The inflammatory process of the periodontal soft tissues that occurs during complicated or improper teething is called pericoronitis. Inflammation during teething can occur in both adults and children, regardless of the location of the problem tooth, but most often pericoronitis of the wisdom tooth develops (it is also often called the “eight” or third molar).
Causes of inflammation and swollen gums during teething
The main prerequisites for the development of pericoronitis are:
- Mechanical injuries to the gingival tissue over the tooth germs due to hard foods, too hard toothbrushes, as well as due to other damaging factors.
- Long-term or difficult teething.
- Favorable conditions in the mouth for the accumulation of bacterial plaque and food particles under the gingival margin (insufficient hygiene, peculiarities of microflora in the oral cavity).
Swollen gums during teething are easily susceptible to traumatic influences, which leads to the development of inflammation. In this case, teething itself can be difficult for the following objective reasons:
- Dense bone tissue in the “eight” zone; bone compaction is most often formed because there are no milk teeth in this zone.
- There is not enough space for the “eight” in the dentition.
- Thickening of the gums and periosteum in the posterior part of the jaw is usually explained by the characteristics of embryogenesis.
Even one of these factors can cause the disease.
Diagnosis of gingivitis
The diagnosis should be made by a doctor in a dental clinic; only through a visual examination will he be able to determine the status of the disease and differentiate it from many others, which at an early stage may manifest the same symptoms.
The main clinical signs by which a dentist can make a diagnosis are:
- the presence of erythematous formations at the gum edge;
- looseness, separation of soft tissues from the dentition, the appearance of pockets larger than 3 mm;
- when pressed with a dental spatula, exudative and bloody discharge is observed, in some cases with a putrid odor;
- obtaining the result of smears to determine the pathogen.
The last point is one of the most important in making a diagnosis and prescribing adequate procedures. Depending on the type of bacteria that caused the disease, various antibiotics and antiseptics can be used to speed up recovery. Also, after collecting an anamnesis, based on diagnostic results, the doctor needs to identify the root cause in order to further prevent the risk of relapse.
Features and risk factors
During difficult and prolonged eruption, the tooth germ practically does not change its position, and a significant part of its chewing surface is covered with a flap of gingival or mucoperiosteal tissue, the so-called “hood”. The flap covering the tooth germ forms a kind of pocket in which food debris and bacterial plaque accumulate. A moist nutrient medium creates optimal conditions for the intensive reproduction of pathogenic microorganisms, which, in turn, actively secrete waste products that are toxic to our body. This provokes the development of an infectious-inflammatory process in the tissues surrounding the problematic tooth germ.
Most often, inflammation of the gums occurs when a wisdom tooth erupts in the lower jaw, which is due to the anatomical structure of the jaw and the lack of space for third molars. In modern people, the jaw arch is approximately 1-1.2 cm smaller than in our distant ancestors, but the size of the teeth has remained the same. This is why the “eights” are cut much later, when the body as a whole and the dental system in particular have already formed - and because of this, it is difficult for the new tooth to find the “right” place on the dental arch.
Since wisdom tooth pericoronitis is the most common type of disease, people over the age of 18 are primarily at risk (usually “eights” are cut at the age of 20-25, but for some this process can take up to 30 years) . As for pericoronitis in children, it usually occurs against the background of insufficient oral hygiene in a child or with infectious diseases of the oral cavity (caries, gingivitis, stomatitis), which complicate teething in children and require treatment. Accumulations of plaque and hard dental deposits significantly increase the risk of developing the disease, so timely and regular removal of tartar can serve as a good preventative method.
What you need to know about gum disease in children
Healthy gums of a child are very vulnerable and delicate pale pink tissues that are easily subject to all kinds of injuries, which is not so typical for the tissues of the oral cavity of an adult. Fortunately, they are capable of rapid regeneration. It is also interesting that children’s gums can reflect the general condition of the body, acting as a litmus test for systemic diseases.
Among the most common diseases around dental tissues and gums
- Gingivitis
This inflammation occurs in 80% of children. The development of the disease in infants is facilitated by the adverse effects of general and local factors. - Gum atrophy
Up to 50% of the child population faces this serious problem. - Stomatitis
Various types of this disease are diagnosed most often in infants and preschool children. - Periodontitis
In this disease, inflammation develops in the periodontal tissues. About 5% of young dental patients are diagnosed with this condition. - Periodontal disease
Similar degenerative changes that affect periodontal tissues practically do not occur in childhood.
Gum diseases that most often occur in children
Inflammatory diseases
Gingivitis is an inflammation of the gums that occurs due to general or local exposure. Over time, untreated gingivitis can develop into periodontitis, that is, a condition where inflammation affects the periodontal tissues (bone tissue and muscle ligaments that hold the tooth in the jaw). In children, this disease is extremely rare, but still, preventive measures should not be neglected. If the development of a serious disease is not noticed in time, this can lead to loosening and further loss of the tooth. If gingivitis in a child responds well to treatment, and you can get rid of it without health consequences, then periodontitis, as a rule, becomes chronic, which is practically incurable.
The inflammatory process that accompanies the granulating form of periodontitis can provoke the formation of a cyst, and even the occurrence of a fistula on the gum. However, these complications are more typical for carious disease of dental tissues. Be that as it may, if you notice that the baby’s gums have acquired a bright red color, and deep grooves have appeared between the teeth and gums, and there is an unpleasant odor coming from the child’s mouth, then most likely the inflammation has affected not only the gums, but also deeper located periodontal tissues. You need to immediately contact pediatric dentistry, where the doctor will promptly prescribe comprehensive treatment.
Dystrophic diseases
Very often, infants and preschool children experience a pathology such as gum atrophy. The development of this negative phenomenon is facilitated by:
- incorrect orthodontic treatment;
- oral injuries;
- crowded teeth;
- all kinds of malocclusions.
Atrophy of gingival tissue is usually local in nature. It usually develops in the area of the canines and front incisors. The development of the disease is accompanied by mild inflammation. The child feels virtually no pain and has no complaints. After some time, degenerative changes cause exposure of the neck of the tooth and its root, the appearance of pathological sensitivity and severe pain.
Periodontal disease is a dystrophic disease that affects all periodontal tissues. This pathology practically does not occur in children. Its development is possible only in seriously ill babies whose immune systems are suppressed. Their body is in a state of deep vitamin deficiency. This disease is characterized by atrophy of the gums and other periodontal tissues. This incurable process can lead to complete resorption of bone tissue. In most cases, teeth that have already acquired unhealthy mobility cannot be saved. Only surgical intervention aimed at removing the affected tooth can bring a certain effect.
Risk factors
Local risk factors
Gum disease in children can be caused by a number of local factors:
- Microbes
Tartar, the formation of which is promoted by poor-quality oral cleaning, can provoke various gum diseases. First, yellow plaque accumulates on the teeth, in which pathogenic bacteria feel at ease. Then, at first glance, harmless plaque turns into hard dental deposits, which subsequently cause serious pathological changes in dental tissue and gums. - Teething
The development of gingivitis can be triggered by teething, as well as their replacement with permanent ones. - Uneven load on the dental system
This entails the development of malocclusion in the child, lethargy of chewing, the habit of chewing food on one side, a short frenulum of the tongue and lips contribute to the occurrence of gingivitis. - disruptions in the functioning of the endocrine system (adolescence and associated hormonal changes);
- diseases of the cardiovascular system;
- diseases of the gastrointestinal tract;
- respiratory system diseases;
- pathologies of the immune system, autoimmune diseases;
- hypo- and vitamin deficiency.
- swelling of the gums and bleeding;
- bad breath;
- burning and itching in the gums.
General risk factors
The following systemic diseases and changes in the functioning of body systems can provoke gum disease:
Attention: first signals!
The following factors can signal the development of gum disease in children:
The occurrence of these symptoms necessitates a visit to the dentist. The sooner the child receives help from a qualified specialist, the higher the likelihood of easy relief of the disease at the initial stage and the opportunity to reverse the nascent process.
Pericoronitis, symptoms and types
With pericoronitis, the symptoms largely depend on the form of the disease - acute or chronic. Acute pericoronitis is characterized by:
- Aching intense pain in the area of the cutting tooth, the pain intensifies under the influence of food and mechanical irritants (hygienic procedures, chewing, touching, etc.).
- Difficulty chewing food, complicated swallowing. A few days after the onset of inflammation, it becomes difficult to open the mouth and severe pain appears.
- Swelling and hyperemia of the mucous membrane.
- Enlargement of regional lymph nodes, sometimes the lymph nodes become painful when touched.
- Externally noticeable swelling of the cheeks a few days after the onset of the inflammatory process.
- General deterioration in health - weakness, lethargy, prolonged low-grade fever (increased temperature to 37-37.5 degrees).
- Bad breath, which is caused by the decomposition of food particles and the active activity of microorganisms in the “hood” space.
Acute pericoronitis can occur in a serous (catarrhal) or purulent form: in the first case, the signs of inflammation are more pronounced, the pain is more intense, and there is no purulent discharge. In the second case, purulent exudate flows freely from the inflammatory focus, due to which tissue tension is somewhat reduced and the symptoms are less pronounced. A person may feel like their condition is gradually improving, when in fact the infection is simply spreading to other tissues in the mouth.
If treatment for acute pericoronaritis was not carried out or was carried out at home, the disease gradually becomes chronic: the severity of symptoms decreases, while exacerbations of pain and discharge of pus into the oral cavity are periodically observed. In this case, there is a high risk of developing severe complications.
Why does an abscess occur?
There can be many reasons for the formation of a lump (fistula, swelling), but the most common of them is undetected or ignored caries. Not all children maintain oral hygiene and eat properly, and not all parents carefully control this, which causes caries to appear on one or several teeth at once.
If caries is not treated, it will develop into pulpitis, extending beyond the tooth area and affecting the upper part of the root. As a rule, a lump appears just near the tooth whose root is inflamed. Typically, a lump can be noticed near a tooth with caries or with a filling that was placed long ago or poorly; Another common reason for its appearance is an injury received from a strong blow or an accidental fall, which can trigger the onset of the inflammatory process.
Stages of development of an abscess:
- As a result of caries, the infection penetrates into the pulp, affecting the root tip.
- Pus begins to form near the top of the root.
- Purulent formations fall under the mucous membrane of the gums.
- A cyst appears, looking like a small lump from the outside.
The most important symptom of an abscess is a soft and painful swelling, even with slight pressure.
Sometimes, due to an excess of pus, the lump may burst under pressure, and then a fistula appears - a small hole in the gum, which is connected with the source of inflammation located in the upper region of the root. A feature of the fistula is the constant release of purulent formations.
If inflammation decreases for some reason, the fistula may close on its own. However, when the child’s immunity decreases and the inflammatory process begins again, accompanied by pus formation, the appearance of a fistula will not be long in coming.
Complications of the disease
In the case when treatment of the gums during complicated tooth eruption was not carried out, serious complications of the inflammatory process develop:
- Periostitis, or flux, is inflammation of the periosteum.
- Osteomyelitis - in this disease, inflammation affects both the bone tissue itself and the bone marrow, gradually leading to bone resorption. This can cause abnormal jaw fractures.
- An abscess when the infection spreads to nearby tissues. Purulent inflammation leads to the melting of muscles and fatty tissues with the formation of a large accumulation of pus.
- Cellulitis is the next stage of a purulent process after an abscess, which does not have clear boundaries. Such purulent inflammation is a serious threat to the patient and is treated in a maxillofacial hospital.
These complications are usually difficult to treat, require a serious systemic approach and can lead to irreversible consequences. Therefore, if a person suspects he has pericoronitis, treatment should begin without delay in order to prevent the condition from worsening. You need to be especially careful if gum inflammation occurs during teething in children, since the children's immune system is still immature, the body's resistance to infections is lower and the process quickly becomes more severe.
Pericoronitis, treatment in children and adults
It should be noted right away that for pericoronitis, treatment at home can only reduce the symptoms of inflammation, but not solve the problem. Therefore, all home methods (rinsing with antiseptics, applying anti-inflammatory ointments, etc.) can only be used as a way to relieve inflammation during the eruption of wisdom teeth and reduce pain - this is a temporary measure before visiting the dentist.
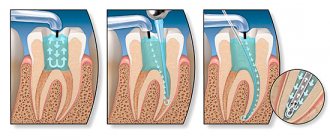
In a dental clinic, in case of complicated teething, treatment will depend on whether the problem tooth should be preserved or whether it should be removed. If preserved, the doctor performs surgical excision of the “hood” under local anesthesia. This eliminates conditions for the accumulation of food and the growth of bacteria, and also facilitates teething. After excision of the “hood,” the patient is prescribed antiseptic therapy (rinses, baths) and, if necessary, antibiotic therapy.
In cases where tooth extraction is indicated due to their incorrect position on the jaw, lack of antagonists, or insufficient space for full eruption, the doctor immediately removes the problematic tooth and prescribes antiseptic therapy to the patient.
In some cases, at the initial stages of the inflammatory process, conservative therapy can be preliminarily applied - local treatment with antiseptic rinses and the introduction of an iodoform tampon into the “hood”. However, local therapy does not always give a positive result; moreover, it is appropriate only at the initial stage of the disease; in other cases, surgical intervention will be required.
When it comes to teething in children, treatment is always aimed at preserving the teeth (except for those cases when dystopia is clearly expressed and the doctor sees that preserving is useless).
Should I give my child antibiotics?
The doctor may prescribe your child broad-spectrum antibacterial drugs to relieve inflammation and reduce the risk of complications after the procedure. Antibiotics help cope with pathogenic flora and prevent secondary infection of tissues, but they can only be used as prescribed by a doctor in the recommended dosage.
How to treat an abscess on the gum
Penicillins are becoming the drugs of choice for the prevention of complications in children. They are available in tablets and capsules, and young children can be given the medicine in suspension form. Commonly prescribed drugs with high effectiveness and minimal side effects include:
- "Augmentin";
- "Amoxiclav";
- "Amosin";
- "Flemoxin".
"Augmentin"
Children over 10 years of age may be prescribed Metronidazole in a dosage appropriate for their age. In case of severe inflammation or complicated pathology, doctors recommend taking potent antibacterial drugs from the group of cephalosporins or macrolides (Zinnat, Sumamed, Ciprofloxacin). The course of treatment depends on the chosen drug and the severity of the inflammatory process and can range from 3 to 10 days.
"Sumamed"
Note! Taking antibiotics of any group must be combined with the use of products that include probiotic cultures, lactobacilli, prebiotics and bifidobacteria. For young children, it is best to give Bifiform, Linex or Bifidumbacterin (provided there is no lactase deficiency). For children over 7 years old, Normobakt and Acipol are suitable.
"Bifiform"
Diagnostic features
History of the disease Pericoronitis sometimes looks like a completely different disease of the oral cavity - for example, its symptoms can be confused with periodontitis (inflammation of the peri-apical tissues of the oral cavity) or pulpitis (inflammation of the dental pulp). The pain in these diseases is very similar, and periodontitis is often accompanied by hyperemia and swelling of the gums. One disease can be distinguished from another by the following signs: with pulpitis there is no pain when opening the mouth and no noticeable swelling of the gums, and periodontitis develops only at the tops of the roots of fully erupted teeth. You also need to pay attention to the presence of a characteristic “hood” - a photo will help you assess how it looks with pericoronaritis.
Prevention
In some cases, especially when it comes to inflammation of the gums during teething in children, preventive measures will help prevent the disease: careful regular oral hygiene, timely removal of tartar and soft deposits, visits to the dentist for diagnostic examinations at least once every six months.
If pericoronitis is caused by the anatomical features of the structure of the dental system and the lack of space for the lower “eights” on the dental arch, preventive measures will only smooth out the course of the inflammatory process (due to timely cleaning of the oral cavity from bacterial plaque and food particles that create favorable conditions for inflammation) and identify the problem in time (subject to regular dental examinations).
Why is gingivitis dangerous in children?
Gingivitis is an inflammation of the gums that occurs as a result of the adverse effects of local and general factors. In children, it occurs quite often: between the ages of two and four years, its prevalence is 2%, and by the age of thirteen, gingival inflammation occurs to one degree or another in 80% of children. Often the disease does not progress beyond gingivitis, since it can be easily cured, avoiding more serious problems. However, if the process is started, the inflammation from the gums will spread to other periodontal tissues (the child will develop periodontitis) and will become a chronic condition, the symptoms of which will need to be relieved with each relapse.