Inflammatory gum disease in adults and children is called gingivitis. It is most often observed in children a few months from birth to 13 years of age, which is explained by the characteristics of the child’s body and poor oral hygiene.
According to statistics, in a child from 2 to 4 years old, gum inflammation occurs in 2% of cases, and by the age of 13, the proportion of this disease in children reaches 80%. Gingivitis cured in time does not become chronic, but if left untreated it can cause the development of periodontitis.
Causes of gingivitis in children
There are many causes for childhood gingivitis. The gums become inflamed due to the functional immaturity of their tissues. In babies under one year of age, the cause of the disease is often teething, when the gums become red and sore. Sometimes inflammation is caused by an allergic reaction to food.
In adolescents, the disease may manifest itself due to the eruption of a permanent tooth. When soreness during brushing does not allow this procedure to be performed efficiently, microbes multiply and gum inflammation develops.
The most common factors that provoke the development of gingivitis in older children are:
Action of microbes
In 90% of cases, the disease appears in a child due to insufficient oral hygiene, as a result of which microorganisms multiply intensively, plaque and tartar form, and stomatitis develops.
Mechanical injury
The integrity of the mucous cavity can be compromised by teething, cuts, scratches, burns, biting, improper brushing of teeth, and eating solid foods.
Foci of infection in the oral cavity
If children have carious teeth, there is a chance that they will develop infectious gingivitis, which affects the gums. Therefore, teeth that require treatment must be treated as soon as possible.
Excessive loads on the dental system
Other causes of gum damage in children may include:
- presence of malocclusion;
- poor nutrition with a lack of vegetables and fruits;
- uneven load on the dental system due to bad habits;
- defects of the oral cavity (short frenulum of the tongue, lips);
- the presence of caries, various infections;
- thermal burn from hot food;
- wearing braces.
Reasons for appearance
Opportunistic bacteria are part of the oral microflora of every person. Age doesn't matter here. Thrush appears when fungi, like yeast, become active and exceed the permissible number. Also, pathology is formed when pathogenic strains enter the patient’s body. The reason that leads to problems may be internal. Also, negative environmental factors influence deterioration of health. Often, anomalies are caused by non-compliance with hygiene rules, intestinal problems and others.
To prevent serious complications, you should consult a doctor promptly. A dental clinic that has modern equipment and uses the latest technologies will help you understand the problem and eliminate it. Advances in dentistry allow you to achieve results quickly. Having identified the true cause of the problem, the dentist will draw up a treatment plan. The problem will be solved when the provoking factor is eliminated.
Candidiasis in the oral cavity
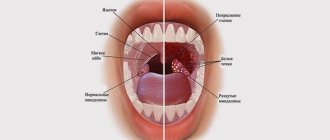
This inflammatory disease is often diagnosed in children. It can affect a newborn. The basis of the disease is pathogenic fungi. They provoke damage to the mucous layer, and the uvula suffers. Candidiasis is suppressed by the defenses of a healthy toddler. But when fungi multiply quickly, the immune system cannot cope with them, as it weakens. The pathology progresses against the background of the following problems:
- Inflammatory processes in internal organs;
- Colds;
- Hormonal instability;
- Problems with the gastrointestinal tract;
- Long-term treatment with antibiotics;
Children's fragile immunity cannot withstand negativity. All this leads to imbalance. White palate in a baby’s mouth can appear due to severe stress, which reduces the body’s immune strength. The growth of fungi is provoked by excessive dryness of the mucous membranes and an imbalance of acid balance. The first sign of damage to the mucous membrane is itching. At risk are those guys who wear braces, are treated with hormonal drugs, and do not clean their chewing organs well. The disease develops especially quickly when unfavorable factors are combined. The baby's mucous membrane is covered with a cheesy film. Whitish crumbs are difficult to remove; ulcers form underneath them. They may bleed.
Infectious lesions
When the body's resistance decreases, the appearance of pathogenic bacteria is often associated with the appearance of one or another infection. As a result, white spots develop on the palate.
- Fungal strains are highly infectious. Pathogenic microbes quickly colonize the damaged mucosa.
- With scarlet fever, the baby's mouth turns red, a rash appears, and the temperature rises.
- With diphtheria, the film has dirty inclusions.
- With whooping cough, a putrid odor from the mouth is clearly heard.
- With dysentery, the layer is dense, and erosions appear underneath it.
Oral diseases
Oral problems cannot be ignored. Parents should immediately show the toddler to the pediatrician, who will refer the child to the dentist. Pediatric dentistry is a department where the exact cause of the disease is determined and a treatment regimen is developed. Specialists know how to work even with the smallest children. Problems in infants can develop due to dental diseases. Most of them are characterized by inflammation, swelling, the appearance of a film and ulcers. The source of infection is pathogenic bacteria. The main diseases include:
- Stomatitis, in which whitish sores with clearly defined edges appear. Children experience discomfort and refuse to eat. The disease progresses when the mucous membrane is damaged, there are not enough vitamins, allergies develop, and the body's defenses decrease.
- Gingivitis, when the gums and other soft tissues of the mouth are affected.
- Caries, with the active development of which white matter is diagnosed in the oral cavity in large quantities.
Stomach and intestinal problems
In pediatric practice, white spots on the palate of a child are quite common. The provoking factor is diseases of the digestive tract:
- Gastritis, which is characterized by inflammatory processes of the gastric mucosa. In addition to whitish deposits, patients experience pain, spasms, and stool disturbances.
- Dysbacteriosis, which is manifested by bloating, weight loss, problems with stool.
- Enterocolitis, in which, in addition to a film in the oral cavity, accumulation of gases and spasms of the gastrointestinal tract are diagnosed.
Symptoms
Gingivitis has a main symptom by which it is easily identified - inflammation affecting the child’s gums. The process begins with a slight redness that quickly gains strength. This signal often goes unnoticed by parents, and children go to the dentist with an active inflammatory process, bright red swollen gums, burning, and pain. These signs indicate that the disease has entered an acute phase.
Children suffer most from the catarrhal form of this disease, which can be chronic or acute. In the first case, the symptoms are not pronounced, pain occurs only when brushing, there is slight swelling, redness, and cyanosis of the gums.
A sign of an acute form of the disease is intoxication of the child’s body. It manifests itself as headache, nausea, lethargy, and fever.
The most complex type of disease, ulcerative gingivitis, manifests itself as follows:
- the inflammatory process progresses;
- their structure changes;
- there is an unpleasant odor from the mouth;
- lymph nodes in the neck enlarge;
- saliva is produced profusely;
- the skin turns pale.
If these signs are left unattended, an ulcerative-necrotic form of the disease may occur, when necrotic areas with a gray-green coating and a putrid odor appear on the gums, saliva becomes viscous, body temperature rises and the general condition significantly worsens.. All this indicates severe intoxication in organism.
During puberty in a teenager or if he has problems with hormones, hypertrophic gingivitis occurs. It occurs due to improper orthodontic treatment of dental anomalies. The inflammatory process is accompanied by increased growth of gingival tissue, which leads to partial closure of dental crowns. This form of the disease is usually localized. One or two gums are affected, sometimes the affected area expands. The most common location is the lower anterior incisors and canines.
Atrophic gingivitis does not have a pronounced inflammatory process and occurs without pain, although over time it can be complicated by periodontal disease.
Prevention
Everyone who gives birth should know how important hygienic cleaning of the child’s oral cavity is. This procedure cannot be ignored. It can prevent many dental diseases. Therefore, do not miss visits to the dentist! Only a doctor can notice problems at an early stage. Treatment started on time will be faster and easier.
Compliance with preventive measures minimizes the risk of pathology. During the period of bearing a child, the expectant mother needs to take care of her health, pay close attention to oral hygiene procedures, and not introduce into the diet those foods that create a favorable atmosphere for the activation of fungi. Prevents problems:
- Refusal of artificial feeding, transition to breastfeeding;
- Before feeding the baby, the breasts should be treated with a solution of baking soda;
- Pacifiers, pacifiers, and bottles should be sterilized;
- After the baby has eaten, you need to give him boiled warm water to drink, which will wash away the remaining milk from the mucous membrane.
Diagnostic methods
The diagnosis is made by a doctor based on the results of studying the medical history and life of the child in combination with a dental examination. The patient’s complaints, the presence of somatic diseases, and whether he is taking medications that may cause the development of gingivitis are clarified.
Then the doctor conducts an external examination, paying attention to maxillofacial anomalies, the condition of the teeth and gums, and makes a diagnosis. The dentist does not require the help of other specialists, since the disease clearly manifests itself externally and does not require instrumental examination.
Causes and mechanisms
The body of a newborn has many structural and functional features and differences, and some persist into older age. Therefore, when you see white formations on the oral mucosa, you should not immediately think about pathology. There are a number of conditions that do not cause concern:
- Bon's knots.
- "Pearls" by Epstein.
- Gingival cysts.
- Neonatal teeth.
Three of the described phenomena (except the last one) make up, perhaps, the majority of cases when parents complain to pediatricians about whitish spots or dots in the mouth of a newborn. However, children may also be susceptible to pathological changes:
- Thrush (candidiasis).
- Aphthous stomatitis.
- Measles.
Based on the variety of possible factors, you will have to exclude them all. And in differential diagnosis you can’t do without a specialist. Most likely, there is no danger in white spots, but parents need to be completely sure that there is no pathology.
The causes of whitish spots or spots on the mucous membrane can be both physiological and pathological changes. Therefore, they cannot be ignored.
Treatment
Treatment for childhood gingivitis is practically no different from how adults are treated. Only medications used for them are softer and more gentle. Treatment begins with professional cleaning of hard deposits and plaque of tooth enamel - mechanical or ultrasonic.
If caries is detected during the examination, then therapeutic treatment is carried out. Gingivitis is then treated with medications with antiseptic and anti-inflammatory properties. Measures are taken to eliminate detected pathologies (bite, frenulum, etc. are corrected).
Ointments and gels are considered effective for children under 4 years of age. For example, Cholisal ointment has analgesic and anti-inflammatory properties, which makes it possible to prescribe it to alleviate the patient’s condition, especially when baby or permanent teeth are cutting. Ointments and gels are applied directly to the inflamed area.
Antibiotics in tablets or in the form of injections are prescribed to children in difficult cases (the presence of infections of bacterial origin in the body). At elevated temperatures, rinses, drinking plenty of fluids, antioxidants, antipyretic drugs for children, and taking vitamins are prescribed.
Prevention measures should include regular visits to the pediatric dentist, training in oral care rules, and parental monitoring of the development of hygiene skills.