Dental treatment
If the dentist does not treat the tooth correctly or completely, it can cause swelling in the cheek.
Causes:
- Allergic reaction.
It appears in the patient as a result of intolerance to the components of the filling. To eliminate swelling, you should visit a doctor and replace the installed filling with a hypoallergenic one.
- Removal of a tooth.
If the cheek is swollen after surgery, then the patient probably ignored the doctor’s recommendations and ate solid or hot foods.
- Nerve removal.
Swelling occurs if part of the nerve is not removed. It is important to see a dentist immediately so as not to lose a healthy tooth.
- Gum section.
Usually required to remove accumulated pus. If the swelling does not subside while taking anti-inflammatory drugs, this may be a serious symptom that requires the attention of a specialist.
Cheek swelling as a complication after tooth extraction
If a patient has had a tooth removed, then swelling is a natural phenomenon. However, it often indicates that the operation was performed incorrectly or the development of a pathological process due to the patient’s failure to comply with the recommendations in the postoperative period. To recognize the problem and contact a specialist in a timely manner, it is important to know that:
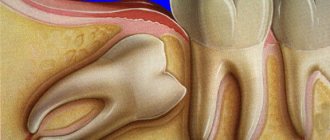
- Swelling is considered normal after removal of an upper wisdom tooth. In this case, the swelling spreads to the upper part of the face. Swelling of soft tissues is very natural, because the area where the tooth roots are located in this case also contains a large number of blood vessels of various sizes.
- Swelling is predictable after complex removal of lower wisdom teeth. If the problematic “eight” was sawed out or split and removed in parts, with a high degree of probability we can talk about subsequent swelling of the soft tissues of the face.
You can understand that swelling does not indicate pathology by the nature of the phenomenon. As a rule, it does not occur immediately after extraction, but the next morning. The swelling increases throughout the day, causing serious discomfort, and remains at the same level the entire next day. On the fourth day after tooth extraction, the swelling should subside and the discomfort caused by it should decrease. Against the background of “normal” edema, there is no fever or throbbing pain.
What to do if your cheek is swollen
To reduce swelling, you can use one of the following tips:
- Rinse your mouth with a solution of salt and soda.
This remedy has an antiseptic effect and helps destroy pathogens. You can enhance the effect by adding a couple of drops of iodine to the solution.
- Use chamomile infusion to rinse
, sage or other medicinal herbs that have anti-inflammatory properties.
- Apply a cold compress to the swollen cheek
if the swelling is caused by a bite or mechanical injury. This method is contraindicated in patients who have an elevated body temperature or a tumor that develops due to inflammatory processes. Warming compresses are not recommended.
- Lotions with aloe or Kalanchoe juice.
A cotton wool soaked in the juice of the plant is applied to the inside of the affected cheek.
If the described methods do not eliminate the problem, you should seek help from a doctor. The day before, you should not take painkillers and anti-inflammatory drugs, so as not to complicate the diagnosis.
Why do my gums or cheeks swell?
In most cases, swelling of the gums or cheeks is caused by purely dental reasons:
- Flux
During gumboil, the gums become swollen and painful, and the temperature rises. The development of a tumor begins with an ordinary carious cavity. It gets infected, which eventually leads to tooth decay. Pus accumulates and begins to look for a way out. The cheek swells greatly and a white spot appears on its surface. Without treatment, a fistula forms in this place, and the cheek turns into a huge purulent wound. If you do not seek help from a doctor in time, blood poisoning may occur.
- Removal of a tooth
This operation inevitably involves damage to soft tissue, and swelling is a natural phenomenon. After a while it subsides. If this does not happen, and the gums swell more and more, then you need to urgently visit a doctor. Causes of severe swelling can be:
- a large accumulation of pus,
- incipient periostitis (inflammation of the periosteum),
- infection in the wound.
If you notice swelling of the cheeks and gums, or tissues of the oral cavity, then you need to consult a dentist.
The doctor will determine the exact cause, begin treatment or refer you to another specialist.
Leave your phone number. The clinic administrator will call you back.
By leaving a request on the site, you consent to the processing of personal data
Make an appointment
Initial consultation with a dentist
For free!
- Inflammatory infiltrate
It usually occurs against the background of pulpitis or periodontitis. Pus begins to accumulate in the soft tissues, which causes the appearance of phlegmons and abscesses. It is considered a very dangerous disease because it can lead to big troubles.
- Periodontal disease
Swelling is accompanied by aching or sharp pain. There is no conservative treatment; surgical intervention is necessary. Often it is necessary to remove some teeth and install dentures.
- Teeth chips
The sharp edges of a destroyed tooth begin to scratch the inner walls of the cheek, which leads to inflammation and severe swelling.
- Wisdom tooth growth, pericoronitis
The eruption of the figure eight often leads to inflammation of the gingival hood. Swelling, as a rule, extends to both the cheek and gum.
- Carious teeth
Advanced caries often causes not only the gums to swell, but also the tonsils and cheeks. After eliminating the cause, the swelling gradually goes away. Folk remedies are useless here; urgent medical help is needed.
- Cyst
Depending on the type of cyst, its shape, and location, the doctor decides on conservative or surgical treatment. In some cases, a consultation with an oncologist may be required.
- Gum disease
Swelling is one of the main signs of inflammation of periodontal tissue. Without treatment, the disease quickly becomes chronic and difficult to treat. There is a high chance of losing a tooth.
In addition to the reasons listed, swelling of the gums and cheeks can be caused by:
- inflammation of the facial nerves;
- pathologies of the maxillofacial skeleton;
- allergies;
- disruption of the immune system;
- inflammation of the submandibular and parotid lymph nodes as a result of an infectious disease;
- malignant neoplasm;
- facial injury;
- diseases of internal organs, such as the heart;
- eye diseases;
- blood pathologies.
The dangers of flux and the dentist's tasks
It is the identification of such foci and their elimination, especially in persons suffering from inflammatory processes of internal organs and in pregnant women, that is one of the essential tasks of a dentist. Untimely sanitation of the oral cavity or its absence in the presence of teeth affected by chronic periodontitis can lead to the development of a number of more severe inflammatory processes, the first of which is acute purulent periostitis.
Purulent periostitis
This disease is an acute purulent inflammation of the periosteum of the alveolar process of the jaw and accounts for up to 40% of complications of odontogenic infection, mainly chronic periodontitis. The cause of the development of this disease is most often large molars, which are primarily affected by the carious process.
The clinical picture of acute purulent periostitis is diverse and depends on the nature of the microflora, localization and extent of the inflammatory process. When the upper jaw is affected, the external manifestations of acute inflammation, in particular hyperemia, infiltration and swelling of soft tissues, are usually more pronounced than when the flux is localized in the lower jaw. However, the phenomena of general intoxication are more pronounced when the alveolar process of the lower jaw is affected, which is due to the difference in the anatomical and topographic relationships of soft tissues and jaw bones.
When examining the oral cavity, smoothness or swelling of the transitional fold of the mucous membrane of the vestibule of the oral cavity, its hyperemia, and sharp pain when touched by the dentist’s hands or instruments are noticeable.
It should be borne in mind that the pain in the “causal” tooth due to the release of exudate (liquid released into the tissue or cavity of the body from small blood vessels during inflammation) beyond the periodontal gap subsides to a certain extent, but slight mobility of the tooth appears. This circumstance sometimes serves as a justification for delaying visiting a doctor and as a cause of aggravated course of the inflammatory process in the future.
The diagnosis of “acute purulent periostitis” is an absolute indication for surgical intervention in the form of opening and drainage of the periosteal purulent focus and removal of the “causal” tooth.
Options for non-drug treatment (physiotherapy) depend on the patient’s general condition, age, and concomitant chronic diseases. In the latter case, the volume and nature of drug treatment is determined by the dentist of the appropriate profile. It is especially important to carry out adequate treatment in patients suffering from rheumomyocarditis, diabetes mellitus, nephritis and some other chronic diseases.
Another complication of chronic granulating periodontitis is the development of acute odontogenic osteomyelitis , accompanied by the formation of phlegmons and abscesses of the cellular spaces of the face and neck.
These complications of flux are the most severe and dangerous result of the progression of odontogenic infection, and depending on the location and nature of the microflora, they can lead to severe complications including the development of sinus thrombosis and mediastinitis.
It is their timely diagnosis in somatic patients that largely determines the outcome of the disease.
The clinical manifestations of phlegmon are different and depend on the location of the flux (deep, superficial), the nature of the pathogen (aerobic, anaerobic flora), body resistance, concomitant diseases, age, etc.
Today, persistent, sluggish chronic necrotic processes in the bone and soft tissues of the face often occur against the background of drug addiction.
Deep phlegmons of the pterygomaxillary, infratemporal, peripharyngeal spaces are manifested by sharp pain of the corresponding localization, severe manifestations of general intoxication up to acute intoxication psychosis, severe inflammatory contracture of the masticatory muscles, pain when swallowing, with an almost complete absence of external manifestations: hyperemia, infiltration, fluctuations, etc. .
Underestimation of certain symptoms of gumboil can lead to a delay in seeking dental care, ineffective therapy and progression of the inflammatory process.
Why does a white coating appear after extraction?
If white plaque appears after tooth extraction, this is normal. Dentists call it fibrinous plaque. It is the result of trauma and necrosis of the gums. No action needs to be taken. New cells that promote healing soon form under the necrotic tissue.
If the gums are swollen after tooth extraction, and soon loose white tissue appears, this is a sign of recovery. Doctors do not recommend removing the crust. It serves as protection for the injured area and usually resolves on its own.
Other reasons
Everything described above can be attributed to natural causes of swelling. It occurs even if the person is healthy and the tooth is removed correctly. But there are several additional causes of swelling that are also worth keeping in mind. These include:
- Tooth extraction from a patient who has already developed a strong gumboil for some reason.
- Difficulty in removal is especially common in the case of wisdom teeth.
- Infection in soft tissues for any reason.
- Individual intolerance, allergies to medications used during surgery.
- Incorrect tooth extraction, medical error.
- Concomitant chronic diseases, such as neuralgia or hypertension.
When a patient does not follow the doctor’s recommendations regarding maintaining a proper diet and careful oral hygiene, the likelihood of a complication becoming many times higher.
Main rules after surgery
Do not touch the wound
. After the operation has been performed, the body does most of the work itself, so it rarely requires outside intervention.
After removal, a blood clot forms at the wound site. It is very important to keep it in place, so you should take extra care when eating and other activities that involve the oral cavity. Main restrictions
.
You should not consume food or liquid for 4 hours after the procedure. For several days after the operation, it is important to be careful when eating, avoid alcohol and smoking, and do not eat too spicy, sweet or salty foods. It is also very important to maintain a comfortable temperature and not drink or eat anything too hot or cold. Compress
: Swelling of the cheek and gums is significantly reduced if applied to the cheek for a few minutes every half hour.
This convenient and simple remedy helps not only relieve swelling, but also relieve pain. It only helps during the first three days. In the following days, this translates into contraindications. Following the recommendations of a specialist
. If the doctor recommended certain medications, then you need to take them only in the prescribed amount and when the doctor said. There is no need to self-medicate.
The main causes of swelling
When a tooth is removed from the gum, an inflammatory process always occurs. It is for this reason that swelling usually appears, and with it a visible swelling of the cheek on the side of the extracted tooth.
It is important that the removal operation is performed by a dentist with extensive experience, and that the patient strictly follows the recommendations. This will prevent infection from entering the wound. When everything is in order, the inflammatory process gradually fades away on its own. At the same time, the pain decreases and the swelling also decreases.
The timing of swelling depends on many parameters:
- Individual physical characteristics of the patient.
- Removal method.
- Type of tooth removed.
- General condition of the oral cavity.
If the procedure was performed correctly, the patient has a strong immune system and there are no serious diseases, the swelling lasts up to four days. Sometimes this condition can last longer - up to one week.
Concerns begin to arise if more than 7 days have passed, and swelling is still noticeable on the cheek next to the extracted tooth. In this case, you need to contact the dentist again. He will conduct an inspection and evaluate the causes of the problem.
You shouldn’t wait for swelling to appear right away. It usually occurs after the anesthesia wears off. In this case, pain also begins to appear. To remove it, simply use the analgesics recommended by your doctor.
A special case is the removal of a wisdom tooth. In this case, the operation is more complicated and damages the gums more. Often the doctor has to apply a suture to speed up the recovery process. You should be prepared for the fact that the swelling in this case will be longer.
In addition, swelling is accompanied by fever and general weakness. During the recovery period, some patients notice difficulty swallowing and trying to articulate speech.
Sometimes after wisdom tooth removal, doctors may prescribe not only analgesics, but also some antibiotics. This allows you to prevent the development of an infectious process. But taking something without a prescription is strictly not recommended.