Tonsillitis is an infectious disease characterized by inflammation of the tonsils. The disease can have both acute and chronic forms. Chronic tonsillitis is diagnosed in 15% of children and 10% of adults. Another name for tonsillitis is tonsillitis, which literally translated from Latin means “squeezing”, “suffocation”. Indeed, the main symptom of a sore throat is a sore throat and discomfort when swallowing. The term "angina" is often used by both medical professionals and patients.
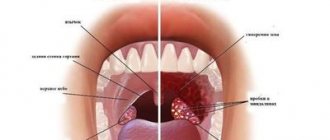
Classification of forms of tonsillitis (tonsillitis)
- I catarrhal form (the inflammatory process is manifested by redness and swelling of the tonsils).
- II follicular form (yellowish purulent dots appear on the surface of the tonsils - festering follicles).
- III lacunar form (liquid pus or purulent-caseous plugs form in the lacunae).
- IV fibrinous form (characterized by the formation of a single continuous plaque of a whitish-yellow color, which can extend beyond the tonsils, often occurs in people with reduced immune system function).
- AIDS, blood diseases, hunger, old age.
- V herpetic form (most often caused by adenoviruses, herpes simplex viruses, characterized by vesicular rashes on the back of the pharynx or soft palate, predisposed to ulceration).
- VI phlegmonous form (intratonsillar abscess) is a complication of acute tonsillitis (lacunary, catarrhal, follicular) or chronic tonsillitis, which is an acute purulent inflammation of the peritonsillar tissue.
- VII ulcerative-necrotic form (gangrenous form) - characterized by the formation of yellow-white blisters (ulcers) on the tonsils, in some cases the spots spread to the entire oral cavity and throat.
- VIII mixed forms (a variant of the disease in which colonization of lymphoid tissue occurs by several pathogens at once, as a result of the addition of a secondary infection or with a severe decrease in immunity).
Norm and pathology
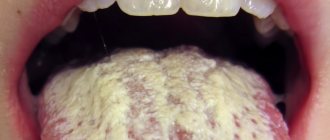
Language is a kind of mirror of the functioning of the body. When it is clean, pink, with visible taste buds, the person is healthy and most likely does not suffer from bad habits. But even a loose white coating, through which the surface of the tongue is visible, is considered as a variant of the norm. It can change shade depending on the time of year: in summer it can be more intense due to hot weather, in winter it becomes white-yellow, in autumn it becomes almost transparent. In addition, a yellow coating on the tongue in the morning appears in heavy smokers and those who drink too much coffee.
However, a change in the color of the tongue may be a consequence of malfunctions in the internal organs, mainly the liver, kidneys, stomach, pancreas and gall bladder. If the plaque has become dense, thick, bright yellow or brownish-yellow, and there is also bad breath, you should consult a doctor and identify the cause of the problem.
Attention!
Typically, “safe” soft deposits come off easily and, if brushed well, will not reappear. But if the plaque returns, we are dealing with pathology.
Complications of tonsillitis (tonsillitis)
Sore throat is one of those diseases that cannot be endured “on your feet”.
Indifference to your health if you have a sore throat is criminal; hoping for help from “folk remedies” and medicines from the home medicine cabinet of your friends and acquaintances is, to say the least, short-sighted. The question of treating sore throat is precisely the correct treatment. If the patient receives inadequate therapy for tonsillitis, complications may include various heart defects, kidney disease, joint damage, the transition of the inflammatory process to surrounding tissues with subsequent formation of abscesses, otitis (inflammation of the middle ear), laryngitis (inflammation and swelling of the larynx), as well as others diseases (tonsil abscess, paratonsillitis, phlegmon, meningitis, mediastinitis, purulent lymphadenitis, tonsillar sepsis, etc.).
Causes of yellow coating on the tongue
- Poor functioning of the gastrointestinal tract.
The most common reason for the appearance of an unpleasant plaque, which can indicate either a mild ailment or a serious illness. As a rule, the issue is resolved by correcting the diet, that is, switching to a more gentle regime and giving up fatty and fried foods.
If the plaque is dense and has an unpleasant odor, then the cause is diseases of the digestive system (pancreatitis, gastritis, ulcers).
- Diseases of the liver, gall bladder, kidneys.
Excessive consumption of fatty and fried foods impairs the flow of bile, which disrupts liver function. Characteristic signs of liver and gallbladder diseases are a yellow coating on the tongue and a metallic taste in the mouth.
- Reaction to antibiotics.
Some medications increase the load on the liver and digestive organs. Since antibiotics kill not only harmful but also beneficial bacteria, to prevent dysbiosis, fermented milk products, prebiotics and probiotics are added to therapy.
- Viral and respiratory diseases.
Yellow plaque can be a consequence of infectious (whooping cough, scarlet fever, etc.) and respiratory (sore throat, pharyngitis, etc.) diseases. During illness, immunity decreases, which is why bacteria settle in the oral cavity, including on the tongue.
Treatment of sore throat at GUTA CLINIC
Treatment of tonsillitis in our clinic is carried out comprehensively, drug therapy is prescribed individually, both antibacterial and immunomodulating, decongestants, antihistamines are used, as well as physiotherapy (rinsing, washing, irrigating the tonsils with various medications).
Treatment of abscesses is only surgical followed by rehabilitation therapy. Otorhinolaryngologists at GUTA CLINICS recommend that at the first symptoms of tonsillitis - difficulty swallowing, pain and discomfort in the throat, redness of the tonsils, fever, changes in sense of smell, taste, voice - contact a specialist. Don't let your sore throat progress and stay healthy!
Publications in the media
Secondary tonsillitis is an acute inflammation of the components of the lymphatic pharyngeal ring (usually the palatine tonsils), caused by a systemic disease: infectious or hematological pathology.
SONGINS IN INFECTIOUS DISEASES
Sore throat with measles • Damage to the mucous membrane of the pharynx occurs in the prodromal period and the period of rashes • Belsky-Filatov-Koplik spots are found on the mucous membrane of the cheeks • Measles enanthema • Characteristic skin rash • Pharyngoscopic picture varies from catarrhal tonsillitis to a necrotic process.
Diphtheria sore throat (diphtheria of the throat) is the most common form of diphtheria.
• Clinical picture •• Acute onset •• General intoxication - headache, malaise, loss of appetite, adynamia, increased body temperature •• Pale skin •• Enlarged regional lymph nodes •• Severe sore throat, usually worsening on the 2nd day diseases.
• Pharyngoscopy •• Swelling of the palatine tonsils and arches, mild hyperemia with a cyanotic tint •• In the depths of the lacunae (island form) and/or on the surface of the tonsils (membranous form), plaque is found in the form of films of grayish-yellow or yellow-white color, plaque appears by the end of 2 days of illness. The films are thick, difficult to remove, leaving a bleeding surface, do not rub on a glass slide, and sink in water. After removing the film, new plaques form in its place •• Plaques on the tonsils persist after body temperature normalizes and symptoms of intoxication disappear (important for the retrospective diagnosis of untreated diphtheria and the prevention of complications - myocarditis, paresis of the soft palate, etc.).
• In cases of sore throat accompanied by the formation of plaque, it is necessary to first suspect diphtheria of the pharynx. Negative results of a bacteriological test for diphtheria are not considered sufficient grounds to cancel the clinical diagnosis of diphtheria.
Sore throat with scarlet fever • Clinical picture •• Inflammation of the mucous membrane of the pharynx from catarrhal to necrotic •• Characteristic is the appearance of scarlet fever enanthema already at the end of the prodromal period, i.e. before scarlet fever exanthema •• Typical appearance of the patient - “scarlet fever mask”: bright blush, pallor of the nasolabial triangle •• Regional lymph nodes are enlarged, painful • Pharyngoscopy •• Severe widespread hyperemia of the palatine tonsils and hard palate with distinct boundaries •• Swollen and hyperemic palatine a tongue that looks like a “crushed cranberry” •• The palatine tonsils are sharply enlarged, hyperemic, their changes correspond to follicular or catarrhal tonsillitis. Grayish-yellowish plaques appear on the tonsils, sometimes merging and covering the entire tonsil. The plaques are tightly fused to the surface of the tonsil, but do not rise above it.
Angina in tularemia occurs in its tonsillar-bubonic form • Clinical picture •• The first 2 days of changes in the tonsils are catarrhal in nature, from the 3rd day - membranous or necrotic •• Regional lymphadenitis - posterior cervical and submandibular lymph nodes increase in size within 1– 3 days, merge to form a tularemic bubo (the size of a nut to a goose egg) •• The conglomerate of lymph nodes is not fused with the surrounding tissues, is not painful, is prone to suppuration and the formation of fistulas •• The process is usually one-sided •• Healing is slow, from 2 –3 weeks to 3–6 months, with the formation of a keloid scar • Pharyngoscopy: the tonsils are enlarged in size, covered with a grayish-white coating. In the necrotic form, the plaque has a dirty gray color, is clearly demarcated and is located below the level of healthy tissue • Diagnosis: detection in smears taken from areas of necrosis and in the lymph nodes of Francisella tularensis.
Sore throat with typhoid fever • Clinical picture •• As an initial symptom of the disease, sore throat occurs in 50–70% of cases •• In the prodromal period - a rise in body temperature •• Moderate pain in the throat •• Lymph nodes are enlarged on the affected side, painful on palpation • Pharyngoscopy : at the beginning of the disease there is a picture of catarrhal tonsillitis, then in the 2nd week a unilateral painless ulcerative-necrotic lesion of the tonsil may occur with the formation of small round ulcers with smooth red edges and a grayish bottom, spreading to the palatine arches. After 4 weeks, areas of granulation tissue appear, followed by epithelization.
Monocytic tonsillitis (angina with infectious mononucleosis) is an acute infectious disease characterized by monocytosis in the blood and typical changes in the pharynx • Etiology: primary infection with the Epstein-Barr virus in adolescence or older • Clinical picture •• Acute onset with chills, headache and a sharp rise in body temperature to 40 °C and above •• Sore throat •• Enlargement (usually symmetrical) and tenderness of the submandibular, cervical and occipital lymph nodes •• At the height of lymphadenitis, changes appear in the pharynx. In the initial stages, the changes are in the nature of catarrhal or follicular tonsillitis, later they resemble diphtheria tonsillitis (in two thirds of cases of monocytic tonsillitis, diphtheria is mistakenly diagnosed) •• Severe swelling of the mucous membrane of the pharynx and lymphadenoid ring occurs, incl. and nasopharyngeal tonsil, which leads to difficulty in nasal breathing, nasal sound, a feeling of stuffiness in the ears •• The liver is enlarged, protrudes from under the edge of the costal arch, may be slightly painful on palpation •• The spleen is enlarged, dense, painless •• Plaques on the tonsils persist for a long time (up to several weeks and even months), sometimes recur • Laboratory signs - leukocytosis 10–20´109/l or more with a predominance of atypical mononuclear cells (up to 60–80%).
ANGINA IN DISEASES OF THE BLOOD SYSTEM
Sore throat with agranulocytosis • Clinical picture •• Increased body temperature to 39–40 °C with chills, intoxication, severe general condition •• Severe sore throat •• Drooling •• Putrid breath •• At the height of the disease, hemorrhagic syndrome develops: bleeding gums, nosebleeds, skin hemorrhages •• Stomatitis, gastrointestinal lesions • Pharyngoscopy. Changes in the pharynx are often localized on the tonsils, are ulcerative-necrotic in nature and spread to the mucous membrane of the pharynx, gums, and larynx. In the blood, the number of all forms of leukocytes (up to hundreds of cells in 1 μl), platelets and reticulocytes is sharply reduced. The number of plasma cells is increased.
Sore throat in leukemia • Clinical picture - signs of sore throat that appear on the 3-5th day of acute or exacerbation of chronic leukemia • Pharyngoscopy. Changes in the tonsils first correspond to catarrhal tonsillitis, later hemorrhagic, ulcerative-necrotic or gangrenous lesions occur. Necrosis spreads to the mucous membrane of the mouth, gums and pharynx. The plaque formed on the surface of necrotic areas has a dirty gray or brown color; when it is rejected, a bleeding, eroded surface is exposed. Regional lymph nodes are enlarged.
TREATMENT • Sore throats due to infectious diseases - hospitalization in an infectious diseases hospital. Etiotropic, pathogenetic and symptomatic therapy. Therapeutic and disinfectant rinses • For diseases of the blood system, treatment is carried out in a therapeutic or specialized hematology department.
ICD-10 • J03.8 Acute tonsillitis caused by other specified pathogens