Content:
- A tooth has been removed: can you or can’t smoke?
- Why smoking after removal is undesirable
- Is it possible to smoke after tooth extraction if there are stitches on the gums?
- Smoking and anesthesia are an undesirable combination
- Useful information about the effect of nicotine on the mucous membranes of the oral cavity
- How to speed up the healing of a hole
A person who has just had a tooth removed is usually nervous. This is understandable - he has suffered stress and wants to relax. Smokers often use cigarettes to calm down, but the question arises: when can you smoke after dental surgery? We suggest you look into it.
Apply cold to prevent swelling -
What to do after tooth extraction to prevent the development of swelling... As soon as you come home, your first actions are to take ice or a piece of frozen meat from the freezer, wrap it in a towel and apply it to your cheek in the projection of the extracted tooth (24stoma.ru). This is necessary to avoid or reduce possible swelling of the soft tissues of the face that may develop (especially if the removal was difficult).
It is necessary to hold the ice 3-4 times for 5 minutes, with an interval of 5-10 minutes between each approach. It makes sense to keep ice only in the first hours after removal, then it is useless. But heating and applying heat is strictly forbidden, because... In this case, suppuration is guaranteed.
Important: if you want to avoid the development of swelling of the soft tissues of the face as much as possible, then in addition to using cold, be sure to take antihistamines (anti-allergic) medications in the first 2-3 days after removal. This group of drugs also has a good anti-edematous effect. Suprastin is especially suitable: 1 tablet per day before bed (for 2-3 days).
A tooth has been removed: can you or can’t smoke?
Dental surgeons prohibit smoking during the first two to three hours after extraction. This short period is relevant if:
- the operation was not very complicated;
- the bleeding has stopped completely;
- after removing the gauze swab, blood did not begin to flow again;
- a dense blood clot has managed to form, isolating the wound in the gum.
In severe cases, smoking after tooth extraction will have to be postponed for several days - the exact time period will be determined by the doctor. This is due to the fact that nicotine contained in cigarette smoke irritates the edges of the inflamed hole and causes spasm of blood vessels. Because of this, regeneration processes slow down and dangerous complications can develop.
Treatment of local complications after tooth extraction
The choice of treatment method is based on the causes of the pathology, its nature and the patient’s condition. Age is also taken into account, since not all medications are suitable for children. Therefore, the treatment regimen is developed individually for each patient.
Complications related to bone structures
Most often, a fracture of the tooth root occurs during extraction. In this case, it is usually removed so as not to provoke an inflammatory process. If symptoms of infection have already arisen, and the pathology is discovered a few days after the operation, wait 1-1.5 weeks and perform surgical treatment again. In this case, the patient takes anti-inflammatory drugs to stop the inflammation process.
If during extraction a tooth that was located next to the extracted one is fractured, the doctor evaluates how reasonable and possible it is to save it. With minor damage, it is possible to build up the damaged area. If the fracture is serious, the tooth is removed.
During surgery, cases of dislocation of the tooth closest to the extracted one are not uncommon. For high-grade injuries, replantation is indicated. If the mobility of the tooth is preserved, it is strengthened with a stabilizer in the form of an endodontoendoxal implant. If the tooth tissue is completely dead, it is removed and replaced with an artificial tooth. If the dislocation is incomplete, strengthening is carried out using a splint.
A situation where the root is pushed into the jaw tissue from below is possible when the third molar of a large tooth is removed. If the hard part is palpable, it is removed through an incision made over it. If there are no objective signs of a root being located in any part of the jaw, an x-ray is taken, which is performed in two projections (side and front) - this is how the desired root is detected and removed.
When removed, the root of a tooth may end up in the sinus of the upper jaw. In this case, the root is urgently removed, as it can cause infectious sinusitis. The operation is not performed through the hole so as not to enlarge the hole in the sinus. First, perforation of the bottom is carried out, then an operation to remove the root is made - for this, a burr hole is made in the sinus of the upper jaw from the outside and in front. The operation is performed using endoscopic devices under continuous monitoring.
Trauma to the alveolar process is not considered a serious complication during tooth extraction. This condition does not cause discomfort and is not considered dangerous. It goes away on its own without affecting recovery after surgery. If the fragment has sharp edges, they are smoothed even during tooth extraction. The most commonly injured teeth are the upper and lower third molars.
Pathologies of soft tissues during tooth extraction
In case of injury to soft tissues or gums, the primary task is to stop bleeding: a hemostatic sponge is applied to the wound, and in case of severe damage, the wound is sutured with excision of those areas whose integrity cannot be restored.
Some patients are concerned about swelling localized on the gum near the extracted tooth. In the first few days after surgery, it is considered physiological. But if the pain persists and the swelling grows, you need to consult a doctor - a purulent complication may develop, which requires opening and draining the resulting cavity.
If a blood clot does not form at the site of the extracted tooth, alveolitis appears. It is provoked by non-compliance with the doctor’s recommendations for oral care (smoking, rinsing in the first few days, failure to perform hygiene procedures, aggressive foods). Sometimes the patient is bothered by pain that is subjectively felt in the temple area. Before starting treatment, the hole is sanitized, treated with an antiseptic solution and a cotton swab with an anti-inflammatory agent is placed in it.
If the rules of asepsis and antisepsis are not followed, osteomyelitis and other purulent complications may occur after tooth extraction. If left untreated, the pathology spreads to neighboring organs and also affects the jaw. To get rid of this condition, the patient undergoes an autopsy of the infectious focus and is prescribed anti-inflammatory drugs.
Other damage after tooth extraction
In some cases, paresthesia occurs due to tooth extraction. It is characterized by a lack of sensation in the cheeks, lips, chin and tongue. The condition lasts about two weeks, then passes. You can speed up recovery by taking B vitamins, ascorbic acid, dibazole and galantamine.
If the patient opens his mouth excessively, the jaw may dislocate. This complication is typical for elderly patients, as well as during surgery on large and small molars of the lower row. When a dislocation usually affects one side, less often both. Patients have this defect corrected on the spot, immediately after detection.
In rare cases, a jaw fracture is detected. It is typical for surgery on the second or third molar. Diagnosis of a fracture is complicated by blurred symptoms, but is clearly visible on x-rays, so x-rays are often used to monitor the success of the operation. A jaw fracture is treated by repositioning the bones and fixing them with splints through the teeth or with the help of intra- and extrafocal bone tissue synthesis.
When removing small or large molars from above, perforation of the maxillary sinus is possible. It is characterized by the presence of a through hole in the hole. The condition may be accompanied by bleeding and discharge of pus. An important stage of treatment is to control the formation of a blood clot in the hole in the absence of inflammation. To speed up healing, an iodoform turunda, a gentamicin sponge or a tampon with an anti-inflammatory and analgesic agent are placed on the hole. To ensure that the applications remain in place, they are fixed with a plastic mouthguard or bandage like a ligature in the shape of a figure 8 on the adjacent teeth. A removable denture can be used to cover the hole.
If clot formation does not occur, an iodoform tampon is secured to the socket to the edges of the gum using silk sutures or a mouthguard. The application should be worn for 5 to 7 days - during this time the wound begins to heal and there is no need for additional coverage. It is important to apply the tampon correctly so that it does not completely fill the hole, otherwise the patient faces sinus inflammation.
If a significant size hole is found at the bottom of the sinus, a blood clot may not form. Then the walls of the resulting hole are processed so as to remove all sharp parts, and then sutured without tension. If there is no positive effect, biological material can be applied to the hole, after which plastic surgery of the defect is performed with soft tissue. To speed up healing, an iodoform tampon is applied to the wound, which is fixed with a plastic plate.
If a root or whole tooth is inhaled, an emergency tracheotomy is performed to prevent the patient from suffocating. When an object passes into the lower parts of the respiratory system, it is removed using a bronchoscope, and for this the patient is transported to a suitable medical facility. If a tooth or part of it has been swallowed, the patient is monitored and the stool is independently monitored. Usually the object comes out naturally without causing significant discomfort.
If after tooth extraction the patient does not insert an implant in time, malocclusion develops over time - this is due to the natural displacement of the teeth towards the vacant space. If the dentition is not restored in time, bite correction with braces will be required, and the installation of a prosthesis will be accompanied by bone grafting.
Complications after tooth extraction in a child
Modern medical standards require that even children’s baby teeth be treated for caries. Until recently, they were simply removed, believing that healthy permanent ones would still grow in their place. But it turned out that this is not so.
Firstly, caries easily passes from baby teeth to permanent ones. Secondly, after the forced removal of baby teeth, a change in the bite often develops. As a result, it took a long time to correct the position of the child’s jaw using plates and braces. Therefore, doctors are increasingly deciding to place temporary implants even in childhood to maintain the correct bite.
The risk of developing malocclusion occurs not only in the postoperative period. There have been cases recorded when, during treatment, the doctor accidentally removed a baby tooth along with the germ of a permanent tooth. This is due to their close location in some children. Correction in this case is only possible with the help of a permanent tooth implant. Therefore, it is important to notice and treat carious lesions in children in a timely manner, rather than delay them and bring the situation to removal.
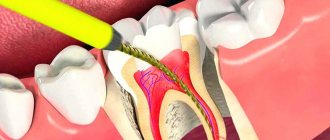
Why smoking after removal is undesirable
If you start smoking after leaving the dentist's office, you may experience dry socket problems. This means that the blood clot formed to protect the wound from the penetration of pathogens will collapse. Then the tissues will be left without a natural barrier. When smoking further cigarettes and eating food, irritating substances will enter the hole. In this case, there is no hope for quick healing.
The inflammatory process that has developed due to dry socket manifests itself:
- pain at the location of the torn unit;
- increased body temperature;
- accumulation of purulent masses in the wound;
- foul breath.
There is no point in hoping that the situation will normalize on its own. If you have a dry socket, you should visit your dental surgeon again as soon as possible.
Smoking and anesthesia are an undesirable combination
Doctors insist that patients do not smoke for the next two to three hours after extraction for good reason. Anesthetics used during dental surgery make the tissue completely insensitive and reduce the activity of some muscles and can change the breathing rate. It is very important to wait until their effect ends.
Nicotine and carbon monoxide entering the oral cavity during smoking a cigarette cause spasm of blood vessels and reduce oxygen saturation in the blood. The combination of all these factors leads to a situation where the tissues of the mouth do not receive enough oxygen, which is important for their restoration.
Should I rinse my mouth after tooth extraction: in what cases is this advisable?
If there is a high risk of infection of the wound surface or an inflammatory process already exists, gentle rinsing is considered appropriate. The doctor will definitely recommend doing antiseptic baths in the following situations:
- The tooth extraction was carried out against the background of already developing inflammation (pain, swelling, and edema were present before the operation). In this case, antibiotic treatment may be additionally prescribed for up to a week;
- If the gums were opened to release the pus (flux) that had accumulated in it. In this case, the doctor must wash the wound with an antiseptic solution in the clinic. At home you should do soda-salt and chlorhexidine baths;
- If there are foci of infection in the oral cavity: inflamed gums, untreated caries, decayed teeth, dental plaque. The advisability of antiseptic baths in such cases is explained by the reduced risk of infection of the wound surface of the hole.
It should be noted that even in the situations listed, we are not talking about rinsing, but about baths. In other words, the liquid should be taken into the mouth, held there for a while and carefully spat out. You should not overuse the procedure - it is best to take baths after meals and no more than five to six times a day.
Useful information about the effect of nicotine on the mucous membranes of the oral cavity
The mucous membranes of the human oral cavity are lined with very delicate and easily vulnerable epithelium. With the systematic use of tobacco products, nicotine and toxic tars damage tissue. The situation is aggravated by the negative impact of elevated temperature when inhaling cigarette smoke.
This is why smokers are often diagnosed with gingivitis and periodontitis. The components present in the smoke change the ligamentous apparatus of the tooth. The gums become inflamed. In the absence of adequate treatment and the persistence of a bad habit, the inflammatory process progresses. Then the unit becomes mobile.
Compounds present in cigarette smoke spasm peripheral blood vessels, disrupt tissue trophism and increase inflammation. Most often, the disease occurs without acute pain and bleeding, so the smoker is in no hurry to see a dentist. But, if you go to the doctor late, you can lose your tooth ahead of time.
How to speed up the healing of a hole
Dentists always give the patient individual recommendations that must be followed. But there are general rules that apply to all patients:
- Do not smoke for at least two to three hours.
- Promptly remove the tampon soaked in antiseptic from the postoperative wound. If you forget to do this, the fabric will become a suitable breeding ground for bacteria.
- Do not touch the blood clot covering the wound. It cannot be picked or felt. The speed of recovery directly depends on the state of the clot.
- When rinsing, do not make intense movements that will help wash out the clot. You just need to put the medicinal solution in your mouth and carefully hold it on the side of the extracted tooth.
- Do not apply medications to the affected area that have not been prescribed by a doctor. Such amateur activities can lead to dangerous complications.
- In the first three days after extraction, do not take a hot bath or steam in a bathhouse or sauna.
- Do not eat until the anesthesia wears off. Otherwise, you may bite the tissue of your cheek or lip.
- Take only those medications prescribed by your dentist. Sometimes doctors decide to prescribe antibiotics - they must be taken strictly according to the specified regimen.
How the regeneration process will proceed depends not only on the actions of the dental surgeon, but also on the behavior of the patient. Remember this!
What should a socket of an extracted tooth normally look like?
As you will see below, the blood clot after tooth extraction first has an intense burgundy color. Gradually, the surface of the clot becomes whitish/yellowish (this is normal, because fibrin effusion occurs). Normally, the blood clot should be dense the next day. If the clot becomes loose, this means it has disintegrated, and you should familiarize yourself with the symptoms of inflammation of the socket in order to consult a doctor in time.
What does the gum look like after tooth extraction (normal) –
Oral care after tooth extraction –
The oral cavity requires careful care after tooth extraction. Teeth should be brushed as usual, including the group of teeth in the area of the extracted tooth. The latter are simply cleaned more carefully so as not to injure the blood clot. You also need to carefully rinse your mouth from foam so as not to rinse the clot out of the hole.
You also need to care for your gums after tooth extraction (antiseptic baths, which we described above, are sufficient for this). But the lack of proper hygiene will cause the accumulation of soft microbial plaque, which is fraught with suppuration of the hole and the development of alveolitis. We hope that the article on the topic: Tooth pulled out, what to do - was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a dental surgeon, 3. National Library of Medicine (USA), 4. “Outpatient surgical dentistry” (Bezrukov V.), 5. “Propaedeutics of surgical dentistry” (Soloviev M.).