Causes of stomatitis
Inflammation of the oral mucosa can be caused by various reasons.
- Mucosal injury6.
- Viral, bacterial or fungal infection6.
- Allergy2.
- Immunity disorders (autoallergy, that is, a reaction to one’s own altered tissues2).
- Diseases of the blood, digestive, cardiovascular, nervous and endocrine systems2.
- Hypovitaminosis - lack of vitamins C, B1, B12, E, D32.
- Common infectious processes: measles, rubella, scarlet fever and diphtheria, infectious mononucleosis, tuberculosis and others1.
Only a specialist can understand the causes of stomatitis. Therefore, if symptoms of the disease appear, you should definitely contact your dentist.
Inflammatory diseases of the oral cavity can occur in a child of any age6. Immaturity of the body is the primary factor predisposing to the occurrence of stomatitis in children under one year of age. The mucous membrane of the oral cavity during this period of a child’s life is very vulnerable, its natural protective properties are reduced. The immunity received from the mother during fetal development and which protected the baby immediately after birth weakens every day. Therefore, the infection easily penetrates the mucous membrane and causes its inflammation. Most often at this age, candidal stomatitis occurs, commonly called thrush1,6.
From the age of one to 3 years, children actively develop immune mechanisms to protect the oral mucosa (local immunity), but its permeability to viruses remains extremely high. Therefore, in a 2-3 year old child, stomatitis is more likely to be viral, in the vast majority of cases - herpetic1,3,4.
From 4 to 12 years of age, stomatitis in children is more often caused by allergic and autoimmune reactions. In particular, chronic aphthous forms of the disease occur during this period1.
Up to contents
Medicines for stomatitis in children: how to treat?
Selecting the right children's medicine for the medical treatment of stomatitis is a rather delicate process. After all, at different ages, children need to be treated differently: those drugs that are suitable for a one-month-old baby may not affect the course of the inflammatory process at all in a two-year-old child.
The same applies to the question of how long it is necessary to treat such a pathology. In infants, a one-year-old baby and a 2-year-old child, recovery times will also differ, even when using the same remedy. In any case, you should not expect quick treatment, since it takes several days to several weeks to relieve inflammatory reactions and heal damaged tissues.
Drug treatment
Drug treatment is aimed at relieving symptoms of stomatitis such as pain and inflammation, as well as accelerating the healing process of damaged tissue.
Painkillers
Since young children have a fairly low pain threshold, pain relief is the primary goal in the treatment of acute stomatitis. For this purpose, both system-wide drugs for oral administration and local agents in the form of gels are used.
Painkillers for oral administration:
- Ibuprofen is a strong drug that has a pronounced analgesic, anti-inflammatory and antipyretic effect. Its dosage is prescribed at the rate of up to 10 mg per kg of the child’s weight three times a day for no more than 5 days in a row. Can be used no earlier than 3 months of age.
- Paracetamol also relieves pain and fights high fever. For children under three years of age, it is preferable to use rectal suppositories or syrup, while older children can use tablets. The dosage is calculated based on the child’s weight (15 mg per kilogram). It is possible to use the product 3-4 times a day.
Local anesthetics:
- Cholisal is a drug with a good analgesic effect, which additionally has anti-inflammatory and antibacterial effects. Apply the gel to damaged mucous membranes 3-4 times a day before or after meals, as well as before bed. It is not advisable to use before 9 months of age.
- Kamistad - a combination of lidocaine with chamomile infusion gives a good analgesic and anti-inflammatory effect. The gel should be used 3-4 times a day, rubbing it into the area of inflammation.
- Kalgel is a combined drug in the form of a gel with antimicrobial and analgesic effects. Well relieves pain from stomatitis, gingivitis and other inflammatory diseases in the oral cavity. Use no more than 6 times a day.
Antiseptic and anti-inflammatory agents
Drugs with antiseptic properties suppress the activity of pathogenic microorganisms and have a good anti-inflammatory effect. They can be used both for rinsing the entire oral cavity and for treating individual areas of damaged oral mucosa. They are successfully used to treat stomatitis at home.
Sprays for the treatment of stomatitis:
- Hexoral is a spray with pronounced activity against pathogenic microflora. Used after meals and remains effective for up to 12 hours. It is used twice a day by briefly spraying the solution in the mouth.
- Inhalipt is a combination drug that combines a soluble form of streptocide in combination with essential oils. It has anti-inflammatory, antiseptic and minor analgesic effects. Oral irrigation is carried out 3-4 times a day until the symptoms of stomatitis disappear.
- Chlorophyllipt is a spray with an antiseptic effect. Suppresses pathogenic microflora, promotes rapid healing of ulcers. Used to irrigate the oral cavity 2-3 times a day until recovery.
Iodine-based preparations:
- Lugol is an iodine-based drug with a pronounced t effect. Used as a spray for irrigating the oral cavity and in a solution for treating damaged areas of the mucous membranes. Treatment of the affected areas is carried out 2-3 times a day using a cotton swab or by spraying a spray.
- Iodinol is another iodine-based medicine. It has low toxicity and is destructive to most microorganisms and fungi. It is not used for stomatitis in children under one year of age, as there is a high risk of swallowing the drug. For children aged 1.5 years and older, it can be used as a mouth rinse (5 ml of solution is diluted in 50 ml of warm water). The procedure is carried out 4-5 times a day, no more than 5 days in a row.
Mouth rinse solutions:
- Stomatidin is a powerful antiseptic with a pronounced anti-inflammatory effect. Used for rinsing the mouth or treating damaged surfaces with an undiluted solution. The procedure is carried out 2-4 times a day, with an interval of at least 4 hours between them. The course of treatment usually lasts 7 days.
- Miramistin is a drug with a broad spectrum of action against pathogenic flora. It eliminates signs of inflammation well. It is used in the form of a solution, which is used to treat areas of stomatitis, or in the form of aerosols, which are applied to the entire oral cavity. The frequency of the procedure is 2-3 times, the duration of the course of treatment is 7 days.
- Chlorhexidine is a solution with an antiseptic effect. Suppresses the growth of pathogenic bacteria and helps the body fight inflammation. Children over 7 months of age can treat the oral cavity with a solution diluted with boiled water (the ratio of water to the drug is 1:1), children over 5 years old can rinse their mouth with a regular solution. Repeat the treatment procedure 2-4 times a day until the symptoms of stomatitis disappear.
- Furacilin is a fairly broad-spectrum antiseptic. Does not cause irritation to mucous membranes. Available in the form of a ready-made solution or tablets. To prepare the solution at home, you need to dissolve 1 tablet of furatsilin in 500 ml of warm boiled water. You need to rinse your mouth with this solution 3-4 times a day until complete recovery. For small children under 2 years of age, the drug can be applied with a gauze swab directly to the inflamed area.
- Hydrogen peroxide as an antiseptic can be used to treat stomatitis in older children. The use of such a product must be careful, since it is toxic and can cause serious burns to the mucous membranes. To prepare a rinse solution, dissolve 1 teaspoon of peroxide in 100 ml of water. Carry out the procedure three times a day after meals. The course of such treatment is 5-7 days.
- Stomatofit is a plant-based drug that has bactericidal, anti-inflammatory and tanning effects. To rinse the mouth, 10 ml of solution is mixed with a quarter glass of water. Treatment is carried out 3-4 times a day until complete recovery.
Anti-inflammatory and antiseptic gels:
- Metrogyl denta is a combined remedy for the treatment of inflammatory diseases of the oral cavity. The gel is applied to areas of the mucous membrane affected by stomatitis three times a day. The course of treatment is approximately 7 days.
Vitamin and regenerating products
Vitamins and wound-healing agents in the treatment of stomatitis are used after acute symptoms have subsided. Their main task is to speed up the regeneration processes in damaged tissues, maximally restore their metabolism and adequate blood supply. Such drugs are most often used topically in the form of oils, gels, and ointments.
The most commonly prescribed drugs are:
- Aekol is an oil solution of vitamins A, E, K and provitamin A. The product is applied directly to the affected area on a gauze bandage once every 48 hours. The treatment course continues until the mucous membrane is completely restored.
- Vinilin - has an anti-inflammatory effect and at the same time stimulates the healing of damage to the mucous membrane. Apply the drug using a cotton swab directly to the affected area after each meal and before bedtime until the clinical manifestations completely disappear. According to the instructions, it can be used after one year of age.
- Solcoseryl is a paste that stimulates the processes of epithelization of damaged tissues, promoting the rapid healing of ulcerative defects in stomatitis. For children, it is necessary to apply the drug 3-4 times a day after thoroughly rinsing the mouth with clean boiled water and drying the inflamed areas with sterile cotton pads.
- Sea buckthorn oil is a natural remedy that has a regenerating effect. After the acute symptoms have subsided, apply with a sterile cotton swab to the inflamed areas twice a day.
Traumatic stomatitis
Inflammation of the mucous membrane in the mouth can be preceded by trauma: mechanical, thermal, chemical, radiation1,6.
Small children who put everything in their mouths can injure the mucous membranes with the sharp edges of toys or household items. Injuries often occur due to inept use of cutlery as a result of falls. In older children, stomatitis may be associated with a thermal burn, blows to the teeth, or the bad habit of chewing a pencil or pen. Sometimes the cause of inflammation is dental diseases and their treatment: sharp edges of damaged teeth and fillings, braces and aligners1.
When stomatitis develops in a child on the gum, on the inner surface of the cheek or in another place, the mucous membrane becomes red and swollen, and a painful erosion or ulcer may appear in the area of damage. Since there are many microorganisms in the mouth, there is always a risk of a bacterial or fungal infection1.
If the mucous membrane is constantly injured, painless whitish or whitish-gray layers may form on it.
In children under 1 year of age, stomatitis can be the result of using the wrong nipples: long, tight, irregularly shaped. The resulting Bednar aphthae are located in the area of the transition of the soft palate to the hard palate and are round erosions or ulcers1.
Treatment of traumatic stomatitis in children includes:
- elimination of traumatic factors;
- rinsing the mouth, irrigating the mucous membranes and treating wounds with drugs with an analgesic and antiseptic effect1.
Up to contents
Angular stomatitis in a child
Causes
In children, seizures are most often a manifestation of allergies, and can also appear while taking antibiotics. The mechanism is as follows: when using antibiotics, the microflora of the oral cavity is disrupted (both harmful and beneficial microbes die), against this background, space is freed up in which Candida fungi settle. It is these fungi that eventually cause the formation of buttocks.
Similar erosions can appear against the background of herpetic lesions, injuries, allergies, dry lips and cracks. It is important to determine the cause of their appearance and only then prescribe treatment.
Symptoms
Angular stomatitis (jams) - erosions with crusts that appear in the corners of the mouth - is also a fairly common form of stomatitis.
Treatment
- Antiseptics (chlorhexidine, miramistin) - use a gauze swab or ear stick to treat the surface of the wound.
- Keratoplasty (solcoseryl, oil solution of vitamins A and E) - applied to a dry surface after antiseptic treatment.
- Fighting the cause of the disease (if it is an allergy, we remove the allergens and prescribe antihistamines, if it is due to antibiotics, we prescribe drugs to restore the microflora and antifungal ointments, etc.).
Viral stomatitis
About 80% of all stomatitis in children is caused by herpes viruses3,5. In approximately 70% of cases, the disease develops in children aged 1 to 3 years3,4.
The disease can occur in mild, moderate and severe forms.
With mild herpetic stomatitis, the general condition is practically not disturbed. Body temperature does not exceed 37-37.50 C. Symptoms of inflammation are limited to swelling of the gums and usually the simultaneous appearance of single painful herpetic blisters and erosions on the mucous membrane (no more than 6). After 1-2 days, the contours of the lesions are blurred, the rashes turn pale, and the erosions heal without scarring3.
With moderate stomatitis, the child’s temperature reaches 38-390 C and lasts until rashes continue to appear. General intoxication manifests itself in the form of weakness, headache, nausea. The child becomes capricious, lethargic, refuses to eat and play3.
As the temperature rises, the oral mucosa becomes red and swollen, and the gums begin to bleed. The number of herpetic elements reaches 20-25, repeated rashes are accompanied by fever3.
Severe stomatitis in children looks like a common acute infectious disease and is accompanied by severe intoxication: fever 39-400 C, chills, headache, aching muscles and joints, heart rhythm disturbances, nosebleeds, nausea and vomiting. The number of herpetic elements can reach 100; they are located not only in the mouth, but also on the skin of the face, on the eyelids and conjunctiva of the eyes, and earlobes. In addition, upper respiratory tract symptoms may be present.3
Treatment includes treating the affected area with painkillers and antiseptic drugs, antiviral therapy, drinking plenty of fluids, a balanced diet and proper nutrition3,5.
Up to contents
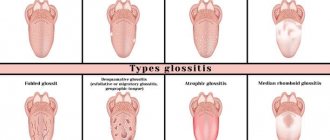
Types of childhood stomatitis and their main manifestations
The classification of childhood stomatitis is based both on the cause of the disease and on some distinctive features in the clinical course of such pathology. We will tell you how to determine this or that type of disease in our article later.
Catarrhal stomatitis
It is the mildest and most common form of the disease. In this case, multiple inflammatory foci appear on the mucous membrane of the gums, cheeks or lips, covered with a whitish coating, but without the formation of aphthae or ulcers. In this case, the child will complain of pain in the mouth when eating, drinking or talking, increased salivation, bad breath, and general weakness.
With catarrhal stomatitis, the mucous membrane is very susceptible to injury and bleeding, even during normal activities: brushing teeth, eating. When inflammatory foci are localized only on the gums, the clinical picture of stomatitis will resemble gingivitis.
Ulcerative stomatitis
The ulcerative form is a consequence of untreated catarrhal stomatitis. In this case, against the background of edematous foci of redness, multiple ulcerations are formed, which gradually increase in size, spread deep into the tissue of the mucous membranes or merge with each other.
The child complains of severe pain in the oral cavity, which intensifies when trying to brush his teeth or eat, and the smell of his breath becomes putrid. General health worsens: body temperature rises, weakness and body aches occur.
Young children are capricious, refuse to eat, and have trouble sleeping.
Gangrenous stomatitis
The gangrenous form of the disease is a continuation of catarrhal and ulcerative forms. A characteristic sign of this pathology is the spread of the inflammatory process deep into the tissues of the jaw with the development of extensive necrosis, which can involve the bones and spread to other anatomical areas.
The condition of a child with gangrenous stomatitis is extremely serious. There may be disturbances of consciousness, severe weakness, and the smell of rotting meat from the mouth. Regional lymph nodes are enlarged and painful on palpation.
Candidiasis (fungal or milk) stomatitis
Candidal stomatitis is characterized by specific symptoms. At the onset of the disease, children have dry mouth. Subsequently, a burning sensation and an unpleasant aftertaste appear. A white coating in the form of small dots is deposited on the mucous membrane. As the process progresses, the points merge into a large lesion that resembles a curdled mass. Such plaque is difficult to remove, exposing the inflamed surface of the mucous membrane.
Fungal stomatitis often occurs without fever, and the general condition is little affected.
Infectious stomatitis
The phenomenon of stomatitis can also be observed in some infectious diseases. With scarlet fever, the typical picture on the mucous membranes of the mouth will be supplemented by specific manifestations of the disease: a pinpoint rash on the skin and a “crimson tongue” - the surface of the tongue is bright red, shiny with hypertrophied papillae.
With diphtheria, damage to the gums will be combined with the detection of dense grayish films on the tonsils or in the throat. In this case, a paroxysmal cough with episodes of suffocation will be noted.
Allergic stomatitis
The allergic form of stomatitis most often affects children over 4 years of age. It is characterized by a clear connection with the action of the allergen, a rapid increase in symptoms and their rapid extinction with adequate treatment. The clinical picture in this case is similar to the ulcerative version of the disease - ulcers or aphthae form on the mucous membranes, covered with a whitish coating and surrounded by a focus of redness. Quite often, this pathology occurs in the form of chronic stomatitis with periodic episodes of exacerbation.
Traumatic stomatitis
In cases of mechanical trauma, a significant focus of infiltration appears on the mucous membrane, which ulcerates as the inflammation progresses. When burned by hot drinks, a bubble often appears, after opening which a fairly deep ulcer is exposed. A distinctive feature of the traumatic form of the disease is a clear connection with trauma or thermal burn of the oral mucosa and the formation of a single lesion.
In case of severe inflammation, local symptoms may be accompanied by general symptoms: fever, malaise, headache.
Herpetic stomatitis
In herpetic stomatitis, the main morphological element is small blisters located against the background of a hyperemic mucous membrane. They quickly open and erosions form, which are covered with fibrous plaque. The lesions can be localized separately or merge into a single affected area.
Erosion is extremely painful, the child refuses to eat, is capricious, sleep is disturbed, and in severe cases there is a significant increase in body temperature. In this case, typical herpetic lesions can be found not only in the oral cavity, but also on the face or other parts of the body.
Bacterial (purulent) stomatitis
Most often, bacterial stomatitis appears due to constant improper oral care or microbial sore throat. The clinical picture is typical for stomatitis: initially foci of inflammation appear, which then transform into deep ulcers covered with abundant purulent plaque.
At the same time, purulent deposits on the tonsils are detected, the child’s general well-being suffers, body temperature often rises significantly, and the cervical, submandibular and clavicular groups of lymph nodes enlarge.
Vesicular stomatitis
Vesicular stomatitis is an infectious disease. Its causative agent is vesiculovirus, a virus transmitted from sick animals to people. The incubation period of this disease is 5-6 days, during which children may complain of fatigue, weakness, and slight chills. Subsequently, small painful blisters with whitish contents appear on the mucous membranes of the oral cavity. Similar elements appear in the area of the feet and hands.
The general symptoms are very similar to a banal acute respiratory infection: the body temperature rises, there may be signs of rhinitis and conjunctivitis. If the intestines are damaged, there may be dyspeptic symptoms: diarrhea or constipation.
Candidal stomatitis
In 80% of healthy children, Candida fungi can be found in the oral cavity. They get there during childbirth, from nipples and pacifiers, from care products, in contact with the mother's skin, with food during eating and usually do not cause any problems. Candidal stomatitis, or thrush, occurs when immunity decreases1.
Predispose to the disease:
- prematurity and postmaturity;
- developmental defects and concomitant diseases;
- treatment with antibiotics and hormones;
- artificial feeding;
- poor care and poor feeding hygiene;
- Using the wrong nipples1.
What does candidal stomatitis look like? In children's mouths, whitish or whitish-gray dotted formations appear on the reddened mucous membrane. They merge into films of a cheesy nature; when the films are rejected, bright red painful erosions are formed. Because of the pain, the baby becomes restless, cries often, sleeps poorly, and refuses to eat1.
In severe cases of candidiasis, a cheesy coating may appear on the palate and on the lateral surfaces of the tongue, on the tonsils and the back wall of the pharynx - candidal tonsillitis and pharyngitis develop1.
If your child has a fungal infection, you should always consult a doctor; he will tell you how and what to treat the mucous membrane with candidal stomatitis, so that the child does not have complications and recovers faster. Treatment, as a rule, involves treating the oral cavity with drugs with antifungal activity (chlorhexidine, hexethidine). In severe cases of the disease, antifungal agents, probiotics and immunomodulators are prescribed1.
Up to contents
General approaches to the treatment of childhood stomatitis
A child who experiences any symptoms of the disease must contact a specialist. It is almost impossible to cure stomatitis on your own, and delaying treatment can cause serious complications, both in newborns and older children.
- It is advisable to isolate a sick child from using common household items in the family. It is worth providing him with separate dishes, cutlery and towels. If there are other children in the family, then it is necessary to minimize contact through shared toys.
- Strict oral hygiene is recommended to prevent secondary infection and worsening of the disease. For example, a child under one year old should treat the oral mucosa with special wipes with xylitol or another antiseptic. Children over one year of age can rinse their mouths with antiseptic solutions before and after meals. To clean your teeth, you should purchase a toothbrush with soft bristles that will not injure the inflamed surface of your gums or tongue.
- When stomatitis occurs in newborns or infants, special attention is paid to the treatment of nipples, feeding bottles, pacifiers and nipples of the mother's mammary glands.
- Eating any food usually brings severe pain to the child. To reduce sensitivity, anesthetic gels and sprays are used.
- Particular attention in the effective treatment of stomatitis is given to nutrition. The food you eat should be at body temperature. All irritating, sour and spicy foods are excluded from the diet. In case of severe pain, you can offer the child to eat homogenized liquid food through a wide tube. Nutrition should be balanced and contain sufficient amounts of nutrients, as well as vitamins and minerals.
For stomatitis, Dr. Komarovsky recommends paying special attention to the microclimate of the room in which the sick baby is located. The room must be well ventilated twice a day. In winter, the air must be humidified using special humidifiers.
Allergic stomatitis
Allergic damage to the mucous membrane most often occurs in the form of contact stomatitis and chronic aphthous form of the disease1.
Allergens can include medications, food products, varnishes and paints that coat toys, toothpastes, mouth rinses, chewing gum, and dental metals included in braces1,2.
With allergic stomatitis in children, erosions and ulcers may appear in the mouth, but more often the matter is limited to redness and swelling of the mucous membrane1.
Treatment is avoiding contact with the allergen, rinsing or irrigating the mouth with antiseptic solutions to prevent infection. If necessary, doctors recommend taking antihistamines1,2.
Chronic recurrent aphthous stomatitis often occurs in schoolchildren and adolescents due to allergies2. In addition, its development can be provoked by diseases of the gastrointestinal tract, upper respiratory tract infections, disorders of the nervous system, and hypovitaminosis1,2.
With aphthous stomatitis in children, itching and burning first appear in the oral cavity. The mucous membrane at the site of the lesion becomes red and swollen, then an aphtha forms on it - a round or oval erosion 0.5-1 cm in diameter rising above the surrounding tissues with a red rim along the periphery and a bottom covered with a grayish-white coating. Aphthae are extremely painful, and if many of them form, they cause significant distress to the child1,2.
How many days does aphthous stomatitis last in children? With a mild course of the disease, the elements of inflammation persist for up to 5-7 days, then they heal without scar formation2 and do not appear for quite a long time. However, in severe cases, aphthae can occur constantly, and then many elements of inflammation can be found on the mucosa at different stages of development1,2.
To treat aphthous stomatitis, doctors use:
- antihistamines;
- immunomodulatory drugs;
- vitamins;
- probiotics2.
As a local therapy, it is recommended to treat the mucous membrane with drugs with analgesic, antiseptic, proteolytic (protein-breaking), anti-inflammatory and regenerating effects2.
Up to contents
Symptoms and signs
How to recognize stomatitis in children? Despite the abundance of causes that cause this disease, all forms of stomatitis have common clinical symptoms:
- The first signs of such a pathology are slight redness on the mucous membranes, which can be localized both on the gums and on the palate, on the tongue or on the lip.
- Gradually, the redness gives way to swelling, round or oval ulcers appear, covered with a whitish or gray coating on top and surrounded by a red cushion. These ulcers are very painful and prevent the child from leading a normal life, eating or sleeping.
- As the inflammatory process becomes more severe, small ulcers merge into one large one.
- Local signs of stomatitis are accompanied by general symptoms: the child’s temperature rises, weakness, and lack of appetite appear.
One of the features of the course of the disease is the appearance of vomiting with stomatitis. It is caused by increased work of the salivary glands and increased excitability of the baby’s nervous system due to severe pain.
Hexoral in the treatment of stomatitis
For local treatment of stomatitis in children, drugs from the HEXORAL® line can be used.
For irrigation of the oral cavity, the doctor may recommend aerosol HEXORAL® based on hexethidine, which has antiseptic properties7. Thanks to the fine spray, the drug is evenly distributed over the entire surface of the mucosa7. A solution of HEXORAL®8, similar in composition, is intended for rinsing the mouth. Both medications can be used to treat children 3 years of age and older.
Mint-flavored lozenges HEXORAL® TABS based on chlorhexidine and benzocaine may be suitable for boys and girls over 4 years of age9.
For patients with stomatitis over 6 years of age - HEXORAL® TABS CLASSIC based on the antiseptic amylmetacresol. The assortment includes tablets with lemon, orange, black currant, lemon and honey flavors10.
HEXORAL® TABS EXTRA may be suitable for adolescents aged 12 years and older. The lidocaine it contains can relieve even severe pain11.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Up to contents
Types of disease
Stomatitis has different forms, depending on which the doctor determines whether it is contagious or not, and also prescribes appropriate treatment.
Allergic stomatitis
This is a common form of the disease that is difficult to treat. From the name it is clear that the cause of its development is an allergy, but it is necessary to find out what exactly it is. These could be medications, food, materials used for prosthetics. The disease is accompanied by the appearance of ulcers, which provoke pain.
Viral stomatitis
The most common type of viral stomatitis is herpetic stomatitis, the causative agent of which is the herpes virus. There are other forms that are provoked by adenovirus, enterovirus, etc. They are often found in children under 5–6 years of age, but are also common among older age groups. A feature of viral stomatitis is its erosive spread, when one ulcer appears next to another. Herpes mucositis may cause complications such as fever, nausea, vomiting and diarrhea.
This form of the disease is transmitted to others by contact and airborne droplets. If it is diagnosed, for example, in someone in kindergarten, then quarantine must be introduced. Infection occurs through dishes and toys, so the disease can quickly spread from child to child.
The virus spreads from nursing mothers to children if hygiene rules are violated. Adults become infected even through handshakes. Sneezing also causes the disease to develop.
Aphthous stomatitis
This form is common among adults. It develops against the background of a weakening of the body’s immune forces, so aphthous stomatitis is a common occurrence in spring and autumn. With this type of disease, characteristic aphthae appear - small ulcers. They can be single or group. Aphthous mucositis is not spread from person to person.
Fungal stomatitis
The disease manifests itself in children and adults, mainly in infants and women. It is provoked by fungi of the genus Candida, which are activated in the oral cavity when the immune system is weakened. The cause of fungal stomatitis can be long-term use of antibiotics. In addition to ulcers, its characteristic feature is a cheesy coating on the tongue, palate and inner surface of the cheeks.
Bacterial stomatitis
This type of disease is diagnosed when the oral cavity is affected by microorganisms, most often streptococci, staphylococci. The manifestation of bacterial stomatitis is provoked by tuberculosis, as well as sexually transmitted diseases, for example, gonorrhea, syphilis. More often, children whose immunity is not strong enough suffer from it. But everyone must be careful. The disease is transmitted from children to adults through dishes, toys, and damage to the mucous membrane.
This form is characterized by swelling in the oral cavity, redness of the mucous membrane and hardening of the palate, as well as an unpleasant odor, ulceration and cracks. Symptoms of intoxication may appear: vomiting, weakness, rapid pulse.
Other forms of stomatitis
In addition to the above types of disease, the following can also be distinguished:
- chemical stomatitis - occurs as a result of burns to the oral cavity with alkaline substances or acid;
- traumatic - ulcers are formed as a result of impact and disruption of tissue integrity;
- radiation – develops as a result of radiation.
Such forms are non-contagious and therefore do not pose a danger to other people.
Literature
- Khomenko L. A. Therapeutic dentistry of children. Textbook for university / ed. 2007 – pp. 643-722.
- Ismailova G. T. Chronic recurrent aphthous stomatitis // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. — P. 124-125.
- Drobotko L.N., Strakhova S.Yu. Acute stomatitis in children // Issues of modern pediatrics. - 2010. - T. 9. - No. 2. - P. 146-149.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Toktosunova S. A., Tsepeleva A. S., Sooronbaev A. A. Prevalence and structure of the incidence of stomatitis in children // Bulletin of Science and Practice. 2022. T. 4. No. 11. — P. 91-96.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Zhumashova N. K., Yuldasheva G. I. Complex therapy of inflammatory diseases of the oral mucosa in children // Bulletin of Science and Practice. 2022. T. 5. No. 5. — P. 96-104.
- Pankrusheva T.A., Maravina I.N., Chekmareva M.S. Research on the development of the composition and technology of tablets for the treatment of stomatitis // Scientific result. Medicine and pharmacy. – T.4, No. 1, 2022. – P. 78-87.
- Instructions for medical use of the drug HEXORAL® aerosol: , .
- Instructions for medical use of the drug HEXORAL® solution: , .
- Instructions for medical use of the drug HEXORAL® TABS: , .
- Instructions for medical use of the drug HEXORAL® TABS CLASSIC: , .
- Instructions for medical use of the drug HEXORAL® TABS EXTRA: , .
Up to contents
Diagnostic methods
Dentists, pediatricians and pediatric infectious disease specialists treat inflammatory diseases of the mouth in children. During the appointment, the doctor will examine your complaints, review your medical history to identify risk factors, and conduct a physical examination.
As a rule, a general and instrumental examination of the mouth is sufficient to make a preliminary diagnosis, since different forms of stomatitis manifest themselves as peculiar ulcers. Additional research may be required to clarify the nature of the disease.