Ketorol is an effective pain reliever. The medicine belongs to the group of anti-inflammatory non-steroidal drugs. In addition to the analgesic effect, the drug reduces inflammation and swelling. In addition, ketorol, the instructions indicate this, has antipyretic properties.
Composition, forms and effects of the drug
The strong analgesic effect of the drug is provided by the main active substance - ketorolac tromethamine. Other components may vary depending on the manufacturer, so be sure to read the instructions.
The effect after taking the medicine is comparable to the effect of morphine. But at the same time, ketorol is a safer drug to use. The product can be used to combat different types of pain, the causes of which are any pathological conditions. It is used to eliminate symptoms and to treat specific diseases that are accompanied by swelling and fever.
The drug is produced in the form of:
- Tablets in a green soluble shell (with the amount of active substance - 10 mg).
- Transparent solution for intramuscular and intravenous administration (with an amount of active substance -30 mg/ml).
- Transparent, homogeneous gel (2%).
The most popular is the tablet form. After taking the drug, the active substance is completely absorbed into the gastrointestinal tract in the shortest possible time. Wherein:
- The maximum concentration in the blood is reached after an hour.
- Antipyretic and analgesic effects are observed after 30 minutes.
- Fatty foods slow down the absorption of the active substance.
Ketorol, 10 mg, film-coated tablets, 20 pcs.
The frequency of side effects is classified depending on the frequency of occurrence: often (1-10%), sometimes (0.1-1%), rarely (0.01-0.1%), very rarely (less than 0.01%) , including individual messages. From the digestive system: often (especially in elderly patients over 65 years of age with a history of erosive and ulcerative lesions of the gastrointestinal tract) - gastralgia, diarrhea; less often - stomatitis, flatulence, constipation, vomiting, feeling of fullness in the stomach; rarely - nausea, erosive and ulcerative lesions of the gastrointestinal tract (including with perforation and/or bleeding - abdominal pain, spasm or burning in the epigastric region, melena, vomiting like “coffee grounds”, nausea, heartburn and others), cholestatic jaundice, hepatitis, hepatomegaly, acute pancreatitis. From the urinary system: rarely - acute renal failure, lower back pain with or without hematuria and/or azotemia, hemolytic-uremic syndrome (hemolytic anemia, renal failure, thrombocytopenia, purpura), frequent urination, increased or decreased urine volume, nephritis, edema of renal origin. From the senses: rarely - hearing loss, ringing in the ears, visual impairment (including blurred visual perception). From the respiratory system: rarely - bronchospasm, shortness of breath, rhinitis, laryngeal edema. From the central nervous system: often – headache, dizziness, drowsiness; rarely - aseptic meningitis (fever, severe headache, convulsions, stiffness of the neck and/or back muscles), hyperactivity (mood changes, anxiety), hallucinations, depression, psychosis. From the cardiovascular system: less often - increased blood pressure; rarely – pulmonary edema, fainting. From the hematopoietic organs: rarely - anemia, eosinophilia, leukopenia. From the hemostasis system: rarely - bleeding from a postoperative wound, nosebleeds, rectal bleeding. From the skin: less often - skin rash (including maculopapular rash), purpura; rarely - exfoliative dermatitis (fever with or without chills, redness, thickening or flaking of the skin, swelling and/or tenderness of the tonsils), urticaria, Stevens-Johnson syndrome, Lyell's syndrome. Allergic reactions: rarely - anaphylaxis or anaphylactoid reactions (change in facial skin color, skin rash, urticaria, itching of the skin, tachypnea or dyspnea, swelling of the eyelids, periorbital edema, shortness of breath, difficulty breathing, heaviness in the chest, wheezing). Other: often - swelling (face, legs, ankles, fingers, feet, weight gain); less often – increased sweating; rarely - swelling of the tongue, fever.
Indications and contraindications for use
In order not to cause harm, it is important to know what ketorol helps with. Most often, ketorol, the instructions for use confirms this, is used as a symptomatic remedy to relieve headaches, dental and menstrual pain, as well as pain in the joints. In complex therapy, the drug is prescribed for the development of cancer and in the postoperative period.
The medicine is indicated to alleviate conditions in the following pathologies:
- Rheumatoid diseases.
- Spinal diseases and radiculitis.
- Ligament ruptures and muscle sprains.
Ketorol, like any non-steroidal drugs, is prohibited for use in the presence of diseases of the gastrointestinal tract. Otherwise, the risk of gastric bleeding increases. The drug is not prescribed to patients under 16 years of age or during pregnancy and lactation. You should stop using the medicine if you are hypersensitive to the components of the drug, as well as if you have the following pathologies:
- Bronchial asthma.
- Hyperkalemia.
- Heart failure.
- Liver and kidney diseases.
- Stroke.
There are other diseases for which the doctor recommends taking the drug with caution. These are chronic hypertension, diabetes mellitus, various nervous system disorders, etc.
Ketorol, for which a prescription is required, should not be taken with a number of other medications:
- Pentoxifylline.
- Acetylsalicylic acid.
- Anticoagulants.
- Lithium salts.
- Probenecid.
When taking the drug simultaneously with alcoholic beverages, the risks of intoxication of the body increase.
Ketorol®
The frequency of side effects is classified depending on the frequency of occurrence: often - (1-10%), sometimes (0.1-1%), rarely (0.01-0.1%), very rarely (less than 0.01% ), including individual messages.
From the digestive system: often (especially in elderly patients over 65 years of age with a history of erosive and ulcerative lesions of the gastrointestinal tract) - gastralgia, diarrhea; less often - stomatitis, flatulence, constipation, vomiting, feeling of fullness in the stomach; rarely - nausea, erosive and ulcerative lesions of the gastrointestinal tract (including with perforation and/or bleeding - abdominal pain, spasm or burning in the epigastric region, melena, vomiting like “coffee grounds”, nausea, heartburn and others), cholestatic jaundice, hepatitis, hepatomegaly, acute pancreatitis.
From the urinary system: rarely - acute renal failure, lower back pain with or without hematuria and/or azotemia, hemolytic-uremic syndrome (hemolytic anemia, renal failure, thrombocytopenia, purpura), frequent urination, increased or decreased urine volume, nephritis, edema of renal origin.
From the senses: rarely - hearing loss, ringing in the ears, visual impairment (including blurred visual perception).
From the respiratory system: rarely - bronchospasm, shortness of breath, rhinitis, laryngeal edema.
From the central nervous system: often - headache, dizziness, drowsiness, rarely - aseptic meningitis (fever, severe headache, convulsions, stiffness of the neck and/or back muscles), hyperactivity (mood changes, anxiety), hallucinations, depression, psychosis .
From the cardiovascular system: less often - increased blood pressure, rarely - pulmonary edema, fainting.
From the hematopoietic organs: rarely - anemia, eosinophilia, leukopenia.
From the hemostasis system: rarely - bleeding from a postoperative wound, nosebleeds, rectal bleeding.
From the skin: less often - skin rash (including maculopapular rash), purpura, rarely - exfoliative dermatitis (fever with or without chills, redness, thickening or peeling of the skin, swelling and/or tenderness of the tonsils), urticaria, Stevens syndrome - Johnson, Lyell's syndrome.
Allergic reactions: rarely - anaphylaxis or anaphylactoid reactions (change in facial skin color, skin rash, urticaria, itching of the skin, tachypnea or dyspnea, swelling of the eyelids, periorbital edema, shortness of breath, difficulty breathing, heaviness in the chest, wheezing).
Other: often - swelling (face, legs, ankles, fingers, feet, weight gain); less often - increased sweating, rarely - swelling of the tongue, fever.
Dosage and recommendations for treatment
In the postoperative period, tablets are usually prescribed, the price of which is affordable. This especially applies to cases where the instructions for use exclude ketorol injections against the background of certain consequences of operations. To relieve pain of any etiology, take one tablet. In case of intense severe pain, repeated use is allowed up to 4 times a day with a break of 4-6 hours. The duration of treatment is 5 days.
Ketorol tablets, the instructions for use emphasize this, should not be taken for any stomach problems. In this case, you need to purchase ketorol injection ampoules. In particular, intramuscular administration is indicated for persistent vomiting or difficulty swallowing. When they ask ketorol injections what they help with, experts often indicate radiculitis. In this case, the pain caused by this pathology can be dealt with quickly. Injections can be repeated with a break of 4 hours.
Ketorol gel is applied in a thin layer to clean and dried skin in areas of pain. Then rub in with soft massage movements. Procedures can be repeated 3-4 times a day until pain is relieved. The break between them is at least 4 hours. The duration of use of the gel is no more than 10 days.
Instructions for use KETOROL
Ketorol is intended for intramuscular injection; the drug should not be used for epidural or spinal administration. The solution is injected slowly IM (deep into the muscle). The onset of the analgesic effect is about 30 minutes with its maximum severity within 1-2 hours, the average duration of analgesia is 4-6 hours.
Administration of the drug several times a day for more than 2 days is not recommended, since in most cases patients do not require longer-term analgesic therapy, or can be switched to oral ketorolac. In this case, the duration of use of ketorolac parenterally and orally should not exceed 5 days in total.
To achieve maximum analgesic effect in the early postoperative period, it is possible to use ketorolac and narcotic analgesics together; the daily dose of the latter in this case is reduced. Ketorolac does not affect the addiction of copioids and does not increase the associated respiratory depression or sedation.
Dose selection and adjustment should be made in accordance with the intensity of pain and response to the drug. To minimize side effects, it is recommended to use the minimum effective dose for the shortest possible course of treatment.
Adults:
The usually recommended initial dose of Ketorol is 10-30 mg, followed by 10-30 mg every 4-6 hours. In the early postoperative period, it is permissible to administer the drug every 2 hours, if necessary. The maximum daily dose is 90 mg/day, in patients with body weight less than 50 kg - no more than 60 mg/day.
Elderly patients (over 65):
It is recommended to use the drug in a dose of 10-15 mg every 4-6 hours, the total dose should not exceed 60 mg/day. Due to the higher risk of side effects in this group of patients, the minimum possible duration of treatment and regular monitoring of the patient’s condition to exclude gastrointestinal bleeding are recommended.
Children:
The safety and effectiveness of ketorolac in children have not been confirmed; the drug is not recommended for use in children under 16 years of age.
Patients with impaired renal function:
the use of ketorolac is contraindicated in patients with severe and moderate renal impairment. In case of mild renal dysfunction, it is permissible to use Ketorol in a dose of no more than 60 mg/day.
If it is necessary to combine parenteral and oral administration of Ketorol, the total daily dose should not exceed 90 mg (60 mg in persons over 65 years of age, with a body weight of less than 50 kg or impaired renal function), while the dose of the drug taken orally should not exceed 40 mg/day . It is recommended to quickly transfer the patient only to the oral form of the drug.
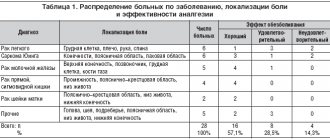
Ketorol for acute back pain
Effective treatment of this group of patients implies timely relief of pain syndrome (PS), elimination of obstacles to carrying out the full scope of rehabilitation measures, and adequate expansion of the motor regime. It has been established that the earliest possible expansion of the motor mode (walking on a flat surface, performing familiar daily activities both at home and outside) is an important factor associated with early relief of pain and a reduction in disability. There is evidence that long-term bed rest (immobilization for more than 7 days), excessive restrictive behavior (both intuitively chosen by the patient himself and recommended by the doctor) are most closely associated with a high risk of increasing the duration of exacerbation, transformation of acute pain into chronic, high probability of developing depressive disorders [3]. Based on these considerations, it seems necessary to orient the patient toward the earliest possible inclusion in the program of restorative and rehabilitation measures, to recommend the patient active behavior as part of the course of restorative treatment, to form positive motivation that ensures the mood to achieve convalescence and compensation for the existing neurological and orthopedic defect. The patient himself should strive for the earliest possible return to the usual level of daily physical activity as the syndrome is relieved. Along the way, it should be noted that factors that negatively affect the effectiveness of therapeutic measures and the timing of rehabilitation therapy are the patient’s incomplete understanding of the cause and essence of his disease, reluctance to take an active position in achieving recovery, the expectation of a significant therapeutic effect from passive therapeutic measures (massage, physiotherapy and etc.). An important condition that determines the possibility of carrying out rehabilitation measures is the early and most complete elimination of BS. There is an obvious connection between the effectiveness of pain therapy and the duration of restoration of adequate motor activity. To relieve pain syndrome (PS), the most widely used drugs are from the group of nonsteroidal anti-inflammatory drugs (NSAIDs). One of the effective NSAIDs used incl. for the treatment of patients with dorsalgia, is Ketorol (ketorolac) - a derivative of arylacetic acid. In clinical practice, it is used in the form of tromethamine salt, which ensures high solubility of the drug in water. In accordance with the results of modern experimental and clinical studies, ketorolac is an effective inhibitor of cyclooxygenase types 1 and 2, which regulates the synthesis of prostaglandins, prostacyclin and thromboxane A2 from arachidonic acid. Ketorolac is a racemic mixture of S(-) and R(+) enantiomers, with the analgesic effect due to the S-form. Without interacting with opioid receptors, ketorolac does not have a cardiodepressive effect, does not depress respiration, and does not cause paresis of intestinal smooth muscles. Of undoubted interest are the recently presented results of experimental studies indicating that ketorolac has the ability to reduce the activation activity of spinal cord glial cells that provide pain sensitivity, in particular by inhibiting the expression of protease-activated receptor-1 [4]. As the authors of the study established, it was precisely due to these properties of the drug that its use significantly reduced the severity of allodynia if ketorolac was administered one day after the injury. It should be noted that the ability of ketorolac to eliminate allodynia caused in the primary headache model was established in another study [5]. The drug is characterized by high bioavailability (80–100%) and quickly enters the vascular bed both after oral and parenteral administration, which ensures rapid onset of analgesia. In practical terms, it should be borne in mind that food rich in fat increases the time to reach the maximum concentration of the drug in the blood by 1 hour. It has been established that after oral administration in a dose of 10 mg of the drug, the analgesic effect develops within 10–60 minutes, and after intramuscular administration in dose of 30 mg – after 15–75 minutes. In clinical settings, it has been demonstrated that the duration of action of ketorolac reaches 10 hours. Up to 95% of the drug entering the body binds to plasma proteins, which ensures the stability of the concentration of ketorolac in the blood. Ketorolac is metabolized primarily in the liver to form conjugated and hydroxylated forms, which are excreted by the kidneys. Given that a significant portion of the drug is excreted in the urine, impaired renal function is associated with the risk of developing toxic effects. The half-life of ketorolac in elderly patients is slightly longer than in young patients (4.7–8.6 and 3.8–6.3 hours, respectively). As noted above, ketorolac is well tolerated and has a low incidence of side effects (about 3%). The most common of these are dyspeptic disorders. Limiting the duration of treatment to achieve a positive effect can be a reliable way to increase the safety of therapy [6]. Currently, ketorolac is widely used in a number of countries to relieve acute BS caused by various pathological conditions, in particular to eliminate postoperative pain. A number of clinical studies have established the high analgesic effectiveness of the drug. The pronounced analgesic effect of ketorolac has attracted the attention of anesthesiologists and specialists faced with the need to relieve acute pain in somatic diseases and after surgical interventions. Thus, in one of the open pilot studies [7], intramuscular administration of ketorolac to 22 patients with severe postoperative PS provided an acceptable level of pain relief, and in 13 cases complete relief of pain was achieved. In 95% of patients, a decrease in pain intensity was observed during the first 60 minutes. after administration of the drug and increased over 2–4 hours, leading to complete elimination of pain in 50% of patients after 3.7 hours. The authors concluded that during the first hour after using ketorolac, additional administration of analgesic drugs is not advisable, given the high probability of delayed onset analgesic effect. An important property of ketorolac, in addition to pain relief, is its anti-inflammatory effect. It turned out that ketorolac administered into a postoperative wound in relatively small doses has an effect comparable to that after systemic use of NSAIDs, although the number of side effects turned out to be incomparably smaller [8]. This local use of the drug ensured a significant reduction in the need for patients to take opioid analgesics. According to the authors of the study, the effectiveness of the drug was due to the local anti-inflammatory effect, as evidenced by a decrease in the content of proinflammatory cytokines in the wound exudate. Similar data were obtained from another in vitro study. It turned out that ketorolac, introduced into cell culture, caused inhibition of the production of a number of proinflammatory cytokines and cell adhesion molecules, despite the fact that the effect was less pronounced than that of corticosteroids, it was significantly superior to that of placebo [9]. According to the authors, ketorolac has the ability to inhibit the cellular component of inflammation, which can find its practical application in the clinic. Somewhat later, a whole series of randomized, usually placebo-controlled, studies were conducted to evaluate the effectiveness of ketorolac in relieving acute BS caused by various pathological conditions. The objective of these works was to compare the effectiveness of ketorolac and representatives of other groups of analgesic drugs, in particular opioids and NSAIDs. In patients with BS caused by extensive surgery, intravenous administration of 30 mg of ketorolac in its analgesic activity was comparable to the administration of 4 mg of morphine [10]. Similarly, ketorolac was found to have comparable analgesic effects to another opioid derivative, meperidine (50 mg), when used in patients with acute hepatic colic, and the need for repeat analgesia was less likely to occur after ketorolac use [11]. The results of this work were confirmed somewhat later in a similar double-blind randomized study that included 324 patients with hepatic colic [12]. It turned out that 2 hours after the administration of ketorolac, the weakening of BS on the visual analogue scale (VAS) was 6.2±3.6 cm, and after the administration of meperidine – 6.7±3.6 cm (the differences were not significant; p=0 ,25). The authors noted better tolerability of ketorolac, as evidenced by a smaller number of patients who reported nausea, vomiting, and a feeling of general weakness. Another multicenter, double-blind study, including 125 patients undergoing arthroscopic autoplasty of the anterior cruciate ligament of the knee joint, compared the effectiveness of ketorolac (20 mg orally once) and a combination of 10 mg hydrocodone and 1000 mg paracetamol [13]. The effectiveness of ketorolac 1, 2 and 3 hours after administration was significantly higher, which allowed the authors to recommend the drug to eliminate BS in the postoperative period. Considering the analgesic effect and tolerability of ketorolac in comparison with opioids, it should be noted that there is experience in using the drug in pediatric practice: in children from 6 to 18 years old who have undergone orthopedic or arthrological surgery on large bones [14]. The results of an open study showed that the use of ketorolac (1.0 mg/kg parenterally as a loading dose, subsequently 0.5 mg/kg every 6 hours throughout the day) eliminates pain and significantly reduces the need for additional painkillers. Of interest are the results of a comparative study of the effectiveness of subacromial administration of triamcinolone or ketorolac for the purpose of relieving local BS [15]. Ketorolac has demonstrated its undoubted advantage as an analgesic agent with better tolerability. In a randomized, double-blind study that included 102 children, a single dose of ketorolac was not inferior to morphine in its analgesic effect [16]. It should be noted that in Russia the drug is approved for medical use in patients at least 16 years of age. Almost all researchers who studied the analgesic effectiveness of ketorolac noted its good tolerability. The undoubted advantage of ketorolac compared to narcotic painkillers is the absence of an inhibitory effect on respiratory function and the cardiovascular system, as well as the absence of sedation. It is important to note that there is no risk of addiction. It is also necessary to mention the absence of gastrotoxicity during short courses of treatment with ketorolac in order to eliminate acute BS. Considering the effectiveness of ketorolac in relieving postoperative pain, attempts have been made to use it in patients with acute pain caused by degenerative lesions of the articular-ligamentous apparatus. A randomized, double-blind study compared the effectiveness of intramuscular meperidine (1 mg/kg) and ketorolac (60 mg) for the relief of acute musculoskeletal pain in the low back in 155 patients over the age of 18 years [17]. The analgesic effect of the drugs according to VAS was comparable: a 30% decrease in pain intensity was recorded in 63% of patients receiving ketorolac and 67% of patients in the meperidine group; 35% of patients who received ketorolac and 37% who received meperidine required additional painkillers. The authors note that, with a comparable analgesic effect, treatment tolerability was significantly better in patients receiving ketorolac; they experienced significantly less unwanted side effects (nausea, repeated vomiting, drowsiness). A large-scale study was conducted in Moscow to study the effectiveness of ketorolac in patients with acute BS caused by inflammatory diseases of the musculoskeletal system, degenerative diseases of the spine (arthralgia, lumbago, ischalgia) and some other pathological conditions [18]. The study was conducted in the setting of prehospital medical care in an outpatient setting. A total of 1011 patients (mean age 54.1±0.46 years) who received ketorolac (30 mg intramuscularly) or other analgesic drugs, in particular metamizole sodium (2 ml of 50% solution intramuscularly) took part in the study. According to the results of assessing the dynamics of pain using VAS, the analgesic effect of ketorolac is 1.3 times greater than that of metamizole sodium. It is significant that the need to repeatedly seek medical help (call an ambulance team) for musculoskeletal pain was 3 times higher in patients who received metamizole (18% versus 6.2%). The onset of the analgesic effect after the administration of ketorolac was observed after an average of 12.4±0.33 minutes, whereas after the use of metamizole - after 26.9±0.47 minutes. (the difference was significant), and the severity and speed of onset of the effect did not significantly depend on the age of the patients. The data obtained allowed the authors to conclude that the use of ketorolac in the prehospital stage of treatment of acute BS of various etiologies is effective and clinically justified in various pathological conditions, in particular in acute musculoskeletal pain. It should be noted that, according to the results of the cited study, the use of ketorolac has certain pharmacoeconomic advantages: the value of such a parameter as the cost per unit of effectiveness turned out to be 3 times less than with the use of metamizole (the differences were significant), and significantly lower than with use of other NSAIDs. Almost simultaneously, an open, uncontrolled clinical trial was conducted, the purpose of which was to evaluate the effectiveness and safety of the use of parenteral and oral forms of ketorolac (Ketorol) in relieving moderate and severe back pain (at least 940 mm on VAS) [18]. The study included 30 patients aged 30–65 years (average age: 49.4 years, 17 men) with degenerative lesions of the lumbar spine. Diagnoses were verified based on the results of clinical and radiological studies. The duration of treatment for patients did not exceed 5 days. At the beginning of therapy, ketorolac was prescribed as intramuscular injections of 60 mg/day. (30 mg 2 times/day) for 2 days, and then in tablet form 20 mg/day. During the study period, the use of other NSAIDs was excluded. During the study, it was found that as a result of a 5-day course of using ketorolac, the intensity of BS according to VAS significantly decreased, and after parenteral administration of the first dose of the drug it decreased from 65.4 to 22.1 mm (p < 0.05). At the same time, the volume of active movements in the lumbar spine increased, which was reflected in the results of the Thomaier tests (increase in the range of movements by 33% from the initial indicators) and Schober (increase by 25%). Based on the data obtained, the authors concluded that ketorolac is highly effective and well tolerated. It seems important that when assessing the safety of the drug, only 16% of patients had side effects (gastralgia, feeling of fullness in the stomach, headache accompanied by a rise in blood pressure). These side effects were not severe and did not require discontinuation of the drug or change in its dosage regimen. Over the past years, significant experience has been accumulated in the use of ketorolac not only in patients with musculoskeletal pain syndromes, but also in other pathological conditions in neurology associated with intense pain. Of undoubted interest is the possibility of using the drug to relieve an acute attack of migraine. The results of meta -analysis of 8 randomized clinical studies (321 patients are included, of which 141 received ketorol parenterally), selected from 32 dedicated to the possibility of its use in migraine attack, showed that the drug is able to effectively stop the hemicacular attack [20]. It turned out that, by the ability to eliminate the attack of Ketorolak pain, he exceeded the constituent, introduced by orally, while its use was not associated with the risk of dependence, which could be observed when using some opioids, in particular meteridine. Thus, the results of numerous studies indicate that ketorolac (ketorol) is an effective and safe drug for the treatment of acute pain in the lower back. The use of Ketorolak (ketorol) in such patients in its effectiveness not only surpasses many NSAIDs, but is not inferior to weak opioids. Subject to the reception regimen, the drug is well tolerated by patients and does not cause serious side effects. Literature 1. Carey T., Evans A., Hadler N. et al. Acute Severe Low Back Pain. APPULATION-BASED Study of Prevalence and Care-seeking // Spine. 1996. Vol. 21. P. 339–344. 2. Luo X., Pietrobon R., Sun S. et al. Estimates and Patterns of Direct Health Care Expenditures Among Individuals with Back Pain in the United States // Spine. 2004. Vol. 29. P. 79–86. 3. Bair M., Robinson R., Katon W. et al. Depression and Pain Comorbidity: A Literature Review // Arch. Intern. Med. 2003. Vol. 163. P. 2433–2445. 4. Dong L., Smith J., Winkelstein B. Ketorolac Reduces Spinal Astrocytic Activation and Par1 Express Associated with AttenUtion of Pain Following Following Joint Injury // J. NeUROTRAMA. 2012. 5. Oshinsky M., Sangvi M., Maxwell C. et al. Spontaneous Trigeminal Allodynia in Rats: A Model of Primary Headache // Headache. 2012. Vol. 52 (9). P. 1336–1349. 6. BJarnason I. GastroinTestinal Safety of Nsaids and Over-the-Counter Anaalgesics // Int. J. Clin. Pract. Suppl. 2013. Vol. 178. P. 37–42. 7. Perez-Urizar J., Granados-Soto V., Castaneda-Hernandez G. et al. Anaalgesic Efficacy and Bioavailability of Ketorolac in Postoperation Pain: A Probability Analysis // Arch. Med. Res. 2000. Vol. 31 (2). P. 191–196. 8. Carvalho B., Lemmens H., Ting V., Angst M. Postoperation Subcutaneous Instillation of Low-Dose Ketorolac But Hydromorphone Reduces Wound Concentrations of Intereleum 6 and InterleUKIN-10 and IMPROVES ANALGESI Following Cesarean Delivery // J. Pain. 2013. Vol. 1. P. 48–56. 9. Mazzocca A., McCarthy M., Intravia J. et al. An in vitro evaluation of the anti-inflamMatory Effects of Platelet-Rich Plasma, Ketorolac, and Methylprednisolone // Arthroscopy. 2013. PII: S0749–8063 (12) 01896–8. DOI: 10.1016/J.Arthro 2012.12.005. 10. Brown C., Moodie J., Wild V. et al. Comparison of Intravenous Ketorolac Tromethamine and Morphine Sulfate in the Treatment of Postoperation Pain // PharmacoPyrapy. 1990. Vol.10 (6 (PT 2)). 116S --121S. 11. Dula D., Anderson R., Wood G. A Prospective Study Comparing Im Ketorolac with Im Meperidine in the Treatment of Acute Biliary Colic // J. Emerg. Med. 2001. Vol. 20 (2). P. 121–124. 12. Henderson S., Swadron S., Newton E. Comparison of Intravenous Ketorolac and Meperidine in the Treatment of Biliary Colic // J. Emerg. Med. 2002. Vol. 23 (3). P. 237–241. 13. Barber F., Gladu D. Comparison of Oral Ketorolac and Hydrocodone for Pain Relief After Anterior Cruciate Reconstruction // Arthroscopy. 1998. Vol. 14 (6). P. 605–612. 14. EBERSON C., Pacicca D., Ehrlich M. The Role of Ketorolac in Decreasing Length of Stay and Narcetic Complications in the Postepection Pediatric Orthopaedic Patient // J. Pedicatr. Orthop. 1999. Vol. 19 (5). P. 688–692. 15. Min K., Pierre P., Ryan P. et al. Elbow. Surg. 2012. PII: S1058–2746 (12) 00372–2. Doi: 10.1016/J.JSE. 2012.08.026. . 16. Lieh-lai M., Kauffman R., Uy H. et al. A RANDOMIZED Comparison of Ketorolac Tromethamine and Morphine for Postoperation Anaalgesia in Critically Ill Children // Crit. Care Med. 1999. Vol. 27 (12). P. 2786–2791. 17. Veenema K., Leahey N., Schneider S. Ketorolac Versus Meperidine: Ed Treatment of Severe Musculoskeletal Low Back Pain // Am. J. Emerg. Med. 2000. Vol. 18 (4). P. 40404–40407. 18. Vertkin A.L., Prokhorovich E.A., Goruleva E.A. and others. The effectiveness and safety of the use of ketorol to stop the pain syndrome at the prehospital stage // Emergency therapy. 2004. No. 1-2; 16–17: 12–17. 19. Shostak N.A., Pravyuk N.G., Aksenova A.V. and other possibilities of optimizing analgesic and anti -inflammatory therapy in patients with acute pain in the back // breast cancer. 2006. No. 14; 8. S. 610–615. 20. Taggart E., Dran S., Kokotillo A. et al. Ketorolac in the Treatment of Acute Migraine: A Systematic Review // Headache. 2013. Vol. 53(2). P. 277–287.