severe hypertension, open tuberculosis, disorders of the autonomic nervous system
But proper rinsing effectively clears a white throat for various causes of plaque.
There are also contraindications for this procedure: it cannot be done during pregnancy, cancer, severe hypertension, open tuberculosis, or disorders of the autonomic nervous system. But proper rinsing effectively clears a white throat for various causes of plaque.
Washing tonsils in the clinic
Rinses can be varied: from cheap home remedies (soda-salt solution, chamomile decoction, furatsilin solution) to expensive pharmaceutical ones. The main condition is the frequency of manipulations. If you wash the tonsils rarely, the effect will not be achieved, since within a few hours the pus accumulates again.
Regular, frequent rinsing (once an hour or as prescribed by a doctor) allows you to remove germs, food debris, and immune cells, which eliminates the formation of a favorable environment for the life of microorganisms. Your tonsils will become less red and painful.
Symptoms of the disease
Sore throat or acute tonsillitis have a pronounced clinical picture. The incubation period lasts from 12 to 48 hours, after which clinical signs appear.
- Increased body temperature (above 39°C, less often 37-38°C). With a sore throat, it is difficult to lower a high body temperature with the help of antipyretics.
- Signs of intoxication are body aches and weakness, headache, chills, dizziness, pain in the chest and heart area.
- Pain and sensation of a lump in the throat. Pain when swallowing.
- Hoarseness of voice.
- Inflammation of regional lymph nodes.
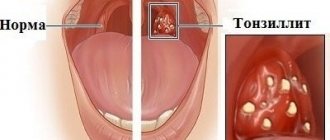
On examination, swelling and hyperemia of the palatine tonsils are revealed. Depending on the type of inflammation, purulent plaque forms on the lacunae or all tonsils.
In some cases, the symptoms of the disease may not be expressed. The temperature may remain within the low-grade range or slightly elevated, accompanied by unpleasant and painful sensations in the throat.
How to remove white plaque from tonsils with sore throat
The appearance of white plaque on the surface of the tonsils is often observed with angina, in particular with its lacunar and follicular forms. The differences between these forms of the disease are that with follicular angina the plaque has the form of dots, and with lacunar angina - extensive spots or a continuous film.
In any case, the formation of plaque indicates a bacterial infection of the tonsils. It is necessary to treat bacterial tonsillitis on time, as it often leads to complications - paratonsillitis, otitis media and even rheumatism.
The question that worries everyone who is worried about sore throat and white plaque on the tonsils is how to remove and remove spots in the throat? Is it possible to do this at home, and how? This article will talk about how to remove plaque from tonsils with a sore throat in a safe way, and how not to do it.
Prohibited methods of treatment for purulent sore throat
Unfortunately, patients often make independent treatment attempts, which only worsen the clinical picture. The following actions are prohibited:
- Pierce the ulcers with sharp objects.
- Push out, tear off or squeeze out ulcers.
- Treat tonsils with hydrogen peroxide, Lugol's solution, iodine.
- Warm your throat and gargle with hot water.
- Rinse with vinegar and concentrated alcohol solution.
- Apply compresses of vodka and alcohol to the throat.
Important to remember! It is very dangerous to try to remove purulent deposits on your own.
At the ENT CLINIC in Chertanovo, otolaryngologists immediately help patients. They carry out non-contact removal of purulent plaque using ultrasound on the CAVITAR device (USOL therapy). Pharyngoscopy and smear analysis are performed to determine sensitivity to antibiotics in order to prescribe an effective medicine. Specialists use modern drugs of the latest generation to improve the patient’s condition. Based on the severity of the disease, individual characteristics, and age of the patient, the clinic’s ENT doctor prescribes medications and gives recommendations for treating purulent tonsillitis at home.
Diagnostics
Not many pathological conditions can cause the appearance of a layer on the tonsils, which is why an experienced specialist will not have difficulty establishing the correct diagnosis. The exception is plaque on the tonsils without fever.
In any case, diagnosis requires an integrated approach and includes:
Palpation of cervical lymph nodes
- conducting a detailed survey of the patient or his parents - to obtain a complete clinical picture for the clinician. It is necessary to inform the doctor about the first time of onset and intensity of symptoms;
- the doctor's examination of the patient's medical history and life history - this is necessary to search for predisposing factors;
- palpation of the neck - to identify enlarged lymph nodes;
- examination of the throat using special ENT instruments;
- laboratory blood tests will indicate the occurrence of a pathological process in the body;
- taking a smear from the tonsils for subsequent bacterial culture;
- PCR - to detect the pathogen that could cause the appearance of a pathological layer on the tonsils.
Only after the otolaryngologist has familiarized himself with the results of all examinations, can he prescribe an individual tactic on how to remove plaque from the tonsils.
To eliminate plaque from the tonsils in adults and children, conservative therapy is indicated, which is aimed at taking medications and using alternative medicine techniques.
Drug treatment includes:
- taking antibacterial and antifungal agents;
- treating the throat walls with antiseptic solutions;
- prescription of a vitamin complex;
- local use of dental anti-candidal ointments, which provide not only treatment, but also pain relief;
- taking agents that absorb and remove toxins;
- rinsing the mouth and throat with soda, saline and furatsilin solution;
- taking painkillers.
Folk methods for removing plaque from tonsils include rinsing the mouth or sucking using the following components:
- chamomile and calendula;
- sage and garlic;
- beet juice;
- lemon and honey;
- Luke.
Before starting such treatment, you should consult your doctor.
Surgical intervention for plaque on the tonsils and throat is used extremely rarely.
What is a sore throat
Classification
The disease can be classified according to the course of the process: acute (tonsillitis) and chronic (chronic tonsillitis). By localization - one-sided and two-sided. By form - typical or banal and atypical or isolated, rare.
Typical forms:
- catarrhal – the most common and relatively easily tolerated;
- lacunar – the second most common form;
- fibrinous - not only the tonsils are affected, but also the mucous membrane of the throat;
- follicular - characterized by purulent inflammation of the palatine, tubal, pharyngeal and lingual tonsils, locally manifested by separate purulent foci on the tonsils;
- phlegmonous (intratonsillar abscess) - characterized by purulent inflammation of the palatine tonsils and other lymphoid formations of the peripharyngeal ring. Most often it occurs as a complication of other types of acute tonsillitis.
Atypical forms:
- the ulcerative-necrotic or ulcerative-membranous form develops in people with severely weakened immunity and vitamin deficiency;
- laryngeal (submucosal laryngitis) can occur not only from exposure to pathogenic microflora, but also against the background of injury or burn of the throat;
- fungal form;
- herpetic – caused by the herpes virus (Kosaki virus) and, unlike other forms, spreads in the summer;
- syphilitic – one of the forms of syphilis, characterized by a long, sluggish course;
- monocytic – one of the forms of mononucleosis;
- agranulocytic – a rare manifestation of agranulocytosis.
Clinical manifestations
The disease is also characterized by severe pain in the throat when swallowing and in the tonsils, severe swelling of the tonsils and lymph nodes, plaque on the tongue and on the mucous membrane of the throat, and purulent plugs in the tonsils.
Treatment
Depending on the pathogen and the form of the disease, treatment is prescribed. The basis of treatment for acute tonsillitis is bed rest, antibacterial therapy, vitamin therapy, diet, and drinking regimen. In case of a viral nature of the disease, antibiotics are not prescribed.
For differential diagnosis and selection of adequate therapy, it is necessary to contact a specialist at the first manifestations of the disease.
Gargling with antiseptics, herbal decoctions, inhalations, and treatment of the mucous membrane with antiseptic solutions are mandatory.
Local treatment for sore throat is no less important than general treatment. Medications are used to relieve symptoms: painkillers, antipyretics, antitussives, and runny nose medications. Sore throat is accompanied by a runny nose and cough in the case of a secondary bacterial infection.
Cough and rhinitis are not typical for this pathology. It is strictly not recommended to remove purulent plugs from the tonsils on your own, as this can lead to complications (for example, an abscess, bleeding from the tonsils)
A sore throat is accompanied by a runny nose and cough if a secondary bacterial infection is attached. Cough and rhinitis are not typical for this pathology. It is strictly not recommended to remove purulent plugs from the tonsils on your own, as this can lead to complications (for example, an abscess, bleeding from the tonsils).
Treatment of purulent sore throat
Purulent tonsillitis threatens serious complications from the heart, kidneys, joints and soft tissues of the neck if therapy is chosen incorrectly or treatment is started late. It is for this reason that it is important to immediately consult a doctor when the first signs of a sore throat appear.
The basic treatment regimen for acute tonsillitis with purulent exudate:
- Taking antibiotics of the penicillin group or the macrolide group. You can't do without them. General and local remedies are prescribed. Antibiotics kill pathogenic microflora and after a few days the production of pus stops, blood circulation in the tonsils is restored.
- Taking anti-inflammatory lozenges, lozenges, lozenges.
- Gargling and irrigating the throat with different solutions every hour.
- Use of local antiseptics in the form of a spray.
- Taking antipyretic drugs.
- Vitamin therapy and taking immunomodulators.
The principle of treatment of acute tonsillitis in children is similar, the only differences are in the dosage of medications. The patient needs to observe strict bed rest, talk less and gargle more often.
If the prescribed drug therapy does not have positive dynamics within several days, the patient continues treatment in the hospital.
Due to the presence of purulent plaque on the palatine tonsils, eating is difficult or completely impossible, so you can eat only pureed and liquid food, and also drink a lot of warm water to relieve symptoms of intoxication.
What leaves tonsillitis on the tongue and teeth?
What effect does tonsillitis have on the tongue and teeth, and what measures should be taken?
A healthy oral cavity is of great importance for the entire body. Bad teeth can cause the development of many diseases. Chronic tonsillitis sometimes causes negative changes in the oral cavity, since the body cannot cope with pathogenic microbes on the tonsils and their aggression.
Gray and white coating on the tongue with tonsillitis
Tonsillitis contributes to the development of various concomitant diseases. This disease is characterized by a particularly negative effect on the tongue. If tonsillitis develops on the tonsils, a coating may appear on the tongue. This area on the tongue will become painful and turn bright red. The tongue with chronic tonsillitis has a heterogeneous gray coating. The inflammatory process affects the pharyngeal ring and tonsils, and they are located between the palate and the tongue. Pain in the tongue indicates inflammation of the tonsils.
photo of white plaque on the tongue with tonsillitis
Inflammation of the tongue is not a rare occurrence in the acute form of the disease. When tonsillitis develops, the tongue may become slightly swollen and have a white coating. The presence of a white coating on the tongue during tonsillitis is caused by inflammation of the tongue and is felt as an unpleasant burning sensation, which intensifies when irritated by food. Any changes in the mucous membrane of the tongue should be immediately examined by a doctor to further prescribe the correct treatment.
The effect of tonsillitis on teeth
Inflammation of the tonsils has a direct effect on the teeth. An infection located on the tonsils is easily transferred to the teeth. As a result, caries occurs, the tooth begins to decay and inflammation develops. Chronic diseases of the mouth, including tonsillitis, very often cause caries. When a doctor diagnoses tonsillitis, teeth must be carefully protected.
Caries is directly related to chronic tonsillitis. First, the infection transfers to the teeth, and then the carious teeth affect the tonsils. That is why doctors prescribe complex treatment of the oral cavity and pharynx. When tonsillitis is completely cured and the teeth are checked by a dentist, only then is the oral cavity completely healthy.
To prevent the inflammatory process in the tonsils from affecting the tongue and teeth, it is necessary to take some preventive measures
If you have tonsil disease, it is important to rinse your mouth with various antibacterial compounds. It is better to use the healing solution 2-3 times a day. It will eliminate the infection developing in the oral cavity
It will eliminate the infection developing in the oral cavity.
Share “What does tonsillitis leave on the tongue and teeth?”
Causes of white spots on the tonsils in a child
The tonsils affected by white plaque are unable to perfectly perform their protective functions. This leads to the appearance of serious pathologies. To completely cure the disease, it is necessary to eliminate the cause of the formation of whitish spots.
If there is a temperature
If, in addition to white dots on the tonsils, the child’s body temperature is elevated, you should consult a pediatrician. Such symptoms may indicate a serious illness. Without treatment, the condition will only worsen; the pathology can lead to a number of complications and become chronic.
If a child has an elevated body temperature, then whitish spots on the tonsils can be caused by:
- Sore throat (acute tonsillitis). In addition to whitish spots, ulcers may be present. With a sore throat, the throat becomes red and sore, and the temperature rises to 39 degrees.
- Chronic tonsillitis. The disease develops as a result of prolonged inflammation of the tonsils after viral infections, which were accompanied by inflammation of the pharynx.
- Flu, ARVI or pharyngitis. The first symptoms of these pathologies appear in children on the tonsils in the form of white dots.
- Diphtheria. Whitish spots on the tonsils are combined with temperatures up to 40 degrees. Advanced cases can provoke the appearance of cardiovascular problems or disturbances in the functioning of the nervous system. Diphtheria is an infectious contagious disease. Therefore, a sick child must be hospitalized and isolated from contact with others.
Parents may also notice white dots in the baby’s mouth due to scarlet fever.
If there is no temperature
It happens that whitish spots on the tonsils are not accompanied by elevated temperature. This happens when food particles get into the loose tonsils. Thorough rinsing of the mouth quickly eliminates the problem. But it happens that plaque is a symptom of a serious illness.
Reasons for the appearance of white dots on the tonsils at normal body temperature:
- Stomatitis. In addition to plaque in the child, there is an increase in the submandibular lymph nodes and increased salivation. Erosion and ulcers form on the tonsils. Stomatitis is provoked by injuries, allergies, hypothermia, and low immunity. The disease is complicated by gangrene, loss of voice, and tooth loss.
- Candidiasis. Fungal infection can be a complication after therapy with antibacterial agents. Antibiotics not only inhibit pathogens, but also destroy beneficial microflora. This causes the proliferation of yeast-like fungus to become more active. Candidiasis is characterized by the formation of a white cheesy coating and ulcers on the tonsils.
- Leukoplakia. It manifests itself as keratinization and thickening of the oral mucosa. This process can take a malignant form. In addition to white spots on the tonsils, there are ulcers.
There is no point in trying to independently determine and eliminate the cause of the appearance of dots on a child’s tonsils. To avoid worsening the situation, it is better to take your baby to see a pediatrician.
Sore throat is dangerous because it can lead to serious complications from the gallbladder, heart, blood vessels and kidneys.
Clinical picture
Once a pathogen enters the body, two hours are enough for it to spread. Streptococci settle on the tonsils, weakening local immunity. The incubation period varies from several hours to 5 days.
The main differences between purulent tonsillitis are symptoms:
- A sharp pain in the throat occurs, which causes discomfort even at rest. The next day she becomes unbearable when talking or eating.
- Within a few hours, the body temperature rises to 39-40°C. Against the background of high temperature, it throws you either hot or cold, sweating increases and chills are present.
- Swallowing saliva causes severe, sharp pain.
- There is not enough air when breathing due to swelling of the tonsils.
- When examined with the naked eye, swollen tonsils and severe hyperemia of the back wall of the throat are visible. The next day the tongue and palate swell.
- There is a sensation of a foreign body in the nasopharynx, which intensifies when saliva is swabbed.
- Due to the fact that the tonsils are well supplied with blood, a yellowish-white dot appears on them, the boundaries of which quickly expand. The next day, the throat may become covered with many white purulent dots, which gradually merge into large ulcers.
Purulent tonsillitis in children occurs in a more severe form. Due to the excessive pressure of the swollen lymphoid tissue of the adenoids on the Eustachian tubes, the ears become blocked and there is tinnitus. If treatment is not attempted, the infection can spread to the ears, complicated by otitis media.
Usually the acute period lasts no more than one week if treatment is prescribed on time.
Important to know and remember! Purulent tonsillitis is a dangerous infectious disease, so the patient should be immediately isolated from household members.
How to remove plaque from tonsils?
Having seen the film on the tonsils, many patients wonder - how to remove plaque from the tonsils with a sore throat? It is contraindicated to specifically remove plaque or remove ulcers. For this procedure, many patients lubricate the throat with various antiseptics using cotton swabs, but such manipulations should not be carried out. Such procedures only increase the likelihood of a bacterial infection connecting to an existing sore throat. The chances of introducing pathogenic microorganisms to the inflamed mucous membrane greatly increase, so it is not worth conducting such home “experiments”.
Plaque can only be removed with the help of a doctor, who will clear the throat with sterile instruments and in a sterile room. With proper treatment, the plaque will come off on its own.
Expert opinion
As an ENT specialist, I want to say that catarrhal tonsillitis is a very common disease with an increase in incidence in the autumn-winter period. Due to the decrease in air temperature and the spread of respiratory infections, the number of sick children is increasing. However, the pathology responds well to conservative treatment. The main thing is not to ignore the signs of the disease and seek help from a specialist as early as possible. Self-treatment risks progression of the disease and the development of dangerous complications.
Medicinal solution to the problem
Before prescribing the necessary medications, the cause of the disease should be determined. This will make it possible to choose the right remedy that will help you quickly get rid of not only the signs of the disease, but also its causes. If a sore throat is infectious, your doctor may prescribe antibiotics. Antibacterial and antiviral drugs are also selected. Sometimes the patient requires surgery.
Medicines are prescribed in combination with rinsing, sprinkling, and cleansing the mouth. Suppuration is best removed by rinsing. The most popular rinse is furatsilin tablets. To carry out the procedure, you need 1 tablet of the product, dissolved in warm water. To eliminate the effects of microcrystals on the tonsils, it is worth straining the solution. The throat should be rinsed for 5 minutes, every 2 hours.
Chlohexidine is also prescribed. It removes germs and relieves pain, preventing the spread of infection. For rinsing you need 1 large spoon of product. Antiseptic stopangin is used undiluted, 1 tablespoon. Gargle with chlorophyllipt 3 times a day, dissolving 1 teaspoon in a glass of warm water.
To remove plaque, you can use disinfectant solutions, treating the tonsils and oral cavity with them. It is necessary to make tampons from cotton wool or a bandage, soak them in peroxide and thoroughly wipe the tonsils and oral cavity. The procedure is carried out until the plaque is removed. In this way, pus is removed using:
- oily chlorophyllipt;
- Lugol's solution;
- stomatidine.
Frequent sore throat in a child: causes, how to treat?
Causes of the disease
The most common type of this pathology in childhood is bacterial tonsillitis. It is usually caused by group A beta hemolytic streptococcus or staphylococcus. In second place are viral sore throats. The cause of their occurrence is such types of viruses as Coxsackie enterovirus, adenoviruses, and herpetic viruses. In third place are fungal diseases. They are caused by fungi of the Candida family. Provoking factors in the development of the disease in a child are a decrease in general or local immunity.
Symptoms of the disease
Bacterial sore throats most often occur with severe intoxication. In a general blood test, in this form of the disease, significant leukocytosis, increased ESR and a high content of neutrophils are observed.
Viral sore throats, or herpangina, are very common in children, especially in the summer. Clinically they manifest themselves as follows:
- very severe intoxication;
- chills, fever;
- sore throat.
Small, red rashes on the tonsils, soft and hard palate are also characteristic. They may burst and disappear spontaneously within 3-5 days.
As for fungal tonsillitis, the clinical picture is often moderate. High fever is rare, and a characteristic cheesy coating is present on the tonsils.
What are the possible complications?
Untimely or unqualified treatment of the disease can lead to a number of complicated consequences. Among which the most common are:
- otitis media;
- phlegmon of the neck;
- sinusitis;
- acute lymphadenitis.
If we talk about dangerous complications, the early ones include: infectious-toxic shock, sepsis, meningitis, pharyngeal abscess. They occur in the first days of the disease. And in the later period, lymphatic fever may develop, which we have heard a lot about as rheumatism, sinusitis, nephritis. These are pathologies of vital organs - heart, kidneys. Unfortunately, they can lead to disability of the child and serious complications to the baby’s health.
Therefore, experienced pediatricians at children's medical centers are always very afraid of the development of complications of streptococcal sore throat, and in this situation it is imperative to prescribe antibiotics.
Marshall syndrome in children
Imagine the condition of parents whose child suffers from a sore throat every month. We are talking about Marshall syndrome, which many treated like a regular sore throat. And the baby received a monthly dose of antibiotics. In fact, antiviral and antibacterial drugs are absolutely ineffective for this pathology. The only effective method of treating the disease in this case is the use of glucocorticosteroid drugs such as Prednisolone or Dexamethasone. But this does not guarantee that in a month the child will not again develop symptoms of Marshall syndrome. The radical treatment method in this case is removal of the tonsils.
When is it necessary to remove tonsils?
Experts recommend removing tonsils in children if:
- your child suffers from sore throats more than four times a year;
- conservative therapy does not help;
- disorders of the heart, kidneys, and joints are noted;
- the child has a violation of nasal breathing, a deformation of the facial part of the skull is formed, and the habitus is disrupted;
- frequent otitis occurs;
- the disease is complicated by an abscess.
But before deciding on surgical removal of the tonsils, a mandatory consultation with an ENT doctor is necessary. If complications develop, consultations with a nephrologist and cardiologist will also be required.
Correct diagnosis
The necessary competent examination by the attending physician begins with a general blood and urine test. It is also necessary to take a swab from the throat for a nutrient medium. This study is carried out over several days. At home, you can use a special product called “streptatest”. It is sold in pharmacies, the instructions are very detailed and clearly describe how to use it. The result will be ready within 5 minutes. If it comes back positive, it means you need to use an antibiotic right away.
The next test to determine the presence of viruses is a polymerase chain reaction (PCR) test. Currently, this method is considered highly accurate, and in our Healer clinics you can come and carry out all the necessary tests in one place. At a high professional level, our experienced laboratory doctors will qualitatively examine your child and give you absolutely correct, reliable results that will help cure your baby.
I wish your children and you good health. To prevent the pathologies that I described above, I recommend hardening your children. This procedure allows you to boost the body’s immune system, which in turn prevents the development of various chronic lesions, as well as the occurrence of sore throat in a child.
How to remove plaque on tonsils?
After consulting with your doctor and determining the cause of the plaque, you can begin to treat it. You can remove plaque on the tonsil by rinsing the throat with antiseptic drugs dissolved in warm water, such as Furacilin, Nystatin or methyl blue.
The drug Hydrocortisone in tablet or cream form helps eliminate lichen planus, which can also cause a buildup on the glands. If the cause is candidiasis, then the layering is removed with universal antifungal agents.
Pain and sore throat accompanying inflammation of the tonsils can be relieved by lozenges with an analgesic effect - Decathylene, Septefril, Faringosept.
Washing the tonsils in a hospital is the most effective method to get rid of white plaque. An otolaryngologist will help eliminate the problem by manipulating the use of an antibacterial solution, which enters the lacunae with a strong stream, cleaning them. As a rule, it is necessary to do up to 10 similar procedures within a month to completely eliminate the problem. They also use vacuum washing - the plaque is quickly removed and plugs can be removed under pressure.
You can also remove the layer at home - a piece of bandage or a cotton swab moistened with an antiseptic, wrapped around a pencil and made in a circular motion to remove the pus. You can also use a large moistened cotton swab for this purpose. In this way, only the surface film can be removed; the lumps in the gaps remain untouched.
Oral candidiasis
Since Candida fungi are constantly present on the mucous membrane, but cause disease only under certain conditions (immunodeficiencies, taking antibacterial drugs, early cessation of breastfeeding, poor hygiene, etc.), oral candidiasis is an autoinfection. Plaque with this disease can be:
- dotted, islanded or solid;
- foamy, curdled, filmy;
- white, yellowish.
Sore throat with candidiasis is usually not intense. The exception is a severe form of the disease, in which plaque covers the entire surface of the mucous membrane of the oropharynx, is tightly fused to it and is difficult to remove. The layers take the form of films, the surface of which is dirty gray, and the lower layers remaining after partial removal are white.
In mild to moderate forms, the pain is moderate and accompanied by dryness in the mouth and throat. In the first case, the plaque is localized only on the tongue and/or cheeks; it is easy to remove, after which the reddened, intact mucous membrane is exposed. In the second case, fungi affect not only the superficial, but also the deep layers of the epithelium. The layers are located on the tongue, cheeks, hard palate, lips, it is difficult to remove them; when trying to do this, the mucous membrane is damaged and sometimes bleeds.
The leading symptom of the classic course of oral candidiasis is a cheesy white or yellow coating in the oral cavity (including on the tongue).
For a more accurate description, there is a comparison of the layers with curdled milk. More common are mild forms of the disease, which are characterized by limited, sometimes focal, lesions.
The following treatment options are used to help the patient:
These are various types of antibacterial drugs (Amoxicillin, Cefuroxime) for bacterial pharyngitis and tonsillitis, antitoxic anti-diphtheria serum for diphtheria, antifungal agents (Diflazol, Diflucan) for candidiasis. Local antiseptics, antibiotics and antimycotics in tablets, sprays, solutions (Anzibel, Bioparox, Ekalin) are also used.
- Pathogenetic and symptomatic.
This group includes anti-inflammatory drugs - usually topical (Tantum Verde, Isla-moos), antipyretics (Ibuprofen, Paracetamol), painkillers (Strepsils Intensive) drugs. Gargling (chamomile decoction, tincture of calendula, sage, Chlorhexidine) is also recommended.
- Correction of regime, nutrition.
Bed rest is necessary for fever, eating only warm, comfortable temperature foods and drinks, humidifying the air in the room where the patient is, stopping smoking and alcohol.
In severe cases of any disease with damage to the oropharynx and tonsils, hospitalization and detoxification therapy (sodium chloride solution, glucose, Dextrose, Reopoliglucin) are necessary. The treatment of oral candidiasis includes probiotics (Bioflor, Bifinorm), while limiting the amount of carbohydrates in the diet.
Treatment of diphtheria is carried out only in an infectious diseases hospital.
There is no need to specifically clean or wash off plaque:
The presence of plaque on the tongue of a patient who is bothered by a sore throat cannot be considered a sufficient sign to make a diagnosis. It is necessary to evaluate all the symptoms that are identified during the survey and examination, as well as during laboratory and instrumental studies. It is worth understanding that in some cases you may encounter not a classic, but an atypical form of the disease, in which the main manifestations will look different from what was expected. Only a doctor should prescribe treatment, especially if the patient is a child.
2016—2017, OOO "Studi Group"
Any use of site materials is permitted only with the consent of the portal editors and by installing an active link to the source.
The information published on the site is intended for informational purposes only and in no way calls for independent diagnosis and treatment. To make informed decisions about treatment and medications, consultation with a qualified physician is required. The information posted on the site is obtained from open sources. The portal's editors are not responsible for its accuracy.
Higher medical education, anesthesiologist.
Doctor of the highest category, pediatrician.
Treatment of the disease
In most cases, treatment is carried out on an outpatient basis. Patients are prescribed bed rest, warm, plenty of fluids, and food should be light and liquid. Treatment, depending on the type of sore throat, includes antibacterial therapy, antiviral drugs and local symptomatic treatment. Additionally, the tonsils are irrigated with anti-inflammatory drugs, gargling with herbal decoctions and antiseptic solutions. To reduce swelling and symptoms of intoxication, antihistamines are indicated. The course of treatment is 5-10 days.
“Plaque on the tonsils” is observed in diseases:
Lacunar tonsillitis is an acute illness of an infectious nature, characterized by local inflammation of one or several elements of the lymphadenoid ring of the pharynx. Usually the inflammation covers the tonsils, but damage to the larynx and pharynx is also possible. This disease can be provoked by pathogenic microorganisms, including meningococci, streptococci, hemophilus influenzae, etc. The disease has no restrictions regarding gender and age.
Streptococcal infection is a group of diseases that causes pathological processes in the respiratory tract and skin. Infections of this type are present in the body of a healthy person. The development of the disease is possible only if there is a favorable environment for this. Children and pregnant women are most susceptible to the disease.
Follicular tonsillitis is a disease characterized by purulent inflammation of the follicles of the tonsils. If such a disease progresses, pus is located on the surface of the lymphoid formations of the pharynx in the form of separate pinpoint foci. The pathological process can affect the pharyngeal, palatine, tubal and lingual tonsils. The progression of follicular tonsillitis is accompanied by regional lymphadenitis and severe hyperthermia.
Description of the disease
Catarrhal tonsillitis is clinically the mildest form of the inflammatory process that can occur in the palatine tonsils.
In pediatrics, it occurs in children aged 6 months to 18 years. The disease responds well to drug treatment if you consult a doctor in a timely manner. The pathology belongs to the group of tonsillitis. The palatine tonsils are the first barrier to the penetration of infection deeper into the respiratory tract, and therefore are often affected by the inflammatory process. Depending on the nature of the disease, angina can be acute or chronic. The severity of the inflammatory process varies.
- Catarrhal sore throat. This is the mildest form, in which the child’s general well-being deteriorates slightly.
- Follicular. The pathological process is accompanied by a pronounced disturbance of well-being.
- Lacunarnaya. This is a severe variant of follicular tonsillitis with high fever and massive damage to the tonsils.
- Membranous-necrotic. A critical condition that can cause acute airway obstruction.
Catarrhal tonsillitis in children can occur without complications (94-95% of cases) or with the development of undesirable consequences - tonsillar abscesses, exacerbation of chronic diseases, and the addition of a secondary infection.
Frequent catarrhal tonsillitis at an early age indicates a reduced barrier function of the tonsils. This threatens the process becoming chronic with the formation of a persistent focus of infection in the pharynx. A possible result of this development of events is acute rheumatic fever with damage to the heart. In particular, the heart valves suffer, and intracardiac hemodynamic disturbances (stenosis, regurgitation) occur.
The best way to prevent complications from occurring is to promptly contact an ENT doctor if you have any suspicious symptoms.
Reasons for the raid
The reasons may be different, but the main one is the proliferation of viruses and bacteria in the nasopharynx. It can occur due to diseases such as:
- tonsillitis (purulent ones are common);
- ARVI;
- tonsillitis;
- pharyngitis (both viral and bacterial);
- candidiasis in the oral cavity;
- diphtheria is a serious illness requiring hospitalization;
- scarlet fever;
- stomatitis;
- mononucleosis;
- lichen planus;
- leukoedema;
- chemical burns from medications;
- syphilis.
Harmful organisms can enter the nasopharynx either through airborne droplets or due to non-compliance with hygiene rules and consumption of unwashed foods.
As soon as you notice purulent inflammation of the tonsils, consult a doctor.
To establish a clear diagnosis, you need to immediately conduct a comprehensive examination of the body, taking into account the symptoms that appear.