We are publishing an article by Natalya Lvovna Mayorova, a dentist, therapist, and head of the therapeutic department of the Dentalika clinic.
Pain relievers used in modern dental practice can work wonders. After receiving an anesthetic injection, the patient does not feel any pain or even particularly unpleasant sensations. To ensure that the injection itself is painless, before the procedure the doctor “freezes” the injection site with a special preparation with a delicious smell of cherry, lemon, or apple.
Local anesthesia is the main method of pain relief used in dental practice. With local anesthesia, the patient remains fully conscious, and this allows the doctor to fully control the entire course of treatment, communicate with the patient, and monitor your reaction.
The quality of dental interventions depends on the results the doctor obtained during local anesthesia. Therefore, achieving 100% pain relief is necessary not only for the patient, but also for the doctor, in order to carry out treatment calmly, slowly, and efficiently. Hence the following requirements for local anesthetics:
- they must have a strong analgesic effect, easily penetrate into tissues and remain there for as long as possible;
- have low toxicity, causing a minimum number of both general and local complications
Based on these wishes, we chose several widely used drugs:
- Ultracaine DS forte (4% articaine, adrenaline 1:100,000);
- Ultracaine DS (4% articaine, adrenaline 1:200,000);
- Scandonest SVC (3% mepivacaine; without vasoconstrictors - adrenaline).
Now in more detail about their action.
Ultracain DS
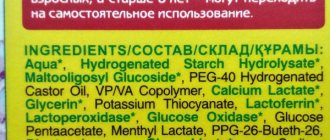
The analgesic basis of the first two drugs is ARTICAINE (amide anesthetic from the thiophene series), an antispasmodic - lowers blood pressure. It is characterized by rapid action - anesthesia occurs in 0.5-3 minutes. Articaine is 2 times stronger than lidocaine and 6 times stronger than novocaine (anesthetics of previous generations), less toxic, relatively quickly eliminated from the body. Its half-life is, on average, 22 minutes, that is, all traces of the drug disintegrate in 44 minutes and are then completely eliminated from the body. Has high penetrating ability. It is distinguished by high purity of the solution. Allergic reactions to articaine are very rare - one in one hundred thousand injections ; the use of articaine, according to studies, is safe in 99.4% of cases. They also contain a vasoconstrictor (a substance that causes constriction of blood vessels and a decrease in blood flow in them) - adrenaline. The use of a vasoconstrictor continues and enhances anesthesia. The drug also contains antioxidants (sulfites) - substances that prevent the oxidation of adrenaline.
Ultracaine does NOT contain parabens (anesthetic preservatives), which significantly reduces its toxicity. In addition, parabens can cause allergic reactions.
Thus, ultracaine is:
- a strong anesthetic with moderately low toxicity, due to its components;
- the safest drug for pregnant women, because articaine does not penetrate the hematoplacental barrier - the barrier separating the blood of the fetus and the blood of the mother (Ultracaine DS).
School-age children can also use Ultracain DS. We always remember that the administration of an anesthetic solution with adrenaline is CONTRAINDICATED for children under 5 years of age, patients with pathologies of the cardiovascular system, with endocrine pathologies, taking antidepressants, thyroid hormones, drugs that block beta adrenergic receptors; - an anesthetic that practically does not require postoperative pain relief;
- a drug that provides a rapid onset of anesthesia, depending on the anesthesia tactics chosen by the doctor, the effect occurs within 30 seconds to 3-5 minutes);
The duration of anesthesia is, depending on the technique chosen by the doctor, from 1.5-2 hours to 5-6 hours. The choice of different techniques (infiltration, conduction anesthesia) depends on the planned dental procedure. For example, there is a difference between the treatment of caries of one tooth and the complex removal of a wisdom tooth. - good local and general tolerability. According to studies, only 4.3% of patients experienced toxic reactions, which was caused by the presence of adrenaline and sodium disulfate in the anesthetic solution.
- For standard procedures, a small amount of anesthetic is required (0.9 ml-1.8 ml).
I would like to note that for standard dental operations it is better to use Ultracain DS (adrenaline 1:200,000). A strong anesthetic provides high-quality anesthesia even during complex, long-term interventions, and a small amount of vasoconstrictor ensures low toxicity of the anesthetic solution. And we prefer to consider Ultracaine DS forte (adrenaline 1:100,000) as a “reserve anesthetic” in more complex situations:
- anesthesia of the lower lateral teeth (molars) for their treatment and depulpation;
- pain relief for inflammatory processes in the maxillofacial area (periostitis, osteomyelitis);
- for particularly traumatic interventions;
- in patients with a low pain threshold.
Lidocaine
The toxicity of lidocaine increases when it is used simultaneously with cimetidine and propranolol due to an increase in the concentration of lidocaine; this requires a reduction in the dose of lidocaine. Both drugs reduce hepatic blood flow. In addition, cimetidine inhibits the microsomal activity of liver enzymes.
Ranitidine, Diltiazem, verapamil, propranolol and other β-blockers reduce the clearance of lidocaine, which leads to an increase in its concentration in the blood plasma.
Antiviral agents (eg, amprenavir, atazanavir, darunavir, lopinavir) can also cause increased serum concentrations of lidocaine.
Hypokalemia caused by diuretics may reduce the effect of lidocaine when used simultaneously (see section "Special Instructions"). Lidocaine should be used with caution in patients receiving other local anesthetics or agents structurally similar to amide-type local anesthetics (eg, antiarrhythmic agents such as mexiletine, tocainide) because systemic toxic effects are additive.
When lidocaine is used in combination with narcotic analgesics, hexenal or sodium thiopental, the inhibitory effect on the central nervous system and respiration may be enhanced.
Separate drug interaction studies have not been conducted between lidocaine and class III antiarrhythmic drugs (eg, amiodarone), but caution is recommended when using them together.
In patients concomitantly receiving antipsychotics that prolong or have the potential to prolong the QT interval (e.g., pimozide, sertindole, olanzapine, quetiapine, zotepine), prenylamine, epinephrine (with occasional intravenous administration), or 5-HT3-serotonin receptor antagonists (e.g., tropisetron, dolasetron), the risk of developing ventricular arrhythmias may increase.
Concomitant use of quinupristin/dalfopristin may increase lidocaine concentrations and thus increase the risk of developing ventricular arrhythmias; their simultaneous use should be avoided.
Patients receiving muscle relaxants (eg, suxamethonium) may have an increased risk of enhanced and prolonged neuromuscular blockade.
Cardiovascular insufficiency has been reported following the use of bupivacaine in patients receiving verapamil and timolol; lidocaine is similar in structure to bupivacaine.
Dopamine and 5-hydroxytryptamine lower the seizure threshold in patients receiving lidocaine.
Opioids appear to have anticonvulsant effects, supported by evidence that lidocaine lowers the seizure threshold to fentanyl in humans.
Combinations of opioids and antiemetics, sometimes used for sedation in children, may lower the seizure threshold to lidocaine and increase its CNS depressant effects.
The use of epinephrine with lidocaine may reduce systemic absorption, but with accidental intravenous administration the risk of ventricular tachycardia and ventricular fibrillation increases sharply.
Concomitant use of other antiarrhythmic drugs, beta-blockers and slow calcium channel blockers may further reduce AV conduction, ventricular conduction and myocardial contractility.
The simultaneous use of vasoconstrictors increases the duration of action of lidocaine.
Concomitant use of lidocaine and ergot alkaloids (eg, ergotamine) can cause severe hypotension.
Caution must be exercised when using sedatives as they may interfere with the action of local anesthetics on the central nervous system. Caution should be exercised when using antiepileptic drugs (phenytoin), barbiturates and other inhibitors of liver microsomal enzymes, as this may lead to decreased effectiveness and, as a result, an increased need for lidocaine. On the other hand, intravenous administration of phenytoin may enhance the depressant effect of lidocaine on the heart.
The analgesic effect of local anesthetics can be enhanced by opioids and clonidine.
The combined use of lidocaine with procainamide can cause central nervous system stimulation and hallucinations.
When using lidocaine and polymyxin-B simultaneously, it is necessary to monitor the patient's respiratory function. Ethyl alcohol, especially with prolonged abuse, can reduce the effect of local anesthetics. Lidocaine is not compatible with amphotericin B, methohexitone, nitroglycerin.
With the simultaneous use of lidocaine with narcotic analgesics, an additive effect develops, which is used during epidural anesthesia, but increases the depression of the central nervous system and respiration.
Vasoconstrictors (epinephrine, methoxamine, phenylephrine) prolong the local anesthetic effect of lidocaine and can cause increased blood pressure and tachycardia.
Use with monoamine oxidase inhibitors (furazolidone, procarbazine, selegipine) probably enhances the local anesthetic effect of lidocaine and increases the risk of lowering blood pressure. Guanadrel, guanethidine, mecamylamine, grimstaphane camsylate increase the risk of a pronounced decrease in blood pressure and bradycardia. Anticoagulants (including ardeparin sodium, dalteparin sodium, danaparoid sodium, enoxaparin sodium, heparin, warfarin, etc.), nonsteroidal anti-inflammatory drugs (NSAIDs) or plasma expanders increase the risk of bleeding.
Lidocaine reduces the cardiotonic effect of digitoxin.
Lidocaine reduces the effect of antimyasthenic drugs (prozerin, oxazil, etc.), enhances and prolongs the effect of muscle relaxant drugs.
When treating the injection site with disinfectant solutions containing heavy metals, the risk of developing a local reaction in the form of pain and swelling increases.
Mixing lidocaine with other medications is not recommended.
Scandonest SVC
If the patient belongs to a risk group (with severe concomitant diseases , in particular cardiovascular pathology ), the use of an anesthetic solution with adrenaline, a vasoconstrictor, should be completely abandoned. In such cases we use Scandonest SVC . This anesthetic exhibits a vasoconstrictor effect, i.e. has vasoconstrictor properties and can therefore be used without adrenaline, which means that the drug does not contain sulfites and can also be used in patients with bronchial asthma and allergic conditions (after an allergy test). Scandonest SVC is a medium-strength anesthetic; provides anesthesia, depending on which part of the jaw the doctor disconnects from pain sensitivity, for 20 - 90 minutes, which sets it apart from the group of other non-adrenaline anesthetics.
Advantages of carpule pain relief
The most important advantages of carpulal anesthesia can be considered:
- The exact amount of the drug in 1 ampoule is exactly 1.7 ml. Thanks to this, the doctor can count the carpules and know exactly the dosage of the administered drug.
- Complete sterility. Carpules are manufactured and sealed in a warehouse under completely sterile conditions. This way you can be sure of the quality of the injected drug.
- Less pain from the injection itself. Patients feel less pain when punctured because the needle of a carpule syringe is much thinner and more flexible than that of a regular syringe.
- It is more convenient for the doctor to control the process. The dental anesthesia carpule syringe fits very comfortably in the hand thanks to special handles and stops. Also due to the greater flexibility of the needle, it can be bent in almost any direction without fear of it breaking off.
- Elimination of errors. When using Carpules, the possibility that the doctor will administer the wrong drug or in the wrong quantity or concentration is completely eliminated. After all, with carpule anesthesia, the doctor always knows exactly what he is injecting - the name of the drug, its concentration and quantity is written on each carpule.
Allergy tests
If you have previously experienced allergic reactions to medications, you have doubts, and you do not fully know which local anesthetics are safe for you, we strongly recommend that you undergo tests for allergic reactions at an allergy center before visiting the dentist. The addresses of such centers can be obtained from the reception of the Dentalika dental clinic. The test results can be completely trusted. This recommendation especially applies to parents of children who bring their children to the dentist for the first time. Unfortunately, from year to year the number of children susceptible to allergic reactions in our city is only growing. A visit to the allergy center will completely protect your child from possible complications.
General overview
The name of the technique - carpule anesthesia - comes from the special design of the syringe, with the help of which a composition is introduced into the tissues that reduces the sensitivity of the tissues. The capsule with the drug is called a “carpule” and is replaceable, which allows the device to be used repeatedly for dental procedures. For the manufacture of medical instruments, a metal alloy is used, which is safe for biological tissues of the body. The system consists of a frame and piston part, as well as a needle, while the piston is not completely removed from the body, and in the side there is a slot for placing a capsule with the drug.
An ampoule with an anesthetic, hermetically sealed along the seam, has a rubber plug on one side and a metal valve on the other. The algorithm for using a carpule syringe involves placing the capsule in the gap, followed by screwing in the needle and performing the injection. The plug is located on the opposite part - as you press the piston, the composition moves into the fabric structure, providing the desired result.
Children
It should be noted separately the features of local anesthesia in children. The technique of local anesthesia in children must be planned so that 100% pain relief is achieved at all stages of treatment, otherwise it will be impossible to carry out the necessary manipulations.
As mentioned above, children under 5 years of age are given an anesthetic without adrenaline (3% scandonest SVC, or septanest 4% SVC).
Children over 5 years old can use an anesthetic with low concentration adrenaline (1:200,000 - Ultracaine DS). The dose of drugs is selected depending on age. Pain relief is performed in children in 3 stages:
- First, a superficial anesthetic gel is applied
- then a small dose (0.1-0.2 ml) of anesthetic is administered;
- after which, after 60-90 seconds (time sufficient for effective anesthesia of the needle path in the soft tissues), the remaining amount of the planned dose of anesthetic is administered.
We wait 5-10 minutes until complete anesthesia occurs. The child, feeling a complete absence of pain, gains confidence in the doctor and gives the opportunity to carry out the necessary intervention.
Lidocaine during pregnancy and lactation -
Lidocaine cannot be used as a local anesthetic during pregnancy. However, lidocaine spray can be used, because in the doses used, it does not pose a danger to the fetus. During lactation, the drug should not be prescribed either in the form of a spray or for local anesthesia.
The safest drug for pregnant and lactating women is Ultracaine “DS” (instructions for the drug).
Lidocaine: contraindications for use
- allergy to lidocaine components,
- significant impairment of liver function,
- sick sinus syndrome,
- 2-3 degree atrioventricular block,
- severe bradycardia,
- myasthenia gravis, cardiogenic shock.
Sources:
1. Higher prof. the author's education in surgical dentistry, 2. Based on personal experience as a dental surgeon, 3. National Library of Medicine (USA), 4. “Local anesthesia in dentistry” (Baart J.), 5. “Propaedeutics of surgical dentistry” (Soloviev M.).
Failed anesthesia
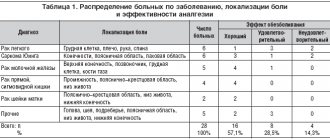
I would also like to touch upon the topic of unsuccessful local anesthesia. Almost every dentist has encountered this in their practice. The reasons for this phenomenon can be classified into 2 groups:
- depending on the doctor (poor choice of anesthesia technique and anesthetic solution; errors in the technique);
- depending on the anatomical and psychological characteristics of the patient.
To eliminate psychological causes in patients with a labile psyche (with increased emotionality, sensitivity, excitability), premedication is used: sedatives and sedatives.
In all other cases, the doctor must approach the choice of anesthetic and local anesthesia technique with even greater responsibility and professionalism, starting from the very first minutes of communication with the patient (history collection).
You should always remember that there are NO teeth that cannot be anesthetized, it’s just sometimes more difficult to achieve this.
High-quality pain relief minimizes patient discomfort and allows dentists to perform the necessary interventions.
Natalya Lvovna Mayorova doctor - therapist - dentist October 2009
Dear Colleagues! When copying information, placing a link to the source site is mandatory.
general description
Anesthesia is administered using a special syringe, after which the sensitivity of the nerve endings of the tooth is reduced. The capsule is called carpool. The procedure for administering the medicine itself follows a standard procedure.
The carpule syringe is designed for reusable use. It is made of medical metal, and the structure includes a frame, a piston part and a needle. The piston is equipped with a gap to accommodate the capsule. The latter is a special ampoule containing an anesthetic.
The ampoule is sealed in a sealed package, which ensures the safety of properties and compliance with sanitary standards.