Viruses are around us. Some of them suddenly appear and paralyze the normal life of the entire planet, others have been known for a long time, exist everywhere, often even are in the human body, but do not manifest themselves. The second option is the herpes virus.
Currently, 8 types are known, and the human body reacts differently to each of them. Some cause shingles or chickenpox, and only the first two appear less severely, most often just as “blisters” on the lips [1].
This disease was mentioned in literary works and historical documents 2000 years ago. But it was only in the 40s of the last century that the human herpes simplex virus was discovered, studied and described.
WHO indicates that in 2012, the number of people infected with the first type of virus alone was about 3.7 billion. At that time, 67% of the world's population was infected with it. The spread of this virus is trending to increase. Many people carry herpes and don't even know it [2].
Another problem is the high infection rate of the healthy population, mainly young, working age.
In the world, from 16 to 800 people are infected annually, and in Russia from 40 to 80 people per 100 thousand population “Features of herpes viruses” Ph.D. Peradze Kh. D., Ph.D. Sukhoruk A. A.
Types of herpes simplex virus and their features
If we talk about such a manifestation of herpes as a “cold” on the lips, then it is caused by the first two types of virus: HSV-1 and HSV-2. They are very contagious and contribute to the appearance of small bubbles - vesicles - on the mucous membranes. The favorite site of manifestation of HSV-1 is the oral cavity, and HSV-2 usually affects areas in the genital area.
Herpes disease does not always appear only on the lips or genitals. Other areas of the body may also be affected: fingertips, cornea, skin, internal organs and systems, even the spinal cord and brain.
Signs of the presence of herpes virus in the body
Anyone who has ever encountered such a problem knows how herpes manifests itself. Typically, herpes on the lips occurs in several stages and is accompanied by unpleasant symptoms.
- Itching and tingling . A few days before the herpetic rash appears, itching, burning or tingling in the lips may occur.
- Bubble formation . Small bubbles filled with clear liquid usually form at the border of the red border of the lips and the skin around the mouth. Herpes can also be located near the nose, ears or on the cheeks.
- Crusts and weeping . The vesicles burst, the liquid pours out, and shallow open wounds remain on the mucous membrane of the lips, which eventually become covered with a crust.
Most often, this is how the body reacts to the reappearance of symptoms, when the immune system has already developed an algorithm for how to get rid of herpes. The first manifestation of herpes on the lips can be more complicated and be accompanied by additional symptoms:
- fever;
- ulcers on the gums;
- sore throat;
- headache;
- muscle pain;
- enlarged lymph nodes.
Folk remedies
Folk remedies for fighting the virus are considered the most accessible and easiest to use, but in each case their effectiveness can be different - it always helps one person quickly, while on another it acts “like a poultice on a dead person.” It should be noted that natural folk remedies do not cause side effects, and therefore can be used to treat pregnant women and children.
Natural oils - fir, sea buckthorn, rosehip, tea tree. As soon as the first symptoms of “fever” on the lips begin to appear, you should immediately lubricate the area with oil and repeat the procedure every hour or two. This way you can avoid bubbles altogether. Of course, Siberian fir oil does not taste very pleasant and burns a little, but it is better to endure it right away than to walk around with a wound on your lip for a week, or even two. Apply oils in a circular motion, moving from the outer boundaries of the inflammation to the center.
Sea buckthorn oil is considered one of the relatively effective folk remedies.
Also, at the first signs, use Kalanchoe and aloe juices. Simply break off a leaf and gently brush the juice onto your lip.
Garlic, the most famous natural antiviral agent, significantly reduces the symptoms of colds. Having crushed the clove well, add a coffee spoon of honey and a dessert spoon of rich sour cream so as not to get burned when you apply the mixture to the inflamed area.
The affected part of the skin can be gently wiped with chamomile or celandine decoctions.
Laboratory diagnosis of herpes
The insidiousness of this virus is that there are no signs of herpes for a long time. A person may not be aware of his infection until the first vesicle appears on the lips.
But it is quite easy to detect it in a laboratory. For this, the PCR (polymerase chain reaction) method is used, which detects even a small amount of viral particles in biological material. It is suitable for early diagnosis, as it allows diagnosing the disease regardless of the timing of infection, even when the body has not developed an immune response [3].
If you examine antibodies, the enzyme-linked immunosorbent assay (ELISA) is considered the most reliable. The body of the infected person begins to produce protective immunoglobulins G and M. IgM antibodies appear immediately after infection, and IgG antibodies are formed only after the first relapse.
Tests establish the presence of the virus and determine which of the two types it belongs to [4, 5].
Fever in pediatric practice
Fever is an increase in body temperature above normal daily fluctuations (during the day the fluctuation in body temperature is 0.5–1 °C in a healthy person), which accompanies most infectious and some non-infectious diseases. The development of fever is associated with pyrogens - substances that enter the human body from the outside, as well as those formed inside it. Exogenous pyrogens most often represent components of infectious pathogens (lipopolysaccharides, superantigens, peptidoglycans, muramyl dipeptides of the cell walls of gram-positive and gram-negative bacteria, etc.). Exogenous pyrogens act indirectly through endogenous pyrogens - proinflammatory cytokines (interleukin-1β, interleukin-6, tumor necrosis factor-α, interferon-α), which are produced by macrophages, monocytes, dendritic, endothelial, epithelial cells (Fig.). This leads to the formation of prostaglandin E2 (PGE2), which activates thermoregulatory neurons with a shift in the set point in the thermoregulatory center of the anterior hypothalamus, so normal body temperature is perceived as decreased and heat production begins to prevail over heat loss [1].
Fever (temperature 38 °C and above) as a component of the body's inflammatory response to infection is largely protective in nature, while hyperthermic syndrome (temperature 40 °C and above) is a pathological variant of fever and is accompanied by a rapid and inadequate increase in body temperature, with impaired microcirculation , metabolic disorders and progressively increasing dysfunction of vital body systems.
Clinicians define fever as an increase in body temperature by more than 1 °C compared to the average normal temperature at a given point of its measurement.
A child’s normal body temperature fluctuates during the day within the range of 0.5–1.0 °C with an increase in the evening hours. When measured in the axilla, normal body temperature ranges from 36.5 to 37.5 °C, with maximum rectal temperature reaching an average of 37.6 °C, exceeding 37.8 °C in half of the children. The criteria for fever should be considered: rectal temperature more than 37.9 °C, oral temperature more than 37.5 °C, axillary temperature more than 37.3 °C, tympanic temperature above 37.5 °C.
Fever is accompanied by a number of subjective sensations: chills, headache, anorexia, drowsiness, thirst, oliguria, but in children they are usually mild or absent. An increase in temperature for every 1 °C is accompanied by an increase in respiratory rate by 2-3 per minute and pulse by 10 beats per minute.
There are “pink” and “white” fevers. “Pink” fever reflects the correspondence of heat production to heat transfer; with it, the skin is pink, hot, and moist to the touch, and the child behaves normally. With “white” fever, the skin is pale, with some cyanosis and/or a marbled pattern, “goose bumps”, acrocyanosis, and coldness of the extremities often appear. A decrease in heat transfer at the onset of the disease may indicate a process of “warming up” to a new high set point, usually accompanied by chills. It should be remembered that a similar picture may indicate centralization of blood circulation, disruption of microcirculation and blood rheology.
The combination of fever with individual clinical symptoms in infectious and somatic diseases is presented in Table. 1.
In approximately 20% of cases, children aged 0 to 36 months experience fever without an obvious focus of infection (LFIO) - a temperature above 38 ° C, the duration of the fever is no more than 7 days, the history and physical examination do not allow identifying the cause of the fever [2, 3]. In case of LBIO, diseases such as urinary tract infection, bacterial and aseptic meningitis, osteomyelitis, latent bacteremia (Str. pneumoniae, Staph. aureus, H. influenzae, E. coli, Salmonella spp., Listeria monocytogenes), pneumonia, gastrointestinal infections should be excluded. -intestinal tract [4]. In addition to early age, complement deficiency, abnormalities of opsonization and phagocytosis, and severe combined immunodeficiency predispose to LBIO.
When assessing the severity of intoxication in a child with LBIO, it is necessary to pay attention to: the child’s activity; reaction to the environment, parents; anxiety not related to external circumstances; nature of screaming, crying; skin color; state of hydration. Laboratory and instrumental studies for LBIO include:
- detailed blood test with assessment of leukocyte formula, erythrocyte sedimentation rate;
- morphological changes in peripheral blood neutrophils;
- Analysis of urine;
- determination of microbial number in urine;
- lumbar puncture with examination of cerebrospinal fluid;
- microscopy of blood and cerebrospinal fluid for the presence of gram-positive or gram-negative flora;
- bacteriological culture of blood, cerebrospinal fluid, urine, feces;
- coprogram;
- determination of the level of C-reactive protein;
- chest x-ray.
It must be remembered that fever in a child in the first three months of life is an indication for emergency hospitalization, followed by the above studies and the prescription of parenteral antibiotic therapy [5].
In 1961, BP Beeson and RT Petersdorf defined the concept of “fever of unknown origin” (ICD-10 R50) - body temperature above 38.3 ° C for more than 3 weeks, the cause of which could not be determined after 1 week of intensive examination [6] . In approximately 30–40% of cases, fever of unknown origin (FUO) is caused by infectious agents, 10–20% of cases are due to collagenosis, 10% are malignant neoplasms, 5–10% are inflammatory bowel diseases, in 1/3 of cases the cause of FUO cannot be determined succeeds and the process resolves spontaneously [7, 8]. Possible causes of LDL (nosological forms) are presented below:
- Pontiac fever;
- extrapulmonary tuberculosis;
- brucellosis;
- Lyme disease;
- AIDS virus;
- parasitic diseases (leishmaniasis, trypanosomiasis);
- fungal diseases (aspergillosis, blastomycosis, cryptococcosis, pneumocystosis);
- solid tumors;
- histiocytosis;
- systemic connective tissue diseases;
- vasculitis;
- subacute thyroiditis;
- Crohn's disease;
- nonspecific ulcerative colitis;
- celiac disease;
- thrombophlebitis;
- osteomyelitis;
- drug fever (β-lactam antibiotics, sulfonamides, metoclopramide, benzodiazepines, phenytoin, phenothiazines, azathioprine).
To determine the cause of LDL, in addition to the above studies for LBIO, the following are recommended:
- study of blood serum and cerebrospinal fluid using enzyme immunoassay and polymerase chain reaction for viral, bacterial, fungal and parasitic pathogens;
- determination of the level of antinuclear and antineutrophil antibodies, rheumatoid factor;
- study of the level of thyroid-stimulating hormone, T3, T4, antibodies to thyroid peroxidase;
- Mantoux reaction, Diaskintest;
- ultrasound examination of the abdominal organs, heart, lungs, thyroid gland;
- magnetic resonance imaging of the brain and spinal cord;
- multislice computed tomography of the chest and abdominal cavity;
- fibrocolonoscopy.
Fever is not an absolute indication for lowering the temperature. Taking antipyretic drugs at a temperature of 38 °C and above is indicated for: children in the first three months of life; children with a history of febrile seizures; for severe heart and lung diseases; for organic diseases of the central nervous system; children with hereditary metabolic diseases [9].
Previously, “healthy” children were given antipyretic drugs at temperatures of 39 °C and above [10].
The World Health Organization recommends only two drugs as antipyretic therapy in children: paracetamol and ibuprofen [11]. The main characteristics of these drugs are presented in table. 2.
A 2010 meta-analysis of 85 randomized trials showed that ibuprofen, compared to paracetamol, is more effective for fever and pain in children and adults, and the study also confirmed the high safety profile of these drugs [12].
In a study by AM Magni et al. (80 children aged 6 months to 8 years) showed a more pronounced antipyretic effect of ibuprofen at a dose of 10 mg/kg than that of metamizole sodium at a dose of 15 mg/kg. The benefit of ibuprofen was especially pronounced in children with high (> 39.1 °C) body temperature [13]. It is also interesting that ibuprofen is better at reducing high body temperature (> 39.2 °C) than paracetamol in children aged 2 to 11 years [14].
Thus, ibuprofen (Nurofen® for children) is the drug of choice for conditions that require a complex antipyretic, analgesic and anti-inflammatory effect: influenza; enteroviral fever, enteroviral vesicular pharyngitis, enteroviral vesicular stomatitis with exanthema; scarlet fever; Infectious mononucleosis; extraintestinal yersiniosis; acute otitis media, tonsillitis, pharyngitis; teething syndrome and acute toothache; prevention of fever in the post-vaccination period; diseases accompanied by chronic inflammation [15–18]. Ibuprofen (Nurofen® for children) should not be used for more than 3 days as an antipyretic, or for more than 5 days as an analgesic drug for acute illnesses in children.
One of the forms of release of ibuprofen (Nurofen® for children) is suppositories, designed specifically for children in the first two years of life, when oral administration of medications is difficult (in case of vomiting and regurgitation in a child, refusal to take oral forms).
Rotating antipyretic medications to treat fever in children is an old and common practice. However, the combination of paracetamol and ibuprofen can be considered as a possible risk factor for the development of additional adverse events (acute renal failure, toxic hepatitis, gastric bleeding) compared with the use of each drug separately [19].
Uncontrolled use of antipyretic drugs, especially “course” ones, creates the illusion of well-being and causes the belated prescription of etiotropic drugs.
The use of Aspirin, nimesulide, and Analgin tablets to reduce fever in childhood is contraindicated!
Thus, in pediatric practice, paracetamol and ibuprofen (Nurofen® for children) are indicated as antipyretic therapy in accordance with their high safety profile. For diseases accompanied by fever, pain, and severe inflammation, it is advisable to prescribe ibuprofen (Nurofen® for children).
Literature
- Dalal S., Zhukovsky DS Pathophysiology and management of fever // J Support Oncol. 2006; 4:9–16.
- Wittler RR, Cain KK, Bass JW A survey about management of febrile children without source by primary care physicians // Pediatr Infect Dis J. 1998; 17 (4): 271–277.
- American College of Emergency Physicians Clinical Policies Committee; American College of Emergency Physicians Clinical Policies Subcommittee on Pediatric Fever. Clinical policy for children younger than three years presenting to the emergency department with fever // Ann Emerg Med. 2003; 42:530–545.
- Ishimine P. Fever without source in children 0 to 36 months of age // Pediatr Clin N Am. 2006; 53: 167–194.
- Infants and children: acute management of fever second edition (clinical practice guidelines). NSW HealtH, 2010. 20 r.
- Petersdorf RG, Beeson PB Fever of unexplained origin: report of 100 cases // Medicine. 1961; 40:1–30.
- Tezer H., Ceyhan M., Kara A. et al. Fever of unknown origin in children: the experience of one center in Turkey // The Turkish Journal of Pediatrics. 2012; 54:583–589.
- Shi Xiao-chun, Liu Xiao-qing, Zhou Bao-tong et al. Major causes of fever of unknown origin at Peking Union Medical College Hospital in the past 26 years // Chin Med J. 2013; 126(5):808–812.
- Tatochenko V.K., Uchaikin V.F. Fever // Pediatric pharmacology. 2006; 3:43–44.
- Baranov A. A. Feverish syndromes in children. M.: Union of Pediatricians of Russia, 2011. 228 p.
- The management of fever in young children with acute respiratory infections in developing countries. WHO. Geneva, 1993.
- Pierce CA, Voss B. Efficacy and safety of ibuprofen and acetaminophen in children and adults: a meta-analysis and qualitative review // Ann Pharmacother. 2010; 44(3):489–506.
- Magni AM, Scheffer DK, Bruniera P. Antipyretic effect of ibuprofen and dipyrone in febrile children//J. Pediatr. (Rio J). 2011; 87(1):36–42.
- Walson PD, Galletta G., Braden NJ, Alexander L. Ibuprofen, acetaminophen, and placebo treatment of febrile children//Clin. Pharmacol. Ther. 1989; 46(1):9–17.
For a complete list of references, please contact the editor.
Yu. B. Belan1, Doctor of Medical Sciences, Professor M. V. Starikovich, Candidate of Medical Sciences
State Budgetary Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation, Omsk
1 Contact information
Methods of infection
There are several main ways of contracting a herpes infection.
Straight way
The virus passes to a healthy person from a sick person through direct contact. A prerequisite for transmission is the active skin manifestation of the herpes virus on the lips or other parts of the body. This route of transmission is possible through kissing (herpes on the lips), sexual contact (genital herpes), through hands, when the virus is actively released from herpetic vesicles.
Indirect transmission route
In this case, infection occurs through personal hygiene items, dishes, and cosmetics from a person with herpes at the stage of spreading the virus. For prevention, it is enough to use individual personal hygiene items - a toothbrush, comb, cosmetics - lipstick, creams, cosmetic pencils [2, 6].
Prevention
Since the herpes virus is very common throughout the world, it is almost impossible to avoid infection, but we can make sure that the immune system successfully resists it:
- Always practice good personal hygiene
- Use personal hygiene products: towels, linen, dishes
- Try to touch your face less
- Strengthen your immune system - drink decoctions of rose hips, St. John's wort, mint tea, eat more fruits and vegetables, take vitamin complexes in winter and spring
- If you have a small child and you catch a fever, do not kiss him, wear a cotton-gauze bandage and do not touch the baby without gloves
- Walk a lot, but avoid hypothermia and overheating
- Try to avoid stress and don't take things too seriously
- Get rid of bad habits, as they greatly weaken the body.
- If you are sick or have a cold, get treatment and help your immune system
This is usually enough to minimize the risk of relapse. I hope these tips will help you prevent the appearance of “fever” on your lips, which so spoils your beauty and, accordingly, your mood. Be healthy!
Risk factors for colds on the lips
Once infected, the virus remains in the human body forever. An effective treatment for herpes has not yet been invented to help eliminate it from the body. However, you can try to reduce the frequency of herpes on the lips if you avoid the causes of virus activation. Frequent herpes on the lips can be caused by:
- stress;
- fatigue;
- systemic diseases, ARVI;
- hormonal changes;
- allergies;
- exposure to the sun or local hypothermia [7].
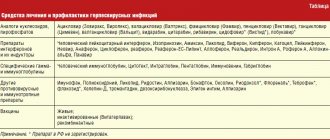
Treatment methods for herpes
Currently, doctors' recommendations on how to treat herpes are limited to a regimen that helps to quickly get rid of the manifestations of herpes on the lip, other part of the body, or helps prevent the onset of the active phase of the disease.
Sometimes local antiviral drugs are sufficient for therapy. Ointments and creams that help against herpes contain one of the following components:
- acyclovir;
- valacyclovir;
- pharmaciclovir;
- penciclovir.
These active ingredients are produced under different brands, and all are aimed at effectively treating the manifestations of herpes.
If local treatment of herpes on the lips is ineffective, it is recommended to take tablet medications that suppress the replication of viruses in cells. They are believed to be more effective. In special cases, with large affected areas, when internal organs and systems are affected, complex treatment in a hospital is possible [3, 4, 8].
Ointments for herpes
In winter and spring, when we especially lack vitamins, and there are many sores “walking” on the street, we must always have with us a remedy that can destroy the beginning manifestations of fever on the lips.
There are many drugs that speed up healing and reduce the symptoms of a “cold”, even if they are already visible, but our goal is to prevent them from occurring. For this, ointments, creams and gels are best suited, which should always be in your home medicine cabinet.
Thanks to the targeted effect on the source of inflammation, the ointment or gel quickly suppresses the activity of herpes, supports and restores the skin that has been attacked, it is simple and easy to use - just apply it in time and repeat the procedure several times a day to prevent the infection from developing.
Plant extracts and acyclovir prevent the multiplication of the virus, enhance skin protection, and help to recover faster. Unlike tablets, gels, creams and ointments practically do not cause allergies and do not affect internal organs, since they are used exclusively at the site of the lesion.
The most popular ointments are Acyclovir, Zovirax and Panavir. The first two and all their variations are made on the basis of acyclovir, a substance that blocks the reproduction of herpes. Various auxiliary components (propylene glycol, petroleum jelly) help relieve pain due to the rapid absorption of the active ingredients. Such drugs are contraindicated for pregnant, lactating women and people with individual intolerance.
If you start therapy on time, you can prevent the development of the virus
The most natural of the antiherpetic pharmaceutical products is Panavir gel (extract from potato shoots).
Prevention of infection and manifestations of the disease
It is not always possible to quickly get rid of herpes on the lips if it has entered the active stage, but you can strive to prevent the spread of the virus and minimize its manifestation.
Prevention of herpes consists of following basic sanitary and hygienic recommendations:
- keep your hands clean;
- use personal hygiene items;
- Avoid skin-to-skin contact with people with active disease.
If exacerbations occur frequently, this is a signal that the immune system needs help: it may be necessary to take a long-term antiviral drug as prescribed by a doctor [2, 9]. If the onset of the disease is provoked by sunlight or low temperatures, it is advisable to use special protective creams on the lip area and the skin around them.
Only a qualified doctor knows how to cure herpes in each specific case. But on your own, you can prevent further spread of the viral infection and reduce the number of relapses.
Medical expert: Oleg Sergeevich Shchekin
Last updated: July 21, 2022
List of sources
- Peradze Kh. D., Sukhoruk A. A. Features of herpes viruses. // URL: https://cyberleninka.ru/article/n/osobennosti-gerpes-virusov (date of access: 04/09/2020).
- WHO fact sheet. Herpes simplex virus. // URL: https://www.who.int/ru/news-room/fact-sheets/detail/herpes-simplex-virus (access date: 04/09/2020).
- Vasiliev A. N., Fedorova N. E., Klimova R. R., Adieva A. A. Improving the diagnosis of herpesvirus infections. // URL: https://cyberleninka.ru/article/n/sovershenstvovanie-diagnostiki-gerpes-virusnyh-infektsiy (date of access: 04/09/2020).
- Kazmirchuk V. E. Clinic, diagnosis and treatment of human herpesvirus infections: monograph / V. E. Kazmirchuk, D. V. Maltsev - K.: Phoenix, 2009 - 248 p.
- Kharlamova F. S., Egorova N. Yu., Guseva L. N., Guseva N. A., Novosad E. V. Viruses of the herpes family and immunity. // URL: https://cyberleninka.ru/article/n/virusy-semeystva-gerpesa-i-immunitet (date of access: 04/09/2020).
- Isakov V. A., Arkhipova E. I., Isakov D. V. Human herpesvirus infections: a guide for doctors. – St. Petersburg: SpetsLit, 2013 – 670 p.
- Lutsenko M. T., Gorikov I. N. Some information about the morphology of herpes viruses and their properties. // URL: https://cyberleninka.ru/article/n/nekotorye-svedeniya-o-morfologii-gerpes-virusov-i-ih-svoystvah (date of access: 04/09/2020).
- Zuikova I. N., Shulzhenko A. E., Kuzmin V. N. Recurrent herpes. A new approach to treatment. // URL: https://cyberleninka.ru/article/n/retsidiviruyuschiy-gerpes-novyy-podhod-k-lecheniyu (date of access: 04/09/2020).
- Kalinina N. M., Davydova N. I. The role of immunotropic therapy in increasing the effectiveness of treatment of herpesvirus infections. // Terra Medica. – 2009 – No. 1(56). – P.17-22.