What is stomatitis?
Stomatitis is an inflammation of the oral mucosa. According to statistics, about 20% of the population of our planet faces it. In adults and children, it can take the form of an independent disease or act as a symptom indicating pathologies of the body. In both cases, treatment is carried out comprehensively and under the supervision of a doctor.
What does the disease look like?
Stomatitis is not difficult to recognize. The initial stage of the disease is characterized by the appearance of mild swelling of the oral mucosa. It becomes redder, drier and shiny. A plaque may appear on its surface, and at the site of future lesions the patient feels an unpleasant itching or burning sensation.
As the disease develops, small ulcers and wounds appear on the mucous membrane - painful oval or round lesions. Their location may be the inside of the lips, cheeks, palate, tonsils, or mucous membrane under the tongue. Their appearance can be seen in the photo at the end of our article.
Definition of disease. Causes of the disease
Stomatitis is an inflammation of the oral mucosa.
This disease is characterized by all the signs of an inflammatory process: redness, pain, swelling, dysfunction, increased local and general body temperature. Stomatitis can occur on the mucous membrane of any part of the oral cavity: on the gum, on the tongue, on the mucous membrane of the palate, in the vestibule of the oral cavity, in the retromolar fossa, on the mucous membrane of the cheeks and lips. The disease can manifest itself in a variety of forms: it can be redness of the mucous membrane in a certain area or the appearance of ulcers in the mouth. Stomatitis manifests itself with decreased immunity and chronic diseases, and stomatitis can also develop as a protective reaction of the body to the action of various irritants (for example, mechanical trauma to the mucous membrane from the sharp edges of teeth).
Inflammation of the oral mucosa occurs in most cases in children [12]. But recently, stomatitis has also appeared in the adult population. This is mainly due to the weakening of a person’s immunity, for example, with acute respiratory viral infections, chronic diseases, and HIV infection.
Causes of stomatitis
The mechanism of stomatitis is not yet fully understood. But scientists are inclined to believe that the root cause of its development is the reaction of the human immune system to various irritants. At some point, the immune system ceases to recognize the potential threat of internal and external factors, which causes its atypical reaction, as a result of which “aggressive behavior” of lymphocytes is observed. The attack of lymphocytes against irritant molecules leads to lesions of the oral mucosa.
A variety of factors can provoke an atypical reaction of the immune system. The most likely of them are the following irritants:
- Pathogenic microorganisms that live in the mouth.
- Improper oral hygiene.
- Various damage to the mucous membrane, for example, burns from eating too hot food or mechanical injuries from seeds, nuts, crackers and other hard foods.
- General dehydration due to high fever, blood loss, vomiting, diarrhea, or thirst.
- Poor quality treatment of teeth and gums.
- An allergic reaction to dental structures in the mouth - braces, implants, crowns, bridges, etc.
- Long-term use of medications.
- A diet depleted of beneficial vitamins and elements.
- Smoking.
- Malignant formations of the oral cavity, respiratory organs or undergoing a course of chemotherapy.
- Hormonal imbalances in the body, for example in pregnant women or children during puberty.
- The presence of chronic diseases or allergies.
- Severe stress.
Interesting to know! Frequent stomatitis in adults can be caused by the use of toothpaste containing sodium lauryl sulfate, a substance added to oral care products to form a thick foam. According to recent studies, it dehydrates the oral mucosa and makes it vulnerable to various types of irritants. Patient observation data confirms the fact that avoiding the use of sodium lauryl sulfate paste can reduce the risk of developing stomatitis in adults by 81%.
Symptoms of the disease
Stomatitis can occur at any age. In the early stages, its course is accompanied by swelling, redness and dryness of the oral mucosa. The main sign of the disease is the presence of one or multiple ulcers and their appearance.
- Oval or round ulcer shape.
- Small sizes.
- Smooth edges.
- The presence of a thin grayish or white film in the central part of the ulcer.
- The ulcer is surrounded by a slightly reddish halo.
- The mucosal tissue around the lesion has a normal, healthy appearance.
The slight itching or burning sensation that the patient experienced at the beginning of the disease is replaced by pain. The ulcers hurt when eating, talking and smiling broadly. Any touch to them causes pain, which complicates hygiene measures and leads to bad breath.
On average, the disease lasts from 4 to 14 days. Its clinical picture depends on the individual characteristics of the organism, the form and type of the disease. During this period, in addition to the main signs of pathology, other symptoms of the disease may be observed.
- Increase in temperature - during the first days, until characteristic ulcers appear (in severe forms of stomatitis, the elevated temperature persists throughout the entire illness).
- General malaise and fatigue.
- Chills.
- Headache.
- Lack of appetite (especially in children).
- Enlarged lymph nodes (in rare cases).
Important to remember! Severe inflammation, toothache or high temperature for a long time indicate a severe form of stomatitis or the development of its complications. In this case, immediate medical attention is required, and if necessary, hospitalization of the patient is possible.
Symptoms of stomatitis
The manifestation of stomatitis can be different.
This depends on the form and stage of development of the disease. The first symptom is redness of the oral mucosa in a certain area. The spot does not rise above the level of the mucous membrane, has a round or oval shape and may be pinkish or whitish in color. Next, the area around the affected area becomes swollen, hyperemic, and pain appears. Aphtha appears at the site of the spot. Aphtha (from the Greek aphtha - ulcer) is a superficial defect of the mucous membrane, having a round shape and a grayish fibrinous coating. If you remove necrotic plaque from the surface of the aphthae, the ulcer will begin to bleed [5]. Most often, aphthae are located along the transitional fold, on the lateral surface of the tongue, on the mucous membrane of the cheeks and lips.
In severe forms, the amount of fibrinous plaque on the surface of the ulcer increases, and an infiltrate appears at the base of the aphthae (an accumulation of cellular elements of blood and lymph in the mucous layer). With such a clinical picture in the oral cavity, the patient experiences pain, burning, itching, bad breath, increased salivation, and eating becomes difficult. Body temperature rises to 38 ℃, weakness appears.
A feature of the disease is frequent relapses. Repeated rashes may appear after a few days or every few months. It depends on the ability of the immune system to fight infection.
In the most severe cases, stomatitis manifests itself in the form of ulcers on the mucous membrane. An ulcer is a deep defect of the mucous membrane, in which the entire thickness of the mucous membrane is affected. The ulcer is surrounded by an inflammatory infiltrate, the edges of the ulcer are uneven, scalloped (jagged) [5]. When ulcers appear in the oral cavity, the general condition also worsens. The submandibular lymph nodes on the affected side may become inflamed. On palpation they will be enlarged and painful.
With candidal stomatitis, a white coating appears on the tongue and gums; when trying to remove the plaque, the affected areas begin to bleed. There is also an unpleasant taste in the mouth and a burning sensation. If candidal stomatitis develops against the background of diabetes mellitus or immunodeficiency conditions, it always has a chronic course.
With viral lesions of the oral mucosa, pain occurs, which intensifies during eating and when talking. The mucous membrane turns red and swells, then small blisters appear on it. The bubbles quickly open and aphthae form in their place. In moderate and severe forms, body temperature rises to 37-40 ° C, general malaise, weakness, and headache are noted.
Can stomatitis go away on its own?
As a rule, mild forms of the disease caused by trauma to the mucous membrane, poor oral hygiene or an allergic reaction of the body can go away on their own. Severe stomatitis caused by infection requires qualified treatment. In both cases, it is better not to wait and not to self-medicate. Because the disease not only causes pain and discomfort, but can also lead to generalization of infection and serious complications.
Consequences and complications of the disease
Possible complications arise when the patient ignores treatment for stomatitis. As a result, mild and severe forms of the disease become chronic. The neglected process turns into an ulcerative-necrotic and then gangrenous form of the disease, as a result of which not only the mucous membrane is damaged, but also the soft tissues of the mouth and jaw bones.
Other serious consequences of untreated stomatitis include the following complications.
- Bleeding gums.
- Scarring of the oral mucosa, disruption of its elasticity and mobility.
- Attachment of a secondary infection.
- Tooth loss.
- Voice changes – hoarseness, hoarseness.
Important to remember! A small ulcer on the oral mucosa is a potential threat to the entire body. Infection from it can spread to other organs and systems, which will disrupt the functions of the heart, liver, kidneys, gastrointestinal tract and respiratory organs.
Folk remedies
For treatment, you can use traditional medicine. The following juices, decoctions, oils and infusions have proven themselves well.
You can gently lubricate the affected areas of the mucous membrane with juices and oils. Solutions and decoctions of herbs are used for regular rinsing of the mouth.
Important! Before using traditional medicine, you should consult a doctor. Only a specialist can determine the advisability of their use without harm to health. The use of folk remedies does not cancel the main therapy, but only complements its effect.
How to treat the disease
Therapy involves the use of local and sometimes systemic drugs. The treatment regimen for the disease depends on what type of stomatitis is diagnosed. For this reason, you should not self-medicate, as it may turn out to be useless and the pathology will continue to develop into dangerous conditions.
The exception is mild catarrhal inflammation associated with poor hygiene. It is enough to exclude the cause and rinse your mouth with antiseptics for several days.
Treatment at home for other types should be discussed with your doctor. The use of folk remedies is not contraindicated, but they can only be used as a supplement to the main therapy. Only a dentist can evaluate the appropriateness and harmlessness of a particular prescription.
Effective drugs for adults
To relieve inflammatory processes, combat pathogenic microflora, and relieve pain, rinses, gels, sprays, lozenges, and ointments are prescribed. For severe pain, pain medications can be taken orally. Since treatment must be carried out regularly, it is important to choose a medicine for stomatitis that will be convenient to carry in your purse and use at work.
Popular medicines:
- Chlorophyllipt, Inhalipt, which have an antiseptic effect. Available in the form of sprays. Apply up to 5 times a day for one week. Sprays are convenient to use if there is stomatitis in the palate or throat.
- Solcoseryl accelerates tissue regeneration, restores mucous membranes, and protects against the development of ulcers. The gel is applied several times a day. The course is from 7 to 14 days.
- Cholisal has a detrimental effect on bacteria, relieves inflammation, and improves tissue healing. The gel is used three times a day for at least a week. An analogue of the drug is Kamistad. Excellent help with aphthous, bacterial form of the disease.
- Viferon, Acyclovir are prescribed to patients with a viral infection. Ointment for stomatitis in the mouth is applied to areas of inflammation several times a day. The course of therapy is up to 2 weeks.
- Lidocaine Asept, Lidochlor are used for any form of pathology, since the main purpose is to relieve acute pain. Available in spray form. Can be used up to four times a day, no more than 1 week.
- Lugol kills bacteria, treats ulcers, and relieves inflammatory processes. The oral cavity is treated with a spray 2 - 3 times a day.
- Miconazole and Nystatin are prescribed for fungal infections. In severe cases of the disease, the ointment is used in combination with systemic medications. Apply to affected areas 2 to 4 times a day.
Any medication for stomatitis must be prescribed by a doctor. The symptoms of the varieties of the disease are similar and it is impossible to independently understand the cause of the inflammatory reactions.
What can you rinse your mouth with?
To treat pathology, you can use pharmaceutical drugs aimed at destroying bacteria, reducing inflammation and healing tissue.
Medicinal solutions that can be bought at the pharmacy:
- Aqualor with sea salt;
- Stomatofit, Dr. Theiss Sage based on sage;
- Romazulan with chamomile extract;
- Chlorhexidine (pre-diluted with water).
Decoctions and infusions for rinsing are easy to prepare at home from chamomile, calendula, aloe juice, sea buckthorn, linden flowers and other medicinal plants. A solution of salt and soda helps a lot.
How many days does treatment last?
Correct, competent treatment of stomatitis significantly speeds up the healing process. Depending on the type of disease, it lasts for 3 to 7 days. If after 1 week of treatment the signs of the disease have not disappeared or worsening is observed, then the patient most likely has complications. The following factors may be the probable reasons for its development.
- The patient self-medicated or did not follow the doctor's instructions.
- Decreased immunity.
- The presence of chronic diseases of the body.
- Regular injury or infection of the oral mucosa.
- Undiagnosed allergy.
- Having bad habits - smoking, chewing, etc.
- Depression or frequent stress.
- Improper oral hygiene.
- Uncontrolled use of medications.
- The use of oral hygiene products containing sodium lauryl sulfate.
Returning to the question - can stomatitis go away on its own - it should be noted that a seemingly harmless disease can turn into serious problems for the patient. Therefore, you should remember three “don’ts” - don’t
engage in self-medication,
do not
put off visiting a specialist and
do not
ignore the recommendations of your doctor.
How to understand that stomatitis has passed?
Very simple! A complete cure is indicated by the absence of lesions in the oral mucosa. There are no small ulcers, wounds or plaque on the cheek, palate, lip, tongue or tonsil area. The mucous membrane looks healthy, is well moisturized, does not cause pain and does not create discomfort during eating, talking, smiling and performing hygiene procedures.
Treatment of allergic stomatitis
This type of stomatitis is caused by the body's immunological response to contact with an allergen. The role of the latter can be played by anything: food products, new oral hygiene products, dentures, animal hair and much more. At risk are patients who are predisposed to allergies or suffer from various autoimmune diseases. A distinctive feature of allergic stomatitis is the acute onset of the disease, accompanied by an increase in temperature, severe pain and putrid odor from the mouth, which does not disappear even after thorough brushing of the teeth.
Treatment methods
- Identifying the allergen and eliminating it (or minimizing contact).
- Antihistamine therapy.
- Relief of inflammation with corticosteroids.
- Taking analgesics to relieve pain.
- Local antiseptic drugs
- Diet.
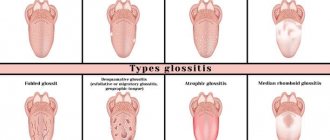
Types of stomatitis in adults
The clinical picture of the disease indicates that stomatitis can be mild or severe, have an acute or chronic course. To facilitate the diagnosis and treatment process, experts have developed the following classification of the disease.
- Allergy is usually a chronic disease that occurs as a result of an allergic reaction of the body to an irritant. In addition to the characteristic ulcers, it may be accompanied by the appearance of white spots, blisters and small hemorrhages on the mucous membrane.
- Herpetic or herpes - the disease occurs due to the entry of the causative agent of the herpes virus into the human body. Stomatitis of this type is characterized by an acute course. Bubbles appear on the surface of the mucous membrane, which open to form erosions and crusts.
- Traumatic (bacterial) – a consequence of mechanical trauma to the oral mucosa and infection entering the wound. As a rule, the disease is mild, with symptoms characteristic of stomatitis.
- Catarrhal and catarrhal-hemorrhagic stomatitis is a mild form of stomatitis, the causes of which are poor oral hygiene, the development of candidiasis, decreased immunity or gastrointestinal pathologies. The disease is accompanied by a typical clinical picture for the disease.
- Candidal (fungal) stomatitis is an acute form of the disease, the so-called thrush, caused by the activity of bacteria of the genus Candida. It is most common in young children, the elderly, and patients who overuse antibiotics. Accompanied by the appearance of a white coating on the mucous membrane, a burning sensation and an unpleasant taste in the mouth.
- Ulcerative is a severe form of the disease that occurs independently or as a result of a complication of the catarrhal course of stomatitis. It occurs acutely, with increased body temperature and enlarged lymph nodes. The resulting ulcers are very painful and can unite and form extensive lesions of the mucous membrane.
- Aphthous stomatitis is a severe form of the disease, occurring acutely or chronically. Accompanied by the appearance of single or multiple gray-white ulcers. The ulcers are surrounded by a red halo and are very painful.
It is important to know! By analyzing the condition of the oral mucosa, the nature of the ulcers and the patient’s complaints, specialists accurately determine the type of stomatitis and make an accurate diagnosis. Thanks to this, treatment of the disease occurs quickly and without complications.
Treatment of ulcerative stomatitis
Ulcerative stomatitis very often occurs due to poor oral hygiene and bad habits (especially smoking). Often this type of stomatitis at its onset is confused with periodontitis and gingivitis, since it is characterized by inflammation of the gums, a grayish coating around the teeth and death of soft tissues. Often accompanied by fever and fever. One of the few forms of stomatitis, which often requires treatment by a doctor, and in the most advanced cases, surgical intervention.
Treatment methods
- Antibiotic therapy.
- Antibacterial treatment of affected areas.
- Surgical intervention (in severe cases, removal of areas of dead tissue and gum grafting).
Which doctor should I contact for stomatitis?
If you notice the first signs of damage to the oral mucosa, you should immediately consult a dentist. After differential diagnosis of the disease and an accurate diagnosis, it is possible to observe it with a general practitioner or other specialized specialist, for example, an allergist.
Do not ignore preventive visits to the dentist.
It is enough to visit a specialist 1 – 2 times a year, which will allow you to promptly identify any dental problem at an early stage of development. This means that its elimination will be quick, easy and without complications.
By clicking the “request a call” button you agree to the personal data processing policy.
Treatment of herpetic stomatitis
Treatment of stomatitis after detection can be carried out many times (once a year or more often), since once settled in our body, the herpes virus remains there for life. Herpes stomatitis is characterized by the accumulation of reddish transparent blisters on the lips and inside the mouth, so it is quite easy to detect. Especially often, herpetic stomatitis manifests itself against the background of decreased immunity, vitamin deficiency, hypothermia and stress. Remember that herpetic stomatitis in adults is contagious, so you should avoid tactile contact.
Types of drugs
- Antiviral agents.
- Immunostimulants (as a preventative measure).
- Ointments (including to eliminate visual manifestations of the disease).
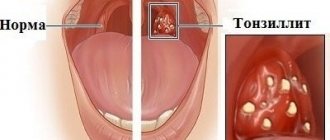
How to distinguish stomatitis from other diseases?
The main sign of stomatitis is the presence of characteristic ulcers, the tissue around which looks healthy. The disease is rarely accompanied by systemic symptoms and, as a rule, recurs from time to time. For a competent specialist, it is not difficult to distinguish stomatitis from other ailments.
For a sore throat
When you have a sore throat, your body temperature always rises. In this case, it is not the ulcers themselves that hurt, but the throat area. Upon visual examination, the tonsils appear swollen, inflamed and red.
For herpes
The problem is that herpetic stomatitis is one of the manifestations of herpes. A viral disease is accompanied by the formation of characteristic blisters that burst and dry out. In the presence of other types of stomatitis, the nature of the ulcers is completely different.
For cancer
Ulcers due to cancer of the oral mucosa do not go away on their own even after treatment. Over time, they increase in size and may bleed and become painful.
From thrush
Candidal stomatitis is thrush caused by the activity of bacteria of the genus Candida. In all other cases, the nature of the disease will be different and can be easily distinguished from thrush by the presence of characteristic ulcers.
For syphilis
When infected with syphilis, a red spot appears on the surface of the mucous membrane. Gradually it thickens, takes the form of a dense nodule and ulcerates - a typical hard chancre is formed, which is completely different from ulcers with stomatitis.
Treatment approach
Treatment of this pathology is not difficult. It is based on several points .
The first is to eliminate the irritant, that is, quit smoking . If this is not possible, then try to reduce the number of cigarettes and focus your energy on improving oral hygiene .
The second is to temporarily stop eating hot and spicy foods, hot foods and drinks .
Eliminate sour foods, sugar, and ice cream from the menu. Gradually, the inflamed mucous membrane will begin to return to normal.
However, you need to approach the treatment of the disease thoroughly; for this there are two ways to eliminate the disease - drug treatment and traditional methods.
Drug treatment
A popular remedy for the treatment of stomatitis is the antiseptic “Chlorhexidine” - it gently cleanses the mucous membranes and has a disinfectant effect.
The drug "Cholisal" effectively relieves pain thanks to tsetalkonium and choline in the composition. The product is applied in the form of compresses to the inflamed areas at least twice a day.
Stay up to date! Gel "Alveolite" - reduces the intensity of inflammation, anesthetizes the surface of the mucous membrane.
Oxolinic ointment - eliminates the symptoms of infection. The product is applied not only to ulcers, but also to the entire oral cavity.
Traditional methods
The best folk remedies for treating the disease in the early stages are herbs and plants (calendula, chamomile, yarrow, anise, sage, oak bark, flax).
In addition to herbal decoctions, folk remedies involve the use of raw potatoes, honey, garlic, cabbage and carrots .
These ingredients are used to make ointments to reduce pain.
Folk remedies are also used for oral administration. For example, rosehip decoction - it destroys pathogenic bacteria, improves immunity and fights inflammation.
On average, treatment of stomatitis occurs within 5-8 days , depending on the degree of the disease. The ulcers heal well and there are no marks left at the wound site.
Recommendations during treatment
Treatment of stomatitis should be carried out comprehensively - local therapy, taking medications appropriate to the type of disease, and strengthening the immune system. During the treatment period, you must adhere to the following recommendations.
- Compliance with the diet - you need to exclude from the diet spicy, salty, sour, too sweet, smoked, hot, cold and any dishes that are traumatic to the mucous membranes.
- Maintaining oral hygiene . To maintain it, it is necessary to use antiseptic agents that you regularly rinse your mouth with.
- Taking vitamin-mineral complexes that strengthen the body's protective functions.
If the doctor has diagnosed the presence of candidal stomatitis, then you should not drink milk or consume fermented milk products, which activate the activity of pathogenic fungi.
Any medications should be used only as prescribed by a doctor. Especially antibiotics.
It is important to know! It is not recommended to cauterize emerging ulcers with pure alcohol solutions. The only thing that is allowed is treating the lesions with a weak solution of iodine or potassium permanganate.
Prevention of stomatitis
Consists of the following items:
- strengthening the immune system, giving up bad habits, hardening, playing sports, eating with a sufficient amount of macros and vitamins (especially vitamin C)
- regular visits to the dentist
- adequate brushing of teeth at home, as well as removal of dental plaque in the dentist’s office once every 6 months
- identifying the allergen and avoiding contact with it
- undergoing medical examination for timely detection of diseases
- treatment of systemic diseases
- taking antibiotics only as prescribed by a doctor, together with a course of probiotics, to avoid dysbiosis
- vaccination (against measles, chickenpox)
Tantum® Propolis
It is worth paying attention to Tantum Propolis, since propolis has an immunostimulating effect, promotes healing, and vitamin C, which is part of it, is responsible for regeneration, participating in the synthesis of collagen.
Propolis also has antiviral and antifungal effects. Therefore, vitamin therapy Tantum Propolis is an effective means of preventing stomatitis.12 Find out more
Prevention
To avoid the occurrence of stomatitis and its relapses, you should adhere to the following recommendations.
- Maintain oral hygiene.
- Avoid using products containing sodium lauryl sulfate.
- Protect the oral mucosa from injury.
- To treat teeth and gums, contact experienced, qualified specialists.
- Balance your diet with healthy foods.
- Strengthen immunity.
- Be attentive to your physical health and psycho-emotional state - if necessary, seek help from specialized specialists.
And do not forget that herpes stomatitis can be transmitted from person to person - follow the rules of hygiene.
Photo of stomatitis
Author: Elena Grunina Dentist-therapist, endodontist. Work experience more than 9 years. The information is for reference only. Before treatment, consultation with a doctor is necessary.