Infectious and inflammatory diseases of the oral cavity are often diagnosed in children. Doctors explain this by insufficient hygiene in childhood and the incomplete formation of the immune system.
In this case, it is necessary to distinguish between dangerous infections and benign inflammatory processes. Thus, temperature during stomatitis in children may indicate the infectious nature of the disease.
Causes of stomatitis
The imperfection of local and general defenses of the child’s body makes the mucous membranes of the oral cavity vulnerable to adverse factors. And the healthy curiosity characteristic of every child has made stomatitis one of the most common diseases among children. Sometimes, for the development of an illness, it is enough to taste any less than sterile object. The main causes of the disease include the following:
- insufficiently good oral hygiene;
- minor injuries - cheek biting, scratch, etc.;
- burns, including chemical burns;
- exposure to pathogens from unwashed hands or dirty toys.
Dentists focus on stomatitis associated with biting the inside of the cheek.
This is often associated with recent dental treatment under local anesthesia. For some time after the procedure, there is reduced sensitivity in the area of the lip or cheek, so you need to eat food after treatment very carefully and only after you have waited for the recommended period of time - usually from 1 to 2 hours. The likelihood of developing stomatitis for these reasons increases after infectious diseases, previous interventions, hypothermia and other factors that contribute to a decrease in protective forces.
Causes
Stomatitis can have different etiologies
Doctors are not always able to identify the cause of stomatitis. The inflammatory form of the disease can occur suddenly against the background of complete clinical well-being. It is assumed that the mucous membrane can be damaged under the influence of a variety of negative factors.
Main reasons:
- Minor trauma to the oral mucosa as a result of careless brushing of teeth, an accidental bite, or damage during eating.
- Negative effects of substances contained in toothpastes and mouthwashes. For example, sodium lauryl sulfate can cause an inflammatory process in the mucous membrane.
- Sensitivity to certain foods. As a rule, these are chocolate, coffee, fruits, eggs, nuts, cheese, spicy and sour foods.
- Vitamin B12 deficiency in the diet.
- Insufficient intake of zinc, folic acid and iron from food.
- Allergic reaction.
- Hormonal changes during puberty and the menstrual cycle.
- Chronic stress.
- Entry of pathogenic bacteria, viruses or fungi into the oral cavity.
- Pathologies of immunity.
It is also necessary to take into account the influence of risk factors, the presence of which increases the likelihood of developing the disease. The main risk factors for stomatitis include:
- Inflammatory diseases of the digestive organs. This could be celiac disease, Crohn's disease or ulcerative colitis.
- Gastroesophageal reflux. The contents of the stomach can even enter the oral cavity.
- Behçet's disease is a rare disorder that causes inflammation throughout the body, including the mouth.
- HIV and AIDS.
- Childhood.
- Family history of inflammatory and infectious diseases of the mouth.
Often, stomatitis appears against the background of other inflammatory pathologies of the digestive organs.
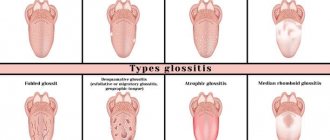
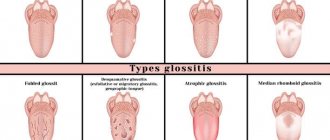
Types of stomatitis
The treatment regimen for stomatitis in children is based on the type of disease. There are several types of stomatitis:
- bacterial;
- viral, including herpes;
- fungal;
- aphthous;
- angular;
- allergic;
- traumatic.
All types of stomatitis occur in children, but the most common among children under 3 years of age are aphthous, candidal, herpetic and allergic. An increase in the incidence of traumatic stomatitis is usually associated with a period of active growth of primary teeth.
It is important to understand that in some cases, stomatitis is combined with other diseases with similar symptoms and is the first sign of more serious diseases. For example, with cheilitis - inflammation of the mucous membrane and red border of the lips, food allergies, etc.
What is stomatitis
Stomatitis is an inflammatory process on the oral mucosa
In the medical literature, stomatitis is an inflammatory disease of the oral mucosa, characterized by the appearance of small white ulcers on the inner surface of the lips, gums, tongue and throat.
Depending on the cause, it may be aphthous or infectious stomatitis. The pathology is manifested by pain, general malaise and other symptoms.
The mucous membrane of epithelial origin covers almost the entire surface of the oral cavity. Special cells of the mucous membrane not only protect internal tissues, but also secrete various substances. Also in the oral cavity there are salivary glands necessary to ensure primary digestive functions.
When an ulcer occurs, the mucous membrane is damaged and the function of the surface epithelium is disrupted. As a rule, the disease has a benign course, but in rare cases dangerous complications may develop.
Small ulcers with stomatitis may appear during the day. Even without treatment, the inflammatory process is self-limiting within 7-10 days. However, large ulcers often require long-term treatment.
Stomatitis can also become chronic. In this case, foci of inflammation will appear periodically in different parts of the oral mucosa. Untimely or incorrect treatment contributes to relapses.
Symptoms
Common symptoms of stomatitis are pain, burning, swelling of the mucous membrane and redness, and bad breath. Salivation also changes - it can be excessive or insufficient, with dry mouth. In some cases, there may be an increase in temperature and enlargement of the submandibular lymph nodes.
The types of stomatitis in children and treatment methods differ, as do the specific manifestations. For example, with aphthous stomatitis, only one large ulceration may appear, but with viral stomatitis, inflammation almost always takes the form of numerous elements or a rash merging into one focus.
Candidal stomatitis is characterized by the formation of a white or yellowish cheesy coating. It is easier to recognize traumatic stomatitis because it is preceded by damage or the source of injury is nearby - a chipped tooth or a rough filling.
Symptoms and signs
With fungal stomatitis, a white coating appears
The symptomatic picture depends on the type of stomatitis. Infectious and inflammatory forms of the disease may have different symptoms.
Main manifestations:
- Painful sensations. The pain may worsen while eating because the skin under the ulcer is very sensitive.
- The appearance of red spots in the mouth.
- Swelling and redness around the ulcer.
- Burning sensation in the mouth.
- Weakness.
- High body temperature.
The most aggressive symptoms are characteristic of candidiasis and herpetic stomatitis.
Diagnostic features
A dentist can detect stomatitis during the first visual examination. But in controversial cases, laboratory tests may be required. Thus, bacterial inflammation may require identification of the causative agent of the disease and its sensitivity to antibiotics. A scraping and/or virological study will help determine the cause of the disease and prescribe appropriate treatment.
If a combination of several ailments with a similar picture is suspected, as well as if the child’s general well-being deteriorates, laboratory tests of blood and urine and consultations with other specialists may be prescribed.
Sometimes stomatitis can be the first manifestation of systemic diseases, general somatic pathology, for example, diabetes mellitus or malignant neoplasms. Therefore, a timely visit to the doctor is extremely important.
Candidal stomatitis
In 80% of healthy children, Candida fungi can be found in the oral cavity. They get there during childbirth, from nipples and pacifiers, from care products, in contact with the mother's skin, with food during eating and usually do not cause any problems. Candidal stomatitis, or thrush, occurs when immunity decreases1.
Predispose to the disease:
- prematurity and postmaturity;
- developmental defects and concomitant diseases;
- treatment with antibiotics and hormones;
- artificial feeding;
- poor care and poor feeding hygiene;
- Using the wrong nipples1.
What does candidal stomatitis look like? In children's mouths, whitish or whitish-gray dotted formations appear on the reddened mucous membrane. They merge into films of a cheesy nature; when the films are rejected, bright red painful erosions are formed. Because of the pain, the baby becomes restless, cries often, sleeps poorly, and refuses to eat1.
In severe cases of candidiasis, a cheesy coating may appear on the palate and on the lateral surfaces of the tongue, on the tonsils and the back wall of the pharynx - candidal tonsillitis and pharyngitis develop1.
If your child has a fungal infection, you should always consult a doctor; he will tell you how and what to treat the mucous membrane with candidal stomatitis, so that the child does not have complications and recovers faster. Treatment, as a rule, involves treating the oral cavity with drugs with antifungal activity (chlorhexidine, hexethidine). In severe cases of the disease, antifungal agents, probiotics and immunomodulators are prescribed1.
Up to contents
Features of treatment
As is often the case with diseases that are at the intersection of several areas of medicine, inflammatory lesions of the oral mucosa are one of the least studied areas of dentistry. Therefore, several specialists can be involved in the treatment of stomatitis in children in the mouth: pediatrician, dentist, dermatologist, immunologist-allergist, otolaryngologist, etc. This is especially convenient when you go to a multidisciplinary clinic.
Self-medication of stomatitis is unacceptable, and although it is now easy to find ready-made treatment regimens and folk recipes, it is important not to experiment with the baby’s health.
Conservative treatment is mainly used, which involves treating the underlying cause of the disease. Your doctor may prescribe the following medications:
- antibacterial drugs (systemic and local in the form of ointments): for bacterial inflammation;
- antiviral agents for herpes and other types of viral stomatitis;
- antifungal drugs for fungal diseases;
- antihistamines - both for allergic origin of stomatitis, and as part of complex therapy to reduce swelling and itching;
- symptomatic drugs - anti-inflammatory, analgesic, antipyretic.
Treatment of candidal stomatitis in infants should be carried out with caution. At the same time, it is important to pay attention to your health; sometimes the cause of such a disease can be insufficient breast hygiene during lactation.
Often, only local remedies are sufficient, but make sure that the entire oral cavity is treated with the rinse - inflammatory agents can be found on the entire surface of the mucous membranes. Healing applications can be used to a limited extent, only on areas of inflammation.
Treatment of stomatitis of any kind in children involves strict adherence to a diet. The diet should be gentle, it is important to avoid salty, spicy, sour foods and drinks, serve the child warm meals, and limit the consumption of sweets.
If traumatic stomatitis occurs, the doctor will prescribe medications to speed up healing. However, it is very important to prevent re-injury. If it was caused by sharp edges of a tooth or filling, this cause should be eliminated. The doctor will suggest grinding off the filling or replacing it, and will also choose the appropriate option for restoring the shape of the crown in case of chips and cracks.
Viral stomatitis
About 80% of all stomatitis in children is caused by herpes viruses3,5. In approximately 70% of cases, the disease develops in children aged 1 to 3 years3,4.
The disease can occur in mild, moderate and severe forms.
With mild herpetic stomatitis, the general condition is practically not disturbed. Body temperature does not exceed 37-37.50 C. Symptoms of inflammation are limited to swelling of the gums and usually the simultaneous appearance of single painful herpetic blisters and erosions on the mucous membrane (no more than 6). After 1-2 days, the contours of the lesions are blurred, the rashes turn pale, and the erosions heal without scarring3.
With moderate stomatitis, the child’s temperature reaches 38-390 C and lasts until rashes continue to appear. General intoxication manifests itself in the form of weakness, headache, nausea. The child becomes capricious, lethargic, refuses to eat and play3.
As the temperature rises, the oral mucosa becomes red and swollen, and the gums begin to bleed. The number of herpetic elements reaches 20-25, repeated rashes are accompanied by fever3.
Severe stomatitis in children looks like a common acute infectious disease and is accompanied by severe intoxication: fever 39-400 C, chills, headache, aching muscles and joints, heart rhythm disturbances, nosebleeds, nausea and vomiting. The number of herpetic elements can reach 100; they are located not only in the mouth, but also on the skin of the face, on the eyelids and conjunctiva of the eyes, and earlobes. In addition, upper respiratory tract symptoms may be present.3
Treatment includes treating the affected area with painkillers and antiseptic drugs, antiviral therapy, drinking plenty of fluids, a balanced diet and proper nutrition3,5.
Up to contents
Prevention of stomatitis
You can reduce the risk of developing stomatitis using the following recommendations:
- regular washing of toys, bottles, pacifiers, breast hygiene if the baby is breastfed;
- general strengthening activities: walks, wet cleaning, a balanced diet, moderate hardening, adherence to a daily routine;
- fighting bad habits of biting nails, pencils, etc.;
- regular dental examinations and timely interventions in case of dental injuries.
The dentists of the Family Doctor clinic treat and prevent stomatitis in children.
Advanced equipment allows us to quickly and accurately assess the condition of the oral cavity and perform the necessary studies in a short time. We practice modern approaches to the treatment of inflammatory diseases of the oral cavity and adhere to an individual approach to each small patient. Consultations with a pediatric dentist are available by appointment. To make an appointment, call the single contact center or fill out a special online appointment form with a pediatric dentist on the website, or you can also visit the clinic’s reception in person.
Treatment and prevention
Stomatitis affects the general condition of the baby
Therapy should be aimed at the root cause of oral ulcers. Typically, all forms of inflammatory stomatitis resolve on their own within 7-10 days.
Treatment may be required if infection develops or inflammation progresses unfavorably. Therapy is also sometimes required to prevent relapses of the pathology.
The most effective treatment methods:
- Mouth rinse. Oral antiseptics and products containing dexamethasone or lidocaine can be used as a rinse. This method of treatment removes pathogenic microorganisms from the oral cavity, as well as reduces pain and inflammation.
- Pastes, creams and gels for treating the oral cavity. The active ingredients in such products help reduce pain and speed up recovery. Your doctor may recommend medications that contain benzocaine, fluocinonide, or hydrogen peroxide. Before prescribing such drugs, it is necessary to determine the etiology of the disease.
- Oral steroid drugs for severe stomatitis. Usually prescribed if the disease does not respond to other drug treatments.
- Chemical cauterization of ulcers using silver nitrate and other reagents. Helps speed up healing and relieve symptoms.
- Antiallergic drugs with a positive sensitization test.
- Antibiotics, antiviral and antifungal agents.
- Nutritional supplements containing folic acid, B vitamins and zinc.
The listed remedies can only be prescribed by a doctor after a thorough diagnosis. Independent drug treatment is fraught with the development of dangerous complications.
Prevention methods include:
- Avoidance of foods that irritate the oral mucosa.
- Child nutrition appropriate for his age group.
- Maintain careful oral hygiene.
- Rinsing your mouth with special solutions.
- Timely treatment of inflammatory and infectious diseases.
Such methods are also important for preventing recurrences of stomatitis.
Treatment
Despite the fact that when stomatitis develops in adults, its symptoms and subsequent treatment are interrelated , that is, based on the manifestation of the disease one can roughly get an idea of the cause, in no case should you self-medicate!
Stomatitis can have several causes, and when treating one, a completely different disease can develop.
It may not be stomatitis at all, but, for example, a simple allergy or herpes.
Active substances contained in both medications and medicinal plants may cause allergies or be contraindicated for some people.
Literature
- Khomenko L. A. Therapeutic dentistry of children. Textbook for university / ed. 2007 – pp. 643-722.
- Ismailova G. T. Chronic recurrent aphthous stomatitis // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. — P. 124-125.
- Drobotko L.N., Strakhova S.Yu. Acute stomatitis in children // Issues of modern pediatrics. - 2010. - T. 9. - No. 2. - P. 146-149.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Toktosunova S. A., Tsepeleva A. S., Sooronbaev A. A. Prevalence and structure of the incidence of stomatitis in children // Bulletin of Science and Practice. 2022. T. 4. No. 11. — P. 91-96.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Zhumashova N. K., Yuldasheva G. I. Complex therapy of inflammatory diseases of the oral mucosa in children // Bulletin of Science and Practice. 2022. T. 5. No. 5. — P. 96-104.
- Pankrusheva T.A., Maravina I.N., Chekmareva M.S. Research on the development of the composition and technology of tablets for the treatment of stomatitis // Scientific result. Medicine and pharmacy. – T.4, No. 1, 2022. – P. 78-87.
- Instructions for medical use of the drug HEXORAL® aerosol: , .
- Instructions for medical use of the drug HEXORAL® solution: , .
- Instructions for medical use of the drug HEXORAL® TABS: , .
- Instructions for medical use of the drug HEXORAL® TABS CLASSIC: , .
- Instructions for medical use of the drug HEXORAL® TABS EXTRA: , .
Up to contents
Symptoms of the disease and its complications
Aphthous stomatitis does not begin with the formation of ulcers. The stages of the disease are:
- The lymph nodes become inflamed, the temperature rises and general weakness occurs.
- Small blisters form in the mouth, which spontaneously open and turn into aphthae.
- Salivation increases.
- At first, it is unpleasant for the patient to eat food with a pronounced taste, and then chewing any food causes pain.
- With a persistent form of aphthous stomatitis, the lymph nodes become inflamed and become painful on palpation.
- The mucous membranes of the mouth are loose and inflamed.
- A white coating appears on the tongue.
- At the final stage of the disease, aphthae scar, and soreness in the mouth disappears.
If the patient has not received adequate treatment, aphthous stomatitis becomes chronic. Wherein:
- The mucous membranes swell and turn pale.
- Aphthae grow and cover the inner surface of the cheeks, palate and back of the tongue. In advanced forms, the ulcers rise above the surface of the oral mucosa.
- Without receiving proper treatment, the growth of ulcers resumes every two weeks. The wounds bleed and penetrate deeper into the tissues of the mouth.
- When healing, erosions leave deep scars.