Our teeth are not only dense organic tissues covered with hard tooth enamel. Hidden inside each tooth is a complex system of blood vessels and nerve endings, which is necessary to maintain the health of the dentition. The sensitivity of soft tissues in the oral cavity is tens of times greater than the sensitivity of other organs. Therefore, any infection that gets inside the tooth causes inflammation and severe pain. Pathology is also provoked by temperature changes: burns or hypothermia. Unbearable pain forces a person to treat pulpitis and seek help from a dentist.
Will we treat him or let him live?
Often the fear of doctors forces us to make do with improvised methods. We take painkillers, fast, endure, in the hope that the sharp pain will go away on its own. Is it really possible to “wait out” an exacerbation, or is it better to get professional help in time? Let's figure it out.
To find the right method of treating a disease, you need to know the origins of its occurrence. The core of the tooth, or pulp, is responsible not only for tooth sensitivity, but also for the production of dentin. The tissue strengthens the tooth from the inside.
The anatomical features of the pulp depend on the type of teeth. In the lateral row, as a rule, there is a chamber with three dental canals. The front row and incisors each have one branch. It is logical that molars are much more difficult to treat than canines or premolars.
Pathological changes in the pulp tissue form swelling, causing unbearable pain. The pain intensifies upon contact with hot food or when pressing on the tooth.
Acute pulpitis
Acute pulpitis, as we have already said, is characterized by severe toothaches that occur WITHOUT a reason and intensify at night. The main symptomatic difference between acute pulpitis and caries is that pain in deep caries is always associated with an irritant, and stops when the action of the irritant is interrupted. The pain associated with pulpitis is pulsating, not associated with impact on the tooth, is difficult to relieve with tablets, and radiates to the ear, jaw, and temple. It is difficult for the patient to determine which tooth hurts; usually he complains that half of the jaw hurts.
There are several forms of acute pulpitis, depending on the location and manifestations of the inflammatory process:
| Forms of acute pulpitis | What is the difference? | Nature of pain |
| Focal | Inflammation of the coronal part of the pulp | Paroxysmal severe pain that radiates to the jaw. |
| Diffuse | Inflammation of the entire pulp | The pain lasts 10-15 minutes with a break of several hours. Symptoms are worse when lying down. |
| Serous | Very severe inflammation in an advanced stage | Continuous throbbing pain. |
| Purulent | Pus forms in the dental canals | Under the influence of warm food or drink, the pain intensifies, and cold food relieves it. |
Prerequisites
The most common cause of inflammation of the dental nerve (pulp) is the presence of caries. And in a deep stage. The infection reaches the soft tissues through the destroyed tooth tissue, provoking an inflammatory process. A similar situation occurs when a filling falls out or is damaged, when the pulp is “exposed.”
Bacteria can enter the tooth cavity from another source of infection in the body. Inflammation also occurs when a tooth is injured, minerals accumulate in the pulp, or low-quality components are used when filling canals.
Also, treatment of pulpitis may be required if the nerve overheats during preparatory procedures for prosthetics. If there is increased sensitivity, swelling of the pulp can be caused by the use of chemicals during therapy. It is also possible that an infection may accidentally enter the pulp chamber when eliminating a carious cavity.
How does pulpitis form?
Pulpitis refers to inflammatory processes that develop in the pulp – the neurovascular bundle. The inflammation itself can be a consequence of mechanical damage to the pulp, for example, as a result of mistakes made by the doctor during canal filling, or injury after a blow or fall.
However, almost always pulpitis becomes the result of severely advanced caries, in which pathogenic bacteria from the carious cavity penetrate into deeper layers and reach the pulp. It is they who cause the rapid destruction of the neurovascular bundle - this is how pulpitis develops, and irritation of the nerve endings provokes acute pain.
Important! The best decision that can be made in case of pulpitis is to immediately consult a doctor. Even better is to make a visit to the clinic, where the treatment will be carried out using a microscope. This optical magnifier will help preserve the tooth for many years and eliminate the risk of re-inflammation. With a microscope, you can remove the nerve without leaving any residue, efficiently pass through, process and fill the root canals without damaging healthy tissue or perforating the root walls. In addition, the device allows you to save a tooth and correct mistakes made by unqualified doctors earlier: using the device, you can carefully remove tool remains from the roots, refill canals, close holes and perforations.
Phases of the disease
Classification of any disease contributes to quick and correct diagnosis and selection of an effective treatment method for the patient. In the case of pulpitis, everything is relatively simple, there are only two subtypes - acute and chronic.
The first type of inflammation occurs with advanced forms of caries. Bacteria destroy tooth enamel and dentin, and the infection enters the pulp. The disease is accompanied by aching, sharp pain, which intensifies with mechanical or thermal effects on the tooth. Severe pain attacks may occur at night.
Interestingly, only adults are susceptible to acute pulpitis. The anatomical structure of a child’s jaw protects him from illness.
This type can be focal or diffuse. Focal inflammation is characterized by local damage to the pulp, located close to the carious cavity. Accompanied by throbbing pain around the affected tooth. Lasts approximately 2-3 days.
Then the process moves to the next stage - damage to all tissues of the dental nerve. The pain syndrome changes from pulsating to constant, unpleasant sensations spread to the entire jaw. Pus forms in the tooth cavity. The phase lasts no more than two weeks. If timely treatment of pulpitis is not started, the pathology enters the chronic stage.
Lotions, rubbing and other procedures
Treatment of dental pulpitis with folk remedies also involves other methods of therapy:
- mouth baths;
- lotions;
- compresses;
- rubbing.
Mouth baths
Almost all decoctions and infusions that are used for rinsing can also be used for oral baths. Place a warm but not hot solution in your mouth, hold it, and spit it out. Repeat every one and a half to two hours.
Lotions and compresses
Soak a cotton pad or gauze napkin in the healing decoction, squeeze lightly, apply to the gum near the tooth affected by pulpitis, and hold for several minutes. Repeat 3-5 times a day.
Rubbing
Apply a paste or cream prepared from medicinal natural ingredients to the gums and rub in with light massage movements until completely absorbed.
You should not overuse rubbing, as they can cause irritation of the mucous membrane; 2-3 procedures per day are enough.
Eliminate cannot be deleted
A term that patients in all fields of medicine fear is chronic disease. Let's see what the consequences are in our case. Inflammation of the dental nerve with chronic pulpitis lasts from a month to several years. The pain syndrome remains, but becomes less pronounced. Seizures occur periodically. The patient can no longer chew on the side of the diseased tooth. The affected nerve begins to bleed and dentin continues to deteriorate. Chronic pulpitis is also characterized by several phases:
- Fibrous. Relatively “easy” stage. It occurs when carious tissues are not located close to the dental nerve. Unpleasant sensations occur only when you press on the tooth.
- Gangrenous. The pulp tissue is completely infected. The nerve changes color. The pain becomes more noticeable. The tooth is deeply affected by caries.
- Hypertrophic. Bacteria destroy the tooth down to the pulp chamber, connecting both cavities. A polyp grows in the vacated space, causing the nerve to bleed. The pain syndrome persists.
- Exacerbation. The final stage of the disease, when the patient is attacked by periodic attacks of pain, combined with constant aching unpleasant sensations. Pus appears in the tooth cavity, inflammation spreads to the tooth root, and periodontitis develops.
In 90% of cases, doctors treat fibrous pulpitis, less often - the second stage. In general, chronic inflammation is an irreversible process. The only solution is to remove the damaged dental nerve.
What is pulpitis?
Pulpitis is inflammation of the dental pulp. Most often, this disease is caused by dental caries. Inflammation of the dental pulp can also develop as a result of dental trauma when the enamel or crown of the tooth breaks. The habit of grinding your teeth (bruxism) can also contribute to inflammation of the pulp. The disease can also be caused by multiple procedures performed on a single tooth (eg, grinding teeth in preparation for crowns or denture bridges, excessive pulp exposure when treating a deep tooth defect).
What is dental pulp?
Pulp is the internal tissue that contains the blood vessels and nerves of the tooth. A healthy and living pulp is a kind of protective barrier; it protects the body from the penetration of harmful bacteria. On the other hand, when a tooth becomes infected, the inflamed pulp becomes a spreader of the disease.
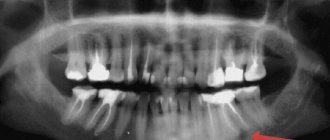
Survey
To determine an accurate diagnosis, the dentist conducts an initial examination. Because If pulpitis develops against the background of other diseases, then diagnosis includes 4-5 stages. The procedure begins with communication with the patient. It is important to understand at what stage the inflammation is, which is especially important in chronic pulpitis. Therefore, the doctor asks you to describe in detail the nature of the pain. Then a “manual” examination is carried out using medical instruments (dental mirror, etc.). Additionally, the doctor checks the sensitivity of the affected tooth for temperature changes and exposure to a weak electric current charge.
The examination is completed by an X-ray examination to assess the condition of the dental nerve and canals. After collecting information and analyzing the image, the doctor plans the pulpitis treatment process and coordinates it with the patient.
Complications of pulpitis
Untimely treatment of acute pulpitis leads to a chronic process. A hidden infectious focus is formed in the body, which can provoke the appearance of both new dental diseases and general ailments, such as:
- flux - periostitis, purulent inflammation of the periosteum,
- osteomyelitis - inflammation of the bone tissue of the jaw,
- purulent inflammatory processes of intraoral tissues and soft tissues of the face,
- dental cyst - a benign neoplasm near the tips of the roots,
- sepsis - blood poisoning,
- The infection spreads to other organs through the bloodstream, with the heart and kidneys most often affected.
These diseases will require surgical or general systemic treatment - in no case should they be allowed to appear.
How to deal with the disease
At the initial stage, it is not difficult to cope with pulpitis. The nerve in the tooth is preserved, and the doctor relieves the inflammation using therapeutic procedures.
The biological treatment method eliminates inflammation through antibacterial treatment of the damaged tooth, without removing the nerve. After removing carious tissue and disinfecting the pulp chamber, the dentist applies a compress with calcium hydroxide and fixes a temporary filling.
Then, after 3-7 days, during a follow-up visit, the doctor takes an x-ray. If there is no inflammatory process, then a permanent filling is installed. However, this technique requires a highly qualified doctor, so it is rarely used. For example, with traumatic inflammation of the dental nerve.
Preserving the pulp is important because... If it is present, the tooth is constantly strengthened due to the production of dentin. Conservative therapy has age restrictions - it is carried out up to 30 years.
Forms and symptoms of pulpitis
Patients usually think that the main sign of pulpitis is pain and a large carious cavity in the tooth, but this is not entirely true.
There are acute and chronic forms of pulpitis, depending on the strength of the inflammatory process affecting the pulp. Severe pain, which is often not relieved by painkillers, is characteristic of the acute form of the disease. But, if it becomes chronic, the pain subsides and practically does not bother you anymore.
As for large “holes” in a diseased tooth, the patient may not see them. Pulpitis also occurs as a result of caries hidden under a thin layer of enamel and under a previously installed filling. The pulp can become inflamed in a tooth without caries, although this happens much less frequently, due to an infection brought into the tooth with blood.
Partial and complete nerve removal
Partial extraction of the pulp is also acceptable if the coronal component of the nerve is separated from the root. To prescribe surgery, there must be a large volume of intact periodontal tissue.
The procedure is performed under anesthesia for patients under 45 years of age.
In practice, pulpitis is treated surgically. The nerve is completely removed, which saves the patient from relapse and re-treatment.
Pulp removal occurs in two ways:
- Extraction of living nerve.
- Preliminary killing of the pulp (devitalization) with further removal.
In the first option, all work is carried out in one session. The dentist removes the affected tooth tissue, thoroughly disinfects the cavity, and then removes the inflamed nerve. At the final stage, a filling is installed.
If it is not possible to remove the living nerve from the tooth, it is treated with medical paste made from arsenic or paraformaldehyde. After 1-2 days, the pulp dies and is painlessly removed. Patients cannot always visit the doctor the next day; in this case, the dentist fixes a less concentrated composition for up to two weeks. A temporary filling is placed on top. During the next visit, the doctor treats the canals with an antiseptic and fills the tooth. Important: this method of treating pulpitis is not applicable in the presence of pus and dead tissue in the pulp.
Complications in the treatment of pulpitis
Although diagnosing pulpitis is not difficult and dentistry has everything necessary for the treatment of pulpitis complications still occur . For example, if a tooth hurts after treatment for pulpitis , this is often due to insufficient antiseptic treatment of the root canal before filling it. Inexperienced dentists may make mistakes when treating pulpitis, which cause pain after pulpitis treatment.
Complications in the treatment of pulpitis include incomplete filling of the root canal; removal of the filling material beyond the apex of the tooth root.
Less common complications of pulpitis treatment are:
- undetected and, accordingly, not sealed additional root canal;
- fracture of an endodontic instrument in the root canal;
- perforation of the root canal wall or tooth wall.
How is therapy carried out?
The process of extracting the dental nerve may require 2-3 visits, depending on the number of roots in the tooth. The time interval between sessions is prescribed by the doctor, in accordance with the diagnosis.
Traditionally, treatment of pulpitis consists of 4 stages:
- Application of local anesthesia. Nerve endings are very sensitive to any impact, so painkillers are indispensable.
- If caries is present, the affected tooth tissues are first removed. Sometimes it is necessary to remove a healthy part of the tooth to gain access to the pulp.
- Using a special tool, a pulp extractor, the dental nerve is extracted. Depending on the stage of the disease, the pulp is pre-treated with arsenic or extracted alive.
- The dental canals are measured and thoroughly disinfected.
After treatment, the tooth is filled: first the root canals, then the upper, coronal part of the tooth. In difficult cases, for example, with chronic pulpitis, the doctor fixes filling materials only in the canals in order to track a possible relapse of the disease. If inflammation reappears, then intermediate therapy is prescribed using antibiotics.
After installation of a permanent filling, the patient may experience pain. This usually lasts no more than 2-3 days, with a reaction to cold foods and drinks. If the discomfort continues, then the inflammatory process has resumed, and you need to visit the dental office as soon as possible.
Rinsing
The most popular procedure that helps get rid of pain, swelling, relieve inflammation, and remove pathogenic bacteria. For rinsing, use a variety of herbal decoctions (sage, chamomile, calendula, bay leaf, willow bark, elderberry, basil, calamus), solutions of hydrogen peroxide, soda, propolis, and alcohol tinctures diluted in water.
Important! The rinse should be warm, but not hot; high temperature promotes the development of purulent inflammation.
Sage
It has an analgesic, sedative and antiseptic effect. You should rinse your teeth and gums with a decoction of sage every 2-3 hours.
Hydrogen peroxide
Excellently disinfects the oral cavity, removes bacterial plaque, and helps localize the inflammatory process. Rinse your mouth with an aqueous solution of hydrogen peroxide several times a day.
Soda
Rinsing with soda allows you to relieve pain for a while and disinfect the surface. You need to dilute a spoonful of baking soda in 200 ml of warm water, rinse 3-4 times a day.
Propolis and calamus
They have an analgesic and disinfectant effect. Mix a tablespoon of calamus with a teaspoon of propolis alcohol tincture and dilute with boiled water. Use for daily rinsing for one month. You can also apply a piece of propolis to a sore tooth; the pain usually goes away within a few minutes.
willow bark
Has anti-inflammatory and analgesic effects. Brew 2 tablespoons of crushed bark, let it brew, strain, use for rinsing and mouth baths.
Bay leaf
It disinfects the oral cavity well and helps relieve swelling. Pour one tablespoon of leaves into a glass of boiling water and let it brew. Use for rinsing.
Elderberry and knotweed
Mix elderberry and knotweed flowers in 1:1 proportions, steam two tablespoons of the mixture in a thermos. Rinse every two hours. Helps with acute pain.
Pomegranate
Excellent prevention of pulp suppuration, relieves inflammation, swelling, pain. Soak the peels of two pomegranates in a water bath for two hours, strain and rinse your mouth 5-6 times a day.
Children's horror stories
The phases of disease progression at a young age are approximately the same. But unlike adults, children's pulpitis develops many times faster. A small hole in the tooth is enough for the infection to cause inflammation in the pulp chamber. Accelerated pathological processes can lead to infection of the soft tissues around the tooth, which can lead to problems with the growth of molars. Therefore, if a child complains of toothache, it is important to consult a doctor immediately.
The question often arises: is it possible to treat pulpitis or is it still necessary to remove the dental nerve in children? An experienced dentist always strives to preserve both the baby tooth and the pulp. Because the absence of teeth in a row can affect the location of neighboring teeth, change the bite, and even diction.
In the case of baby teeth, the dentist uses special filling materials that dissolve over time and do not interfere with the growth of the permanent dentition.
Gentle drugs that are hypoallergenic and safe for babies are used as pain relievers.
Pulpitis in children
Treatment of pulpitis in children follows the same scheme, but there are a number of difficulties here. Firstly, the inflammatory process in the tooth itself occurs very quickly, so it is important to prevent it from spreading to the bone tissue around the tooth. Secondly, a child may experience an allergic reaction to anesthesia during treatment.
Therefore, in the case of children, it will be much easier to initially monitor the condition of the teeth and prevent the occurrence of caries. If your child complains of toothache, you should not put off visiting the dentist. After all, the health of permanent teeth depends on the speed of treatment.
Probably no one wants to get such dental problems. To avoid them, you need to visit the dentist once every six months, have an examination and professional cleaning, eat right, give up bad habits and keep your mouth clean. After all, dental health is only in your hands.
Indications during pregnancy
There is a myth that it is impossible to treat teeth while expecting a baby. This misconception can have serious consequences. Infection, for example in the form of caries, through blood vessels can spread throughout the body.
It is also a mistaken belief that x-rays harm the development of the fetus. It has been proven that modern equipment has a minimal radiation dose that does not affect the body. It is much more dangerous to bring the inflammatory process to a chronic state. Therefore, you should not delay treatment of pulpitis or caries when symptoms appear.
The process of bearing a child is associated with a decrease in immunity, and as a result, with increased sensitivity to bacteria and infections. Tooth enamel in pregnant women is not as strong, because... All nutrients are aimed at the growth of the baby. Therefore, the appearance of pulpitis and deterioration in the condition of the dentition is a normal phenomenon.
The second trimester is considered the optimal period for receiving dental care. During this period, the child is protected by the placenta from harmful substances. However, if an inflammatory process occurs in the dental nerve, it is not recommended to delay treatment so as not to expose the baby to unnecessary risk.
During pregnancy, the doctor chooses a gentle treatment method, when the filling is fixed only in the dental canals. If possible, without the use of anesthesia. After childbirth, the patient is given a permanent filling. X-ray examination is carried out only in emergency cases.
Tooth pulpitis - symptoms and treatment
What can you do about pain before visiting a doctor?
If you notice symptoms of pulpitis, it is best to immediately consult a doctor. If this is not possible, it is possible to use anti-inflammatory or painkillers, but it is worth remembering that this is rather a symptomatic treatment that will help eliminate pain for a while, but will not cause the appearance of pulpitis and will not completely cure it.
Stages of pulpitis treatment
There are several types of treatment for pulp inflammation. Depending on the form of pulpitis, one of the methods is selected. They are divided into two large groups:
- preservation of pulp viability;
- pulp removal.
Preservation of pulp viability can be complete or partial.
1. Conservative treatment of pulpitis. The method of complete preservation of the pulp is called biological. It has the following indications:
- acute partial pulpitis;
- accidental opening of the tooth cavity, i.e. with reversible types of pulpitis.
It eliminates the inflammatory process in the pulp, promotes dentin formation, while maintaining a barrier to bacteria.[1] The biological method is most often chosen at a young age (up to 29 years), with electroodontodiagnostic readings of up to 25 μA and the absence of pathologies on the radiograph.
At the first appointment under anesthesia, mechanical (preparation, removal of soft infected dentin) and medicinal treatment of the carious cavity with various antiseptics, such as chlorhexidine, iodinol and others, is carried out. Next, the cavity is degreased, and a therapeutic pad is placed on the bottom, which contains calcium hydroxide (Dycal, Biolife, Lica, Biopulp, etc.) under a temporary bandage.[2] After 5-7 days, a repeat appointment is scheduled. If nothing bothers the patient, the temporary bandage is replaced with a permanent filling. It is recommended to carry out electroodontic diagnostics and examination after one month, six months of a year and one year. The readings usually recover to 2-12 µA.[1]
2. The method of partial preservation of the pulp is vital amputation . This type of treatment can be used in the following cases:
- acute focal pulpitis;
- chronic pulpitis with electroodontodiagnostic indicators up to 40 μA;
- teeth with an immature root system.
This method of amputation is carried out in multi-rooted teeth, in which there is a significant division into root and coronal pulp. It is also important that periodontal and periodontal tissues are intact (not involved in the process).
The essence of this technique is to excise only the coronal part of the pulp in view of the pulp's ability to regenerate. Local anesthesia is administered, the carious cavity is prepared, and soft dentin is completely removed. Next, the cavity is treated with antiseptic and anti-inflammatory solutions. The tooth cavity is opened with a sterile bur and opened so that after removal of the coronal pulp the orifices of the root canals are accurately identified.
The pulp is amputated using an excavator. During the amputation process, the cavity is also irrigated with anti-inflammatory drugs. To stop bleeding, you can use a solution of hydrogen peroxide, and coagulation is also possible. Next, apply a medicinal paste (identical to that used in the biological method), a glass ionomer cement pad and a temporary dressing. If the patient has no complaints, a permanent filling is placed after about a week.
Methods for complete pulp removal are divided into vital and devital extirpation (removal).
1. Vital extirpation (pulpectomy) is the surgical removal of the entire pulp. This treatment method is suitable for all types of pulpitis.
Endodontic treatment begins with anesthesia, then the carious cavity is prepared. Next, the coronal pulp is removed. The orifices of the root canals are expanded with the help of special instruments, they are shaped into a cone[2], and the pulp is extirpated from the canals. Next, mechanical and medicinal treatment of the root canals begins. The main goal of instrumental treatment is to remove pulp residues, decay products and infected tissues from the walls of the canal, its expansion for high-quality irrigation and subsequent obturation (closure). For root canal irrigation, the first and main solution is Na[6] hypochloride in different concentrations. They also give preference to chlorhexidine, hydrogen peroxide and other solutions. For high-quality treatment of root canals, ultrasonic injection of the above solutions is also used. During instrumentation, various endodontic instruments are used (H-files, K-files, MTWO, Reciproc, Wave One and others).
In certain forms of pulpitis, these stages are completed by temporary obturation of the root canal with anti-inflammatory pastes with an antibiotic (pulposeptin, septomyxin) and a temporary bandage is placed for one to two days. In other cases, treatment is carried out in one appointment. After irrigating the root canals, they are completely dried.
The final stage of endodontic treatment is permanent obturation of the root canals.[10] For this purpose, different filling materials are used. Among their wide variety there are the following options:
- pastes containing zinc oxide and eugenol (“Endomethason”, “Biodent”);[11]
- pastes containing antiseptics and anti-inflammatory substances (“Cresodent”, “Foredent”);
- materials based on epoxy resins (“AN-26”, “AN Plus”, “Toseal”) and others.
Gutta-percha pins are also used for obturation. After obturation, it is necessary to take a control radiograph[12] to ensure that the root canals are obturated all the way to the apical foramen.
If the tooth is severely damaged, strengthening it with pins is recommended. Next comes the procedure for restoring the crown part of the tooth.
2. Devital tooth extraction. The essence of this method is to necrotize the pulp before its removal. This method is indicated in cases where pulpitis cannot be cured by other means due to a number of reasons [13] (allergy to local anesthetics and others).
Treatment is carried out in two doses. At the first visit, soft infected tissues in the carious cavity are removed, the tooth cavity is opened, and a paste is applied to the opened point to necrotize the pulp (it can be arsenic or non-arsenic). Next, the cavity is closed with a temporary bandage and the next appointment is scheduled after 1-7 days (depending on the choice of paste). At the next appointment, the temporary filling is removed, the tooth cavity is opened, the root pulp is excised, and the coronal pulp is removed. Next, treatment is identical to vital extirpation (drug and mechanical treatment, as well as obturation).
Why does a pulpless tooth hurt and how to relieve the pain
After treatment of pulpitis, you may experience pain reactions. Pain can occur due to the removal of the filling material beyond the apex of the root canal, allergic reactions to the filling material, and poor-quality root canal treatment.
Poor treatment of pulpitis most often leads to diseases such as periodontitis (inflammation of the periodontium of the tooth - the tissue around the tooth) and periostitis (inflammation of the periosteum). There are also cases of root perforation or breakage of instruments in root canals; sometimes such situations lead to tooth extraction. If pain occurs, you should contact your dentist.
Is it possible to cure pulpitis with folk remedies?
Traditional methods of treating pulpitis at home without a doctor's prescription can be dangerous.
Features of the treatment of pulpitis in children
Treatment methods for pulpitis in children and adults differ, since the anatomy of primary and permanent teeth is different.
Inflammation of the nerve in the wisdom tooth
Eights have their own specifics, and the doctor often chooses to remove the tooth. The complexity of therapy is due to the anatomical features of the third molars. Curved roots, lack of access to the tooth, partial overlap of the gums equates the treatment of pulpitis in figure eights to jewelry work. And it requires experience and high qualifications of a doctor.
An inflamed nerve in a wisdom tooth can be treated by filling the canals. Provided that there is access to the root and the dental canals have good patency. It makes sense to preserve a tooth in the presence of an antagonist tooth, if the tooth is involved in the chewing process and is used when installing a prosthesis.
What to do if tooth pain persists
According to Dr. Bobkova, patients may experience pain when chewing after root canal filling. However, there is nothing wrong with this phenomenon if the unpleasant sensations disappear after two or three days.
“If the pain has been bothering you for a week or more, then you should consult your doctor. There can be several causes of pain - a fracture of the instrument, perforation in the tooth wall, removal of material beyond the apex of the tooth, or an additional canal was missed during the treatment process. Therefore, you cannot endure the pain; it is better to immediately contact your doctor.”