By length
This is a classification according to Kurlyandsky. According to this criterion, pathology is divided into the following types:
- Localized. Individual units or groups of them are erased. It is diagnosed mainly from the front side, for example, with a deep bite. Local compensation occurs due to the appearance of a hypertrophied alveolar process.
- Generalized. All rows are involved, the height of the bite changes significantly. Whether abrasion will be compensated by the body is determined by its individual characteristics.
Complications
What to do if teeth are worn out depends on the provoking factors. As discussed above, the lack of timely therapy leads to cosmetic defects and disruption of the chewing process. In addition, there are other consequences that affect the quality of life of patients:
- inflammation of the gums in the interdental spaces;
- gingivitis;
- diseases of the temporomandibular joint;
- loss of teeth;
- damage to nerve fibers and muscle tissue;
- uneven load distribution leading to traumatic articulation;
- malocclusion.
Manifestations of the disease
Symptoms depend on the form and severity of the disease. At the very beginning (at the stage of spotty or streaked form), areas with a changed color appear on the surface of the tooth. Stripes and lines are also visible. The enamel itself becomes rough, and small bulges appear.
Subsequently, small spots lead to the formation of larger pathological areas. Inhomogeneous mineralization of tooth enamel occurs. It breaks down and takes on a dull, matte color. At the same time, the smoothness and shine disappears.
A person with fluorosis complains:
- to increase sensitivity to temperature stimuli;
- cosmetic defect, as the color of the enamel becomes yellowish or light brown;
- fragility and rapid wear of teeth;
- frequent chipping;
- multiple caries.
X-rays reveal areas with reduced density, which indicates the process of demineralization, that is, a decrease in mineral substances in the enamel structure. It is for this reason that coloring substances are able to penetrate the porous structure of the tooth surface, which leads to the appearance of pigmented areas.
Diagnostics
Most people aged 50 years and older experience the physiological type of abrasion. The doctor needs to determine in time when the natural process turns into a pathological one. One of the main methods remains measuring the actual parameters of crowns. In addition, it is important to carefully study the shape of the dental units and determine areas of contact with antagonists. The height of the coronal part is compared with age standards established scientifically.
Diagnostic measures include assessment of fissures and enamel condition. The doctor pays attention to the patient’s facial expressions and appearance. It is important to talk in detail about your complaints and describe your feelings.
To assess how correctly the temporomandibular joint functions, electromyography is indicated. X-ray examination, electroodontodiagnosis and other procedures are carried out.
Classification
Teeth abrasion is divided according to:
- Stages
During the active stage, increased abrasion of hard tissue occurs. At the stabilization stage, their condition can be maintained at an acceptable level.
- Distribution
With localized abrasion, the front teeth are most often worn down. In generalized cases, all crowns suffer and the height of the bite decreases. In severe cases, the crown may end right at the gum.
- Shape
With a mixed form, the enamel wears off not only on top, it decreases on all sides. With horizontal, the occlusal surfaces suffer, with vertical, the lateral surfaces.
- Weights:
- Light or 1st degree (within the enamel)
- Transitional or 2nd degree (involving the superficial layers of dentin)
- Pathological or 3rd degree (with exposure of deep layers of dentin)
In grade 1, speech and chewing function are not affected. On the 2nd stage, hypersensitivity and chewing dysfunction appear. On the 3rd, pain in the temporomandibular joint begins. They radiate to the neck and head and can lead to hearing loss and decreased vision.
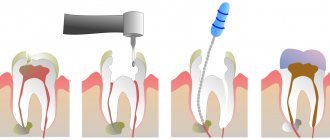
Treatment in dentistry
To eliminate pathological abrasion of hard dental tissues, you need to establish its cause and then get rid of it. The next step is to restore the configuration of the dentition. In the early stages, treatment with medications may be sufficient. If the symptoms are pronounced, only an orthopedist will help.
Medicines
The techniques used are based on the process of remineralization of the enamel layer. In this way, compensatory reactions are activated and mineral metabolism in hard tissues is normalized. Experts prescribe vitamin and mineral supplements with a high content of calcium and phosphorus. Additionally, pastes are used to reduce sensitivity. If the destruction has just begun and the dentin has not been damaged, this option for treating tooth wear can be very effective.
Orthopedic methods
If the defect is serious, medication alone is not enough; more radical correction is required. Most often, doctors use inlays and artificial crowns. If some units fall out, a bridge structure, clasp prosthesis or other types are installed. This therapy allows you to completely restore the functioning of the rows and evenly distribute the chewing load.
Dental fluorosis: treatment and prevention
Diagnosis is carried out at a dentist's appointment. Only a specialist will be able to distinguish the manifestations of fluorosis from a chalk spot, which is the initial stage of a carious lesion. An important distinguishing feature is that fluorous spots are multiple in nature and affect permanent teeth almost immediately after eruption. While initial caries in the spot stage is observed on single teeth.
Treatment is selected individually and depends on how severely damaged the enamel is. At the initial stage of the disease, it is recommended to conduct a course of professional whitening followed by strengthening the enamel using remineralization.
In this case, bleaching is carried out with a gentle composition based on inorganic acids. The number of procedures is selected by the doctor. Usually at least 10 sessions. During the whitening period, it is recommended to take calcium supplements. The result lasts for 6–8 months, then a second course of professional cleaning and bleaching is required.
The remineralization procedure helps strengthen the enamel structure, saturating it with minerals. Calcium and phosphorus compounds penetrate dentin and restore enamel from the inside. This procedure is carried out in several ways:
- Applications with a special composition.
- Electrophoresis or phonophoresis.
- Wearing mouth guards in which active gel is applied.
On average, at least 15 procedures are prescribed. Before the procedure, complete sanitation of the oral cavity is mandatory.
If the disease has already spread to the dentin, then simply bleaching will be ineffective. For moderate severity of fluorosis, methods of aesthetic tooth restoration are used:
- installation of ceramic veneers;
- restoration of tooth shape and color using crowns.
Such methods are recommended not only for aesthetic purposes, but also for medicinal purposes. They help stop further tooth decay and reduce enamel sensitivity.
Home care is also important - using fluoride-containing toothpastes, taking vitamin and mineral complexes, reducing the intake of fluoride from water and food.
How to prevent the disease from developing
The main preventive measure to combat fluorosis is to control the amount of fluoride in drinking water, as well as in the air. Such measures are especially important for areas where the amount of fluoride in the population’s water supply has been found to exceed the norms. Such events are held at the state level.
On an individual basis, it is recommended to use purchased purified water for drinking or use tap filters for additional purification. At the same time, it is important to engage in prevention from the moment the child is conceived. A pregnant woman should be especially careful when choosing food and drinking water. Additional intake of vitamins C, D, and calcium gluconate can reduce the risk of fluorosis several times, especially in children.
When a baby is born, it is recommended to feed him breast milk for as long as possible. After introducing complementary foods, use juices or dairy products instead of water, if possible. If you live permanently in an endemic area, you need to take your children to other areas every year for health improvement. Replacing the water source for 3-4 months helps strengthen tooth enamel and stop the development of the disease.
An important point in disease prevention is nutrition. Limit or completely eliminate products containing fluoride. These are sea fish, nuts, spinach, seaweed. You need to eat more fresh vegetables or fruits.
Also, after consulting a doctor, you can use medicinal remineralizing toothpastes or applications at home.
Prevention
To prevent pathology, it is necessary to regularly visit the dentist for preventive examinations at least once every six months. It is also important to promptly replace dental defects. In addition, all experts advise correcting malocclusion pathologies in a timely manner already in childhood or adolescence. Orthodontic therapy will help cope with the abnormal position of the teeth and prevent wear of the crown part.
You won’t have to decide what to do when the hard tissues of your teeth are worn away if you treat all the diseases that lead to it. For example, this includes bruxism, mineral metabolism disorders, thyroid pathologies, and problems with the digestive organs.
If the patient is at risk due to professional activities, it is necessary:
- use personal protective equipment;
- take a responsible approach to regular hygienic oral care;
- take courses of vitamins and minerals prescribed by your doctor.
The most important point remains the qualitative diagnosis of the transitional stage between physiological and pathological erasure. For this purpose, regular examinations and timely treatment of identified disorders are indicated.
Tooth discoloration: causes and treatment methods
04.10.2012 14:43- ZOOM4 whitening (+ comprehensive hygiene + set for home whitening and remedial therapy) — 30,000 rub
Causes of tooth discoloration
Discoloration of teeth can occur both from the surface of the teeth and from the pulp cavity. Tooth discoloration is conventionally divided into external (located on the surface of the tooth) and internal (located in the thickness of the tooth). External color changes can become internal over time.
- Widespread superficial staining of teeth with vital pulp is the result of consuming beverages or foods containing high levels of dyes. Tobacco causes a yellow-brown or dark discoloration, usually in the isthmus of the teeth and mainly on the lingual surfaces. When chewed, tobacco quickly penetrates the enamel and forms even darker stains, while marijuana can produce clear rings in the cervical part of the teeth near the gum line. Coffee and tea cause the formation of pronounced and persistent brown or black stains on tooth enamel.
- Internal staining can be caused by medications such as tetracycline. Teeth are most sensitive to tetracycline staining during the period of formation, i.e., from the second trimester of pregnancy until approximately 8 years of age. It is believed that tetracycline molecules are absorbed by dentin during the mineralization of teeth. If tetracycline-stained teeth are exposed to sunlight, they will gradually turn dark gray or brown. Since tetracycline is absorbed by dentin during the period of mineralization of the buds, adults whose teeth have already formed can use antibiotics without the risk of tooth discoloration. However, a semi-synthetic tetracycline derivative used to treat acne has recently been found to cause tooth staining in adolescents. It is believed that tooth pigmentation occurs due to the ability of minocycline to form chelates with iron and create insoluble complexes.
- In areas where drinking water contains large amounts of fluoride, children during the period of enamel development and mineralization of tooth germs can absorb excess amounts of fluoride, which causes disruption of ameloblast metabolism, leading to the formation of a defective matrix and improper mineralization - endemic enamel fluorosis. There are two types of dental damage caused by fluorosis: discoloration and surface defects. Affected teeth usually have a shiny surface and may be papery white with areas of yellow or brown (sometimes black) discoloration.
- Fillings and restorations also often cause discoloration of teeth. Destructuring of tooth-colored restorative materials, such as acrylics, glass ionomer cements, or composites, causes the tooth to appear gray or less saturated over time. Metal fillings and inlays made of amalgam, alloys of silver and gold, can be visible through the enamel.
- Oils, iodine compounds, nitrates, root canal filling materials, pins and other materials used in restoration can also cause tooth discoloration. The degree of staining of teeth is determined by the length of time during which these substances penetrated into the dentinal tubules.
- Teeth staining can also occur due to systemic diseases. Although there are many genetic or childhood diseases that change the color of teeth, most are rare.
Examples of such conditions are:
- Green-blue or brown discoloration of primary teeth, observed in children who suffered hemolytic jaundice in infancy. These stains are the result of postnatal staining of dentin with bilirubin and biliverdin.
- A characteristic brown staining of teeth caused by the destruction of a large number of red blood cells during erythroblastosis fetalis as a consequence of the incompatibility of Rh factors of the fetal matter.
- Red-brown discoloration of teeth in people suffering from porphyria, a very rare disease in which an excess amount of pigment is produced.
- Changes in the color, shape and structure of teeth almost inevitably occur as we age. The nature and extent of such changes depend on a combination of genetic factors, lifestyle and various bad habits. Years of smoking and drinking coffee have a cumulative staining effect. These and other types of plaque become even more noticeable due to the inevitable formation of cracks and other changes in the surface of the teeth within their crystalline structure, in the underlying dentin and pulp. In addition to abrasion and injury to teeth, old amalgam fillings and other restorations may begin to deteriorate. Even with a very careful approach to these problems, teeth will change color with age due to natural wear, as well as as a result of exposure to the oral environment. Initially, thinning of the enamel usually occurs. In this case, the buccal surface of the tooth becomes flatter and due to the loss of the transparent enamel layer, a gradual change in the color of the tooth occurs. When the enamel becomes thinner, a natural defense mechanism in the dentin and pulp begins the process of forming secondary dentin. This increased mass of dentin begins to darken. Thin enamel combined with darkened dentin gives teeth an “older” appearance.
- White spots, symmetrically located on the teeth of the same name, may be a symptom of enamel hypoplasia. One of the features of hypoplasia spots is that they are not stained with dyes, and the outer layer of enamel remains smooth and shiny. Chalky teeth can be a result of excessive whitening and prolonged use of soda for this purpose. Small chalky stripes - streaks located in the subsurface layers of the enamel are characteristic of the streaked form of fluorosis. The spotted form of fluorosis is characterized by the presence of chalky spots without stripes. The chalky-mottled form of fluorosis is distinguished by significant diversity. Typically, tooth enamel has a matte tint, and against this background pigmented spots with clear boundaries are visible. Sometimes a large number of spots and dots are found on the enamel. A pronounced whitish color may be due to dense plaque formed as a result of insufficient or improper individual oral hygiene.
- Depulped teeth lose their characteristic shine and acquire a more grayish tint. A similar, and sometimes more intense, color change is observed in teeth with pulp necrosis. Gray coloration can also be caused by poisoning with heavy metals - mercury and lead.
- Teeth with a greenish tint appear when their surface is damaged by specific fungi. Green staining can occur when a tooth comes into contact with copper amalgam fillings. Yellow teeth can be a result of exposure to bromine and iodine fumes, as well as constant consumption of strong tea and coffee. A dark brown border often appears in smokers. Dark brown (even black) color of teeth can appear due to professional contact with metals (manganese, iron, nickel). A change in the color of the tooth crown can occur immediately after an injury, especially in the cervical area on the palatal side, where the enamel layer is thinner, which is a diagnostic sign of injury. Thus, tooth discoloration clinically manifests itself in a wide variety of shades.
Teeth whitening
Changing the color and brightness of teeth is one of the most frequently requested procedures by patients from the dentist today. Geographically, all modern teeth whitening technologies originate from the United States of America.
At different times and different peoples had their own idea of beauty. And what one culture perceives as beautiful, another may consider ugly. For example, in Japan, more than 4 thousand years ago, there was a tradition of decorative staining of teeth. This procedure was considered cosmetic, and its main result was to give the enamel of the teeth a dark brown color.
Harmony of color, together with integrity, symmetry and proportionality, is the basic criterion for aesthetics in composition. Therefore, patients believe that among the factors influencing the attractiveness of a smile, the color of the teeth is the most important. The demand for cosmetic services has increased dramatically in recent years everywhere.
It is necessary to distinguish between the concepts of teeth whitening and teeth whitening.
→ Teeth whitening
This is the return of their natural color due to the mechanical removal of surface pigment deposits. Teeth whitening occurs due to the removal of supra- and subgingival dental plaque with ultrasound. Removing dental plaque using the Airflow device. Polishing teeth with brushes with special abrasive pastes. These manipulations will lighten your teeth to the natural color given to you by nature.
→ Whitening
- this is already a change in the shade of the tooth due to the release of atomic oxygen, which penetrates the enamel and dentin of the tooth and breaks down the pigment. There are several methods of teeth whitening. All professional whitening methods are divided into clinical (the procedure is performed by a dentist in a dental office) and home (the patient independently uses trays with whitening gel at home). Clinical whitening systems come with light and chemical activators. Traditionally, hydrogen peroxide is used in clinical systems - 25 -38%. Such systems can whiten teeth up to 15 shades. Home systems contain lower percentages of hydrogen peroxide up to 10%. The effectiveness of home whitening is significantly lower - from 1 to 8 tones. As for the agents that form the basis of any bleaching system, nothing fundamentally has changed since 1884, when Harlan first proposed the use of hydrogen peroxide. The advantage of professional whitening is that the procedure is carried out and supervised by a doctor.
Indications for teeth whitening
- The patient's desire to make his teeth lighter.
- Mild and moderate form of fluorosis.
- Age-related changes in tooth color (yellowing).
- Coloring as a result of bad habits.
- Penetrating staining from frequent consumption of coloring foods and drinks.
Contraindications
Are common
- Patient's age (minor children and adolescents).
- Pregnancy and breastfeeding.
- Allergic reactions to whitening components.
- Taking light-sensitive drugs such as doxycycline, tretinoin, ciprovloxacin, hydrochlorothioside, etc.
- General diseases: cancer and endocrine diseases, bronchial asthma, hypertension.
- Inflated patient expectations from the whitening procedure.
Local
- The presence of carious cavities, fillings, restorations, crowns in the whitening area.
- Wide pulp chamber.
- Enamel hyperesthesia (increased sensitivity of teeth).
- Significant loss of enamel as a result of pathology and age.
- Acute and aggravated periodontal diseases.
- Diseases of the oral mucosa.
- Diseases of the temporomandibular joint accompanied by limited mouth opening.
- The patient has a pronounced gag reflex.
Possible complications
- The appearance of hyperesthesia (can last from several hours to several days). To eliminate it, it is necessary to conduct a course of retherapy before and after the whitening procedure. The use of desincitizers, special rinses and toothpastes for sensitive teeth.
- Irritation of the oral mucosa (burning).
- Color regression. Within 2 weeks after the whitening procedure, the oxidation process causes a change in the optical qualities of the tooth, giving it a more opaque appearance. After 2 weeks, the oxygen dissipates and the tooth acquires a real light shade.
- Change in taste sensations. It is temporary.
To maintain the results obtained, the patient must follow the following recommendations:
- Follow the rules of personal oral hygiene every day.
- In the first 48 hours after the whitening procedure, do not eat foods with coloring, and in the next 2 weeks follow a clear diet.
- Visit the dentist regularly at least once every six months.
- Repeated course of whitening after 1.5-2 years (if necessary).
Scheme of the teeth whitening procedure
- Questioning
- History taking
- Determining the cause of dental discoloration
- Availability of indications and contraindications.
- Discussion of complications and side effects after the teeth whitening procedure.
- Discussion of patient behavior after a whitening course.
- Registration of the patient's informed voluntary consent to the whitening procedure.
- Determination of the initial color of teeth is carried out using the Vita scale + photographs.
- Professional oral hygiene.
- Applying a protective gel to the mucous membrane.
- Applying whitening gel to teeth (3 sessions of 15 minutes each)
- Registration of the results obtained (color according to the Vita scale + photographs, presence of complications)
- Carrying out a course of remediation after the whitening procedure.
- Recommendations after the whitening procedure, individual selection of oral hygiene products, setting a date for re-examination.
- Re-inspection. Determining the need for a repeat course of whitening. To maintain stable results, prescribe home teeth whitening products (if necessary)
- Repeated whitening procedure (if necessary).
Toothpastes with whitening effect
Patients often ask: is it enough to use whitening toothpaste to whiten teeth?
The main purpose of whitening toothpastes is to maintain the results achieved by professional whitening.
Whitening components included in toothpastes:
- Substances that dissolve plaque (proteolytic enzymes: bromelain, papain)
- Substances with enhanced cleaning properties (sodium bicarbonate)
- Substances that suppress plaque formation (xylitol, bromelain, triclosan with copolymer)
- Substances that inhibit plaque mineralization (pyrophosphates, zinc citrate)
When deciding to use toothpastes with a whitening effect, you need to consider a number of points: Toothpastes based on polishing abrasives are widely available on the market. Constant use of such pastes leads to abrasion of tooth enamel, so such pastes are not recommended for regular use. You can choose different modes of their use. But such pastes are absolutely not suitable for people with cervical dental defects.
Sometimes toothpaste manufacturers promise to lighten teeth by several shades. This effect is achieved using toothpaste that contains carbamide peroxide, as well as home whitening systems. In this case, the concentration of carbamide peroxide should be 8-10 percent. The main distinguishing feature of this toothpaste is its specific peroxide taste. These pastes are technologically very difficult to produce, so there are only a few offers on the market.
Let's sum it up
What to do if the lower front teeth or upper teeth are worn out, pain and other unpleasant symptoms appear? First of all, you need to go to the dentist to conduct a thorough diagnosis and identify the exact causes of the pathology. The longer the patient ignores the presenting signs, the more severe the consequences for him. In order not to encounter this phenomenon, it is necessary to take preventive measures, especially for those at risk.
Sometimes the enamel wears away due to age-related changes. In this case we are talking about a natural process. Which group should the problem be classified into, and whether treatment should be prescribed, should be decided solely by the doctor.
Types of dental hypersensitivity
Causes of sensitive teeth
Today, patients often experience enamel sensitivity after whitening, both independently and in the dentist's office. To ensure that the aesthetic procedure does not cause discomfort, you need to remember important points:
- Whitening toothpaste has an abrasive effect, and it is not recommended to use it more than 2 times a week.
- Laser whitening and the ZOOM 4 machine are relatively safe methods, but they use a gel with carbamide peroxide, which often causes irritation.
- Kits with whitening compounds should be selected based on the jaw cast. If this is not possible, it is better to buy thermoplastic mouthguards.
Another case is sensitivity after installing a filling. At this point, the tooth “removes” after an anesthetic injection, and pain for 48 hours is normal. To minimize discomfort, the first two days you need to:
- Avoid hot tea and coffee.
- Avoid chewing gum and sweets.
- Chew food thoroughly, preferably without solids.
Enamel hypersensitivity in early pregnancy is associated with intoxication and hormonal changes in the female body. Here it is important to consult a dentist in time and consider a course of restorative therapy.
Causes of wedge-shaped tooth defects
Wedge-shaped tooth defects have several causes. Depending on the general condition of a person’s oral cavity, one or more of the following factors may give rise to the development of a wedge-shaped dental defect.
Irregular oral hygiene
A wedge-shaped defect, like most oral diseases, develops due to the active activity of pathogenic bacteria. Therefore, it is very important to carry out thorough and regular oral hygiene. You need to brush your teeth twice a day, morning and evening, and do not neglect additional hygiene products - mouth rinses, dental floss. It is very important to have professional teeth cleaning twice a year - during professional cleaning, teeth are cleaned in hard-to-reach places (this includes the neck of the tooth).
When brushing your teeth, you should not make movements in the horizontal plane. The outer surface of all teeth must be cleaned with vertical movements directed from the gums to the cutting edge of the teeth.
Wedge-shaped defect as a concomitant disease
A wedge-shaped dental defect can manifest itself as a concomitant disease. There is a high probability of developing a wedge-shaped defect due to gingivitis (inflammatory process in the gums) and periodontitis (inflammatory process of the tissues surrounding the tooth). A characteristic feature of these diseases is a considerable amount of harmful deposits on the tooth surface. Also, gingivitis and periodontitis are characterized by the release of fluid from the gingival sulcus. The liquid tends to leach calcium from tooth enamel, thereby significantly weakening the outer, protective surface of the teeth, exposing the teeth to the formation of a wedge-shaped defect.
Incorrect bite can cause a wedge-shaped defect
A patient’s malocclusion can also cause the development of a wedge-shaped defect. If a person has an incorrect bite, then when chewing food, the load on the teeth falls unevenly. And since the enamel at the neck of the tooth is very thin, it is subject to greater abrasion. This contributes to the rapid development of wedge-shaped dental defects.
General diseases of the body
The development of a wedge-shaped tooth defect may signal the presence of a general disease of the body. Doctors say that wedge-shaped dental defects often develop in patients with problems with the thyroid gland. Also, wedge-shaped dental defects are a common companion for people suffering from heartburn.
Prevention from destruction
- A balanced diet rich in vitamins and microelements: meat, fish, vegetables, fruits, cereals. It is advisable that all these products be present in the daily diet.
- Monitor your vitamin D level, as calcium absorption depends on it.
- You should spend more time outdoors and, if necessary, take vitamin D supplements. To replenish calcium reserves, eat more legumes, dairy products, and almonds.
- Give up bad habits: do not chew pencils and pens, do not open bottles with your teeth.
- Regularly undergo preventive examinations at the dentist. At the first signs of enamel destruction, consult a doctor immediately.
As practice shows, in many cases a damaged crown can be saved. The main thing is not to delay your visit to the dental clinic. Be healthy!
How does a wedge-shaped tooth defect develop?
Tooth enamel is constantly exposed to environmental factors. Many of them have a negative effect on the enamel, causing it to wear off. This especially applies to factors such as frequent consumption of citrus fruits (the acid in oranges and lemons is a “solvent” of enamel), carbonated water, wine, sweet and sour foods, as well as smoking.
Naturally, eating sweet or sour foods in itself cannot cause severe forms of wedge-shaped dental defects. But such irritating environmental factors reveal and strengthen the underlying causes of the development of the disease - poor oral health, reduced immunity.
The enamel on the neck of the tooth is the thinnest, much thinner than, for example, that of a dental crown. Therefore, aggravating factors in the development of the disease “attack” first of all the neck of the tooth, turning over time into the appearance of a wedge-shaped defect.
Causes of tooth decay
It happens that the enamel becomes fragile, cannot cope with the load and begins to crumble. Typically this process begins with the formation of small microcracks. Over time, they increase, leading to chips.
Tooth decay is influenced by many factors, both natural and mechanical.
- Poor hygiene. The accumulation of tartar and soft deposits create a favorable environment for the growth of bacteria. Those, in turn, release substances that destroy the enamel.
- Lack of vitamins and microelements that affect the formation of dental tissue, for example, vitamin D, calcium, phosphorus, etc.
- Abuse of sweets, alcohol, sour foods, seeds, smoking, sweet sodas. Simultaneous consumption of foods at different temperatures (ice cream and hot coffee).
- Bad habits: the habit of biting nails, a pen or pencil, opening a bottle with your teeth.
- Bruxism.
- Heredity.
- Diseases of the thyroid gland and endocrine system.
- Age-related changes.
- Pregnancy.
- Chronic diseases: arthritis, diabetes.
- Poor quality water.