One of the most common diseases of the oral cavity is stomatitis. This is a pathology that most often takes an infectious-inflammatory course and is the result of increased activity of lymphocytes in response to the ingress of pathogenic molecules that the child’s body cannot recognize. Decreased immunity is the main factor that provokes inflammatory processes in the mucous membranes of the oral cavity. In newborns and infants of the first year of life, the immune system continues to improve and cannot cope with all negative factors, therefore children under one year of age are considered the most vulnerable group of patients for the development of various forms of stomatitis.
Stomatitis in babies
Treatment of stomatitis in infants differs from therapy that may be recommended for an adult, so you cannot prescribe medications yourself. This is also due to the fact that stomatitis has several varieties, each of which differs in clinical course, symptoms and characteristics of the therapy. To correctly determine the type of disease, laboratory diagnostics (scraping from the tongue and gums) may be required, so if symptoms of stomatitis are detected in an infant, you should immediately go to the hospital. The pathology is treated by a local pediatrician or pediatric dentist.
Childhood stomatitis - how to help your baby?
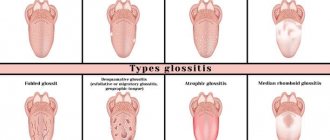
Types of stomatitis common in children?
Treatment of stomatitis will directly depend on the correct diagnosis of the form of the disease and the severity of its manifestation. Below are the forms of stomatitis that are most common in children.
- Herpetic stomatitis in a child is expressed by multiple small or merging blisters, gradually turning into erosions with a white-gray coating.
- Aphthous stomatitis in children is one, two or three elements of a round-shaped rash (aphtha) with a diameter of 5-10 mm with a red rim around.
- Candidal stomatitis in infants is a whitish “curdled” coating on the tongue or cheeks, tightly fused to the mucous membrane.
- Angular stomatitis , seizures - erosions with crusts in the corners of the mouth.
Children may also encounter toxic-allergic, bacterial, erosive, and many types of specific (arising against the background of a specific infection) stomatitis, but the most common are acute herpetic, chronic recurrent herpetic, chronic recurrent aphthous and angular stomatitis.
What is stomatitis?
Stomatitis is the general name for a large group of diseases of the oral mucosa, which are characterized by a general picture of inflammation, as well as the appearance of specific rash elements on the mucosa (depending on the type of stomatitis).
This disease can occur in both adults and children, with the only difference being that some types of “adult” stomatitis do not occur in children (prosthetic stomatitis or stomatitis associated with smoking).
What are the causes of stomatitis in children and infants?
In children and infants, in most cases, the cause of stomatitis is infection. Stomatitis is often associated with ARVI, although the virus is not directly involved in stomatitis.
Stomatitis occurs against the background of a decrease in general immunity, against the background of local immunity in the oral cavity, and can also occur due to injury and subsequent infection of the mucous membrane. With general diseases (acute respiratory infections, acute respiratory viral infections, severe systemic diseases), the body’s overall resistance decreases, which contributes to the development of stomatitis. With viral infections accompanied by a runny nose and cough, the oral mucosa dries out, resulting in a decrease in local resistance - this also contributes to the development of stomatitis.
Main indicators of the disease
Stomatitis in the mouth of a baby manifests itself as follows:
- excessive moodiness, tearfulness;
- increased body temperature (from mild to severe);
- formation of whitish plaque in the mouth;
- the appearance of small blisters resembling ulcers;
- redness of the mucous membrane around the rash, increased swelling;
- difficulty swallowing;
- loss of appetite;
- diarrhea, nausea.
It is not at all necessary that all the manifestations occur at once: sometimes one or several symptoms are enough for the pediatrician to make such a diagnosis and select a course of treatment.
Herpetic stomatitis in children
Causes
This is an infectious stomatitis that occurs under the influence of the herpes virus. There are acute and chronic recurrent herpetic stomatitis. Acute herpetic stomatitis occurs when a child is first infected and occurs most often between the ages of 6 months and 3 years. In 100% of cases, the child gets the infection from parents and other close people (when they lick the child’s spoon and continue to feed him further, lick the pacifier or drink from the same cup). At this age, the child no longer has the antibodies that he gets from his mother’s milk, and has not yet developed his own. Therefore, when a virus enters the body, a disease inevitably begins. In its acute form, such an infection manifests itself in only 10% of children, and all the rest tolerate the primary infection quite easily.
Chronic recurrent stomatitis is due to the fact that the herpes virus, once entering the body, settles there forever and under favorable conditions (the above-mentioned decrease in immunity) can provoke repeated rashes.
The symptoms of acute and chronic herpetic stomatitis are different. In both forms, there are general phenomena (in the body as a whole) and a specific picture in the oral cavity.
Symptoms
Acute herpetic stomatitis
- General deterioration in health. Acute herpetic stomatitis is characterized by weakness, headache, pain in joints and muscles, malaise - general symptoms of intoxication caused by viral activity. The temperature is usually raised to 37 -41 degrees in the first or second day. The lymph nodes (especially the submandibular ones) enlarge and become painful.
In the oral cavity there are:
- swelling;
- redness of the mucous membrane;
- soreness of the mucous membrane in the cheeks, lips, tongue, palatine arches;
- small (the size of a millet grain) bubbles, usually collected in groups filled with a clear liquid; over time, the liquid becomes cloudy, and after 2-3 days the bubbles burst, and a bright red erosion forms in their place. Even later, the surface of the erosion becomes covered with a fibrinous coating (whitish or yellowish). These white spots are surrounded by a red corolla.
- Redness and swelling of the gum edge around the teeth and redness of the interdental papillae are often observed (clinic of gingivitis).
Along with rashes in the mouth, rashes are often observed at the border of the red border of the lips and skin or at the border of the nasal mucosa and skin.
Chronic herpetic stomatitis
All symptoms in the oral cavity repeat the picture of acute herpetic stomatitis, but the general condition, as a rule, does not suffer.
Factors that provoke exacerbations of chronic herpetic stomatitis:
- acute respiratory infections, acute respiratory viral infections, hypothermia;
- avitaminosis;
- allergy;
- stress;
- taking immunosuppressive drugs;
- exacerbation of chronic tonsillitis, sinusitis and other diseases;
- trauma to the oral mucosa;
- foci of infection in the oral cavity (carious teeth, hard and soft dental plaque, gingivitis);
- breathing through the mouth (due to this, drying out of the mucous membrane occurs, which provokes a decrease in local immunity, as well as the formation of cracks on the lips).
Treatment of herpetic stomatitis in a child
Be sure to consult a dentist for an accurate diagnosis. If it is not possible to see a doctor on the first day, you can start treatment, but a visit to the doctor as soon as possible is required.
Antiviral therapy (to combat the pathogen)
- Acyclovir (tablets) or Viferon (gel, suppositories) - depending on the age of the child. Suppositories are more suitable for infants and children up to one year old; older children can be given tablets or treated with gel.
- For rashes that are observed only on the skin, antiviral ointments are used (acyclovir, Viferon, Zovirax and others).
Antiviral drugs are taken according to the regimen specified in the instructions. The sooner you start taking the drug, the more active it will be against the virus. These drugs are taken on days 1-4 of the disease.
Antiseptic treatment (prevention of complications)
- Miramistin (rinse aid) is used directly as a rinse. For young children who cannot yet rinse their mouths themselves, wiping with a gauze swab dipped in a solution of the drug is used. Other antiseptics are either not used at all (since they are not effective against viruses), or are used in combination with miramistin (alternately). You can take chlorhexidine, givalex, rotokan, chlorophyllipt, but all this is only in combination with miramistin.
Keratoplasty (drugs to stimulate mucosal healing)
- solutions of vitamins A and E (you can buy an oil solution at the pharmacy). Applications are made after rinsing with an antiseptic (the drug is applied to a gauze turunda and the wound surface is lubricated).
- rosehip or sea buckthorn oil. Also in the form of applications.
- solcoseryl (after rinsing, apply a thin layer of gel using an ear stick or a clean finger).
One of these drugs to choose from.
Symptomatic treatment
- If soreness of the mucous membrane interferes with eating and hygiene - Dentol or its analogues (drugs used in children during teething) - lubricate the surface of erosions before eating or brushing teeth.
- If the temperature is above 38 degrees - paracetamol, nurofen, ibuprofen, mefenamic acid or any other antipyretics (according to the instructions).
- drinking plenty of fluids to reduce symptoms of intoxication;
- diet excluding spicy, salty, sour, hard foods, allergens (citrus fruits, chocolate, honey);
- Immunostimulants: imunal, amiksin, imudon and others - as prescribed by a doctor.
Causes
Herpetic stomatitis, or as it is also called aphthous stomatitis, is dangerous, first of all, for young children. It is a serious viral disease, which, in addition to damaging the oral mucosa, causes general intoxication of the body and provokes malfunctions of the nervous, immune, and reticuloendothelial systems.
Herpes, which is the causative agent of the disease, may not make itself felt for a long time, although infection usually occurs in early childhood.
When the baby’s immunity is weakened, the herpes virus is activated and begins to multiply, causing an increase in temperature, enlargement of the submandibular lymph nodes, acute inflammation of the mucous membrane, and the formation of bleeding and painful ulcers on its surface.
Main reasons:
- decreased baby's immunity;
- previous infectious diseases;
- lack of vitamins;
- insufficient oral hygiene;
- direct contact with patients with herpes stomatitis.
Infants are more likely to become infected with the herpes virus during childbirth, provided the mother has a herpes infection. In children under one year old and school-age children, the virus is activated against the background of an organism weakened by disease and vitamin deficiency.
Chronic aphthous stomatitis
Causes
Aphthous stomatitis is caused by staphylococcus, a microorganism that is found in large quantities in dental plaque and lives in carious cavities. Every person has this microbe and usually does not manifest itself in any way, but against the background of immune disorders. Often aphthous stomatitis can develop against the background of allergies, gastrointestinal diseases or injuries to the oral mucosa. Another factor in the development of the disease is dirty hands. This disease is often associated with children putting unwashed toys into their mouths, thereby increasing the total number and variety of microbes in the mouth.
Symptoms
Most often, manifestations of chronic aphthous stomatitis occur on the lips, transitional fold, gums, under the tongue and on the tongue - in places where the mucous membrane can be injured by teeth or spicy food.
- Minor change in general health. Characterized by enlargement of the submandibular lymph nodes, fever and weakness.
- On an externally unchanged mucosa, aphtha appears - a spot 5-10 mm in size, slightly rising above the surface of the mucosa, covered with a whitish film tightly fused to the mucosa and surrounded by a bright red rim. Aphthae are very painful when touched. Most often there are one or two aphthae, less often – several.
Must remember! It is necessary to accurately determine the type of stomatitis: herpetic or aphthous. With herpetic stomatitis, there are many small blisters that turn into erosions and sometimes merge with each other, and rashes on the lips are possible. With aphthous rashes, larger, single rashes occur only in the mouth. If you have stomatitis, you should definitely consult a dentist to determine the type of stomatitis and choose the right treatment tactics.
Treatment
Elimination of the factor that caused the disease:
- exclude all allergens (citrus fruits, chocolate, brightly colored foods...);
- if you are taking medications that can cause allergies, then you also need to take this into account (tell your doctor what you are taking and for how long);
- exclude rough, spicy, salty, sour foods;
- if stomatitis is caused by allergies, antihistamines (suprastin, loratadine) are prescribed;
- If the aphthae is due to injuries from sharp edges of a tooth or filling, it is necessary to put the tooth in order.
- in the first 3-4 days, treatment of aphthae is carried out exclusively with antiseptics (rinses, gels). You can use chlorhexidine, rotokan, miramistin, givalex, stomatidine, listerine, chamomile and calendula decoctions - you can take any of these drugs (or any other analogue). Use according to the instructions (there are preparations in ready-made form, and there are those that need to be diluted). Rinse (or wipe the mucous membrane in small children) 3-4 times a day.
- after 3-4 days, epithelializing agents are added: solutions of vitamins A and E, rosehip or sea buckthorn oil, solcoseryl.
- If relapses occur frequently, you should pay attention to your general health. In some cases, only joint treatment with an immunologist, gastroenterologist, endocrinologist and other specialized specialists can help cope with the disease.
Must remember! Aphthous stomatitis is, first of all, a microbial lesion. Oral hygiene, adherence to personal hygiene rules, as well as timely treatment of caries, caries complications, and removal of tartar in many cases are sufficient to avoid aphthous stomatitis.
How to treat: drug therapy
Treatment of stomatitis should always begin with identifying the cause and causative agent of the disease. If an infant is diagnosed with a viral form of stomatitis, the doctor may prescribe the use of antiviral agents in the form of ointments, gels or creams. They must be applied 2 to 4 times a day to previously cleansed mucous membranes. To clean and disinfect the oral cavity, you can wipe the gums, tongue and surface of the cheeks with a light cloth moistened with a decoction of calendula or oak bark or an antiseptic solution, for example, Chlorhexidine.
"Chlorhexidine"
Ointments that can be used to treat infants:
- "Oxolinic ointment";
- "Tebrofen ointment";
- "Viferon";
- "Gerpferon";
- "Acyclovir".
"Oxolinic ointment"
"Viferon"
For severe symptoms of viral stomatitis, a specialist may recommend combined regimens. Including the local use of antiviral ointments and the use of interferon-based rectal suppositories (“Viferon”).
To treat bacterial and fungal stomatitis, agents with a wide spectrum of antimicrobial activity are needed. They can be used in the form of solutions, ointments or suspensions. Levorin and Nystatin suspensions have a good therapeutic effect. To destroy the fungus of the Candida family, the drug of choice is the Candide solution - it quickly copes with pathogenic flora and reduces the intensity of painful sensations after 2-3 days of use.
"Nystatin"
For bacterial stomatitis, it is necessary to treat the mucous membranes with any antiseptic solution 3-4 times a day. This can be “Miramistin”, “Chlorhexidine”, “Furacilin” (to prepare the solution you need to dissolve 1 tablet of “Furacilin” in 140 ml of hot water). The following medications can be used to heal and moisturize soft tissue:
- Which doctor treats stomatitis?
- "Vinilin";
- "Bura";
- Vitamin A in a gelatin shell.
"Vinilin"
If a child has a fever, it is better to use paracetamol-based products. It is better to give the drug to children older than three months in the form of a syrup with orange or strawberry flavor. Cefekon rectal suppositories are good for reducing fever and relieving pain, but they cannot be used for up to three months. If you need to bring down the temperature of a newborn, it is better to use products that contain ibuprofen - Nurofen or Ibuprofen.
"Ibuprofen"
Important! Antibiotics for the treatment of stomatitis are prescribed extremely rarely. If treatment is started at the initial stage of the pathology, in most cases it is possible to do without the use of potent antibacterial drugs. Only a doctor should prescribe and select the dosage of medications in this group.
At the dentist
Candidal stomatitis in children (infants)
Cause
This type of stomatitis appears due to fungi, which are constantly present in the microflora of the oral cavity, but usually do not manifest themselves. Against the background of microflora disturbance (due to licking dirty toys, treatment of other diseases with antibiotics, acute respiratory infections, acute respiratory viral infections, during treatment with corticosteroids and other drugs that suppress the immune system, as well as with a high-carbohydrate diet), the growth of fungi of the genus Candida, which is the cause of stomatitis, is activated in infants.
Symptoms
- a whitish or yellowish cheesy coating on the tongue, cheeks, and gums, which is easily removed. It is important to remember that young children who are breastfed and whose diet is dominated by dairy products may have a coating of milk on their tongue - this is normal and does not need to be treated.
- when removing plaque, the mucous membrane is swollen, slightly red, and may be painful.
General health is usually unchanged.
When it becomes chronic, dryness and pain occur in the mucous membranes, and swallowing is difficult.
Treatment
- Candida mushrooms are well preserved in the external environment. It is necessary to wash all toys, bottles, dishes, pacifiers and other objects with which the child comes into contact with soap or soda.
- In the oral cavity, plaque is easily removed with a solution of soda (1 teaspoon of soda per glass of cold boiled water) - use a gauze swab to wipe the areas where there is plaque.
- Antiseptics (furacilin, decoctions of medicinal herbs, chlorhexidine) - rinsing or wiping the mucous membrane 3 times a day.
- Diet correction (exclude sweet, spicy, sour foods as much as possible).
- Local antifungal drugs (cholisal - spread on the mucous membrane 3 times a day after removing plaque, hexoral - dissolve a tablet (for children over 4 years old) and others). Carefully read the instructions for use and age restrictions.
- If improvement does not occur within 3-4 days, then you should consult a doctor to prescribe antifungal drugs for general treatment, as well as to identify possible concomitant pathologies.
Treatment
Therapy for stomatitis in children involves general rules that are mandatory for all types of the disease, and drug treatment aimed at eliminating the underlying cause.
Treatment should be prescribed by a pediatrician after examining the child, collecting the necessary information and identifying the causative agent of the infection.
General recommendations
General recommendations for treating stomatitis in young children include:
- Drink plenty of fluids (it is allowed to give the child unsweetened compotes and decoctions, but it is best to persuade the child to drink plain water).
- Regular ventilation.
- Air humidification in a children's room.
- Excluding refined and sweet foods from the child’s diet. If your baby is receiving complementary foods, you should avoid fruit purees made from sweet fruits (bananas) and cereals with added sugar.
- Medications depending on the type of stomatitis
For young children, lotions with chamomile decoction are used, which help relieve inflammation, have an antiseptic effect, and reduce pain.
Victoria Druzhikina
Neurologist, Therapist
Treatment of Herpetic stomatitis
Therapy for this type of disease is carried out in three stages:
- relieving irritation and eliminating the inflammatory process;
- healing of wounds formed after opening ulcers;
- fighting the virus and activating the body’s immune reserves.
To treat herpetic stomatitis in children under 3 years of age, antiseptic treatment of the oral cavity is used, after which antiviral medications are applied. Given the young age, rinsing with special infusions and solutions is excluded.
To treat the affected areas, you need to moisten a cotton swab with a solution of Furacilin (Rivanol) and gently wipe all the places where the rashes are localized. After this, you can begin applying ointments (for example, “Oxolinic” or “Interferon”) . The procedure is performed every three hours, unless a different treatment regimen is recommended by the pediatric dentist.
Doctor's advice
In the case of bacterial stomatitis, treatment with a solution of chlorhexidine bigluconate 0.05% is effective. If the child is small, then moisten the cotton wool, squeeze it out and wipe the affected area. Make sure that the drug does not flow from the cotton wool into the child’s throat. Processing is carried out 2-3 times per day. If the child knows how to rinse his mouth, then rinse 3-5 times a day. Hydrogen peroxide solution should not be used to avoid burns.
Victoria Druzhikina Neurologist, Therapist
When herpetic stomatitis is diagnosed in a child aged 1 year (or younger), parents do not always cope with antiseptic treatment measures. If it is not possible to treat the cavity with a tampon, you can purchase a special brush for young children (from 4 months), which is placed on the finger, wrap it in gauze and lubricate the affected areas.
Restoring immunity and fighting herpes viruses occurs with the help of medications (Arbidol, Acyclovir, Imudon). To heal wounds, you can lubricate them with sea buckthorn oil or rosehip oil.
Treatment of Candidal (fungal) stomatitis
Drugs with antifungal effects can only be prescribed to older children, so treatment of candidiasis in children under 3 years of age is predominantly local.
Newborn children can be prescribed medications such as Candide, Nystatin or Clotrimazole - these drugs are safe for children and can be used from the first days of a baby’s life.
In a clinic setting, a doctor may prescribe an irrigation procedure (irrigation of the oral cavity) using sodium bicarbonate in the form of a 2% solution, followed by treatment with sodium borate (10%).
An important condition is maintaining oral hygiene and regular treatment of lesions (plaque removal). This can be done using a soda solution (2 tablespoons of soda per mug of warm water). This procedure will help restore the alkaline environment, which is detrimental to yeast-like fungi. At home, it is recommended to repeat it at least 4-6 times.
Treatment of Bacterial Stomatitis
Treatment of bacterial stomatitis (often occurring at 2-3 years of age) is aimed at destroying bacteria that cause the development of the disease and deterioration of the baby’s well-being.
Severe cases require taking antibiotics, which are prescribed by a pediatrician after taking a smear to determine the causative agent of the disease and its sensitivity to various pharmacological groups of antibiotics.
For local treatment, you can use antibacterial sprays (Tantum Verde, Hexoral, etc.). Treatment must be combined with antiseptic treatment.
Allergic stomatitis
This type of stomatitis, in addition to hygiene measures, includes taking allergy medications and antihistamines (histamine blockers). Young children can use Tavegil or Suprastin for these purposes - both drugs are in drops.
Treating stomatitis in young children is not the easiest task, but it is quite feasible. To do this, you need to consult a doctor in time, follow his recommendations, monitor the baby’s nutrition and hygiene, and not make any changes to the treatment regimen on your own. The use of traditional methods should only be carried out with the permission of a doctor after examination and an accurate diagnosis.
To learn how to recognize and treat stomatitis in a child, watch the video:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://stgmu.ru/userfiles/depts/therapeutic_dentistry/Obyavleniya/stomatity_2013.pdf
Rate how useful the article was
5 Voted by 1 person, average rating 5
Did you like the article? Save it to your wall so you don’t lose it!
Angular stomatitis in a child
Causes
In children, seizures are most often a manifestation of allergies, and can also appear while taking antibiotics. The mechanism is as follows: when using antibiotics, the microflora of the oral cavity is disrupted (both harmful and beneficial microbes die), against this background, space is freed up in which Candida fungi settle. It is these fungi that eventually cause the formation of buttocks.
Similar erosions can appear against the background of herpetic lesions, injuries, allergies, dry lips and cracks. It is important to determine the cause of their appearance and only then prescribe treatment.
Symptoms
Angular stomatitis (jams) - erosions with crusts that appear in the corners of the mouth - is also a fairly common form of stomatitis.
Treatment
- Antiseptics (chlorhexidine, miramistin) - use a gauze swab or ear stick to treat the surface of the wound.
- Keratoplasty (solcoseryl, oil solution of vitamins A and E) - applied to a dry surface after antiseptic treatment.
- Fighting the cause of the disease (if it is an allergy, we remove the allergens and prescribe antihistamines, if it is due to antibiotics, we prescribe drugs to restore the microflora and antifungal ointments, etc.).
How long does the disease last and how many days is the child contagious?
Depending on the complexity of the form, herpes stomatitis in children lasts from several days to 2-3 weeks. With a mild form, the main symptoms disappear on the third or fourth day, treatment of a moderate form takes one to two weeks. The severe form is the most dangerous; healing lasts for weeks and requires mandatory hospitalization of the baby.
The disease is characterized by a high degree of contagiousness precisely during the period of exacerbation.
The infection is transmitted by airborne droplets (including through kissing), when using shared dishes, cutlery, toys, and hygiene items.
Herpes is contagious and can easily be transferred to healthy parts of your own body.
It is necessary to wash your hands thoroughly after treating the surface affected by the sores with medications to prevent the spread of the virus.
Folk remedies
Traditional healers do not offer anything for the treatment of stomatitis in Samara : there are onions with garlic, and aloe, and a decoction of onion peels, and peroxide with water, and honey, and propolis and ... hundreds of other variations on the theme of anti-inflammatory substances. All this is very good, but does not exclude standard treatment, since all these substances act primarily on the consequences - on inflammation, but do not act on the pathogen. Rosehip and sea buckthorn oils are successfully used to heal erosions (the pharmacy equivalent is a solution of vitamins A and E), chamomile, aloe and other plants are used as antiseptics and anti-inflammatory, but their effect is rather weak.
The only thing that deserves attention:
- Rinse with raw egg white. 1 protein is dissolved in 100 ml. water and rinse with this solution (or lubricate the mucous membrane in infants). The protein contains a lot of lysozyme, which helps increase local immunity and helps fight infection. But the other side of the coin in this method is the danger of salmonella infection, so it is difficult to say whether it is worth the risk.
Causes of purulent-inflammatory pathologies
Gingivitis
Gingivitis in children occurs due to regular poor oral hygiene, accumulation of plaque, and deposition of stones. The situation is aggravated by factors such as crowded teeth, malocclusion, installed braces and other orthodontic structures.
Ulcers are formed due to untreated caries and improper oral care.
A fistula is the result of neglected infectious processes, a consequence of improper treatment of dental diseases.
What symptoms should parents be wary of?
The first signs of unhealthy gums are bad breath and bleeding when brushing your teeth.
Upon examination, you can see reddened areas above the teeth. Pus does not always provoke a rise in overall body temperature. Swelling of the face or pain in the initial stages is mild or absent.
Abscess
An abscess on the gum of a child is distinguished by the specificity of its symptoms - a feeling of local distension, pain, the formation of a tubercle, where decay products gradually accumulate in the form of a foul-smelling liquid. As the disease progresses, physical activity decreases and appetite disappears.
Treatment methods
Important! Self-treatment of a fistula on the gum of a child, or other diseases in the form of rinses, lotions, and ointments is unacceptable. This is dangerous due to such consequences as gumboil, loosening and loss of permanent teeth, and periodontal disease. In severe cases - transition to a chronic condition, decreased immunity, frequent viral infections of the body, partial or complete paralysis of the facial nerve.
Fistula
At the dental clinic "Podmoskovye" we take a professional approach to treatment, which includes the following stages:
- detailed diagnostics - examination, instrumental examination;
- drawing up a treatment plan in a clinical setting;
- Recommendations for caring for your oral cavity at home.
Only an integrated approach will preserve the health of the oral cavity until the dental system is fully formed.
Read more about our pediatric dentistry in the Pediatric Dentistry section