Vincent's ulcerative necrotizing stomatitis
One of the reasons that the tongue hurts on the side is Vincent's ulcerative necrotizing stomatitis. With this disease, ulcers appear in the oral cavity, which can be located not only directly on the tongue, but also on the mucous membrane of the cheeks, and even spread further:
- on the gums;
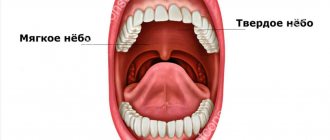
- sky;
- tonsils.
The disease is caused by bacteria: spirochetes and fusobacteria. What is especially characteristic of this pathology is that the ulcers are covered with a dirty gray coating. Vincent's ulcerative-necrotizing stomatitis is treated locally with antimicrobial drugs. Broad-spectrum antibiotics are also prescribed.
Prevention
Glossitis is easier to prevent than to treat. In order to avoid this unpleasant disease you need to follow simple rules.
The first is oral hygiene. This principle applies to both children and adults. If you wash your hands before eating, brush your teeth regularly, do not use someone else’s toothbrushes, and regularly sanitize your mouth, then the risk of developing tongue inflammation is minimal.
Try to avoid damaging the mucous membrane. Avoid eating hard foods that can damage your tongue, such as chips. Hot foods also cause epithelial defects. Spicy foods have an irritating effect. Abuse of them significantly worsens the condition of the tongue mucosa and increases the risk of infection.
Nicotine not only irritates the mucous membrane, but also impairs microcirculation, which reduces the resistance of the epithelium to the effects of infectious agents. Inflammatory diseases of the oral cavity are more common in smokers than in patients who are not adherents of this addiction. Strong alcoholic drinks also have a negative effect on the mucous membranes.
If you have symptoms of glossitis, do not self-medicate, contact a dental clinic. A competent specialist will determine the cause of the disease and prescribe treatment that will help quickly get rid of unpleasant symptoms. Remember, if glossitis is not treated, the disease can lead to serious complications and irreversible consequences.
Tongue injuries
Another reason why the tongue hurts on the side lies in mechanical injuries to the organ. They occur when eating food with sharp parts (seeds, nuts, undercooked cereals), hitting, or biting. Damage can occur due to a seizure, sports, falls, or various accidents.
If you are absolutely sure that the soreness is the result of an injury, then you just need to give the tongue time to recover. Nevertheless, examination by a specialist to clarify the diagnosis and treatment will not be superfluous.
Pain and burning of the tongue: how to treat?
Probably every gastroenterologist in his practice has encountered a patient with complaints of pain or burning of the tongue. Turning to this specialist in the first place is probably due to the following logical chain: the tongue is in the oral cavity, where the digestion process begins, which means that if a problem arises, you should visit a gastroenterologist. Old publications also come to the aid of patients and doctors of other specialties, in which chronic diseases of the digestive organs were considered as the causes of burning tongue.
But is it really that simple? Is pain and burning of the tongue a separate disease and who should treat it?
A little history and terminology.
Pain/burning in the tongue has many synonyms: glossalgia, glossodynia, stomatodynia, glossopyrosis, oral paresthesia, neurogenic glossitis, tongue neurosis, glossalgic syndrome. This condition is traditionally part of the so-called burning mouth syndrome or “burnt mouth syndrome,” in which pain/burning sensations are localized in various areas: tongue, upper palate, gums, lower lip, pharynx.
Burnt mouth syndrome (SMS) was first described back in 1880; in the 20th century, the term glossodynia, i.e., appeared. pain in the tongue, since unpleasant symptoms from the tongue were most common. This syndrome was first identified as a separate disease in 2004.
Almost all existing review articles and recommendations consider glossodynia within the framework of the SOP. General recommendations for the diagnosis and treatment of ROP may be applicable to the special case of glossodynia.
Definition
The International Association for the Study of Pain has designated glossodynia and oral burning as chronic pain, specifically “burning pain of the tongue or other mucous membranes of the mouth.”
Later, a detailed definition was given for ORS: “a burning sensation or sensation of altered sensitivity in the oral cavity, repeated daily for more than 2 hours a day for more than 3 months, without obvious causative lesions on clinical examination and examination.”
Epidemiology
Data on the prevalence of ROP and tongue pain/burning separately still vary from study to study. The average incidence of all cases of oral burning (including but not limited to tongue burning) is 0.1-3.7% of the population. Women suffer from this syndrome 2.5-7 times more often than men, especially often over the age of 60 and after menopause.
Common causes of pain and burning in the mouth.
There are two groups of reasons why patients notice a burning sensation in the mouth:
1) Primary (idiopathic), when there are no diseases of the oral cavity and other organs and systems, this will be the true SOR.
2) Secondary, caused by local (localized in the oral cavity) and systemic causes (autoimmune diseases, deficiency conditions, etc.)
Causes of secondary burning sensation in the mouth/burning tongue.
Possible causes of secondary burning sensation in the oral cavity are diverse and, oddly enough, are rarely associated with pathology of the digestive organs. A review published in 2022 on this problem identified the following conditions and diseases responsible for the occurrence of burning sensation in the mouth:
Local factors:
A. Diseases, conditions and damage to the oral cavity:
- fungal infection (eg candidiasis)
- lichen planus
- pemphigoid
- pemphigus
B. Trauma
1) Mechanical
2) Chemical
A. From the patient's side:
- toothpastes with abrasives
- use of mouth rinses with ethyl alcohol
- medications such as aspirin (applied to the sore tooth); over-the-counter medications containing phenols, peroxide, sulfuric acid
- vitamin C (citrus fruits)
- sour drinks
- lozenges and cough suppressants with high menthol content
b. From the dentist:
- Irrigation of the oral cavity with solutions containing methyl methacrylate, formaldehyde, formocresol, sodium hypochloride
- acrylic resin
- eugenol
3) Thermal: spicy or hot food or drink
C. Parafunctional habits
- Tongue sticking out, cheek biting, excessive tongue brushing
- mouth breathing
D. Xerostomia or impaired quality/quantity of saliva
- consequences of radiation or chemotherapy, Sjogren's syndrome, pathology of the salivary glands
- side effects of medications (antihistamines, antidepressants, diuretics, steroid hormones, non-steroidal anti-inflammatory drugs, amphetamines)
- smoking
E. Allergic reaction/contact hypersensitivity
- products, additives, flavors
- colorings and flavors from oral care products
- dental materials (nickel sulfate, cobalt, zinc)
System factors
A. Deficiency conditions: decreased levels of iron, zinc, folic acid, vitamins B1, B2, B6, B12
B. Endocrine pathology
- diabetes
- hypothyroidism
- hormonal disorders (changes in cortisol/sex hormone levels)
C. Autoimmune diseases
- Sjögren's syndrome
- lichenoid reactions
- systemic lupus erythematosus
D. Other diseases
- gastroesophageal reflux disease
- celiac disease
- multiple sclerosis
- Parkinson's disease
- Fabry disease
E. Medicines
- angiotensin-converting factor inhibitors
- antiretroviral therapy
F. Peripheral and central neuropathies
- diabetic polyneuropathy, neuropathy due to renal failure, neuropathy due to systemic connective tissue diseases, neuropathy due to HIV infection, postherpetic neuropathy, neuropathy due to chemotherapy
As can be seen from this huge list, most cases of burning of the tongue and in the oral cavity in general are caused by a dental problem/pathology, neurological, endocrine and autoimmune diseases. Gastroenterological causes (for example, gastroesophageal reflux disease) are rather the exception to the rule.
Primary burning sensation in the oral cavity (BOR) and its causes.
If there are no indications of secondary causes of burning in the oral cavity, most likely there is a true SOR. This is an independent disease, the cause of which is still unclear. In its development, the role of psychological factors and mental disorders, changes in the nerve endings and conductive nerve fibers of the oral cavity, as well as the central nervous system is assumed.
Clinical manifestations of ROP.
Symptoms that may bother patients with ROP are:
1) Pain and/or burning in the mouth of varying intensity. Some patients describe these sensations as tingling or irritation, as well as impaired sensitivity. The pain often occurs spontaneously, is often symmetrical and does not necessarily affect only one area. In the case of glossodynia, pain/burning is most often localized in the anterior 2/3 of the tongue, on its back, and lateral surfaces. The pain is minimal in the morning immediately after waking up, increasing in intensity throughout the day. Eating spicy, hot foods and drinks, as well as stress and fatigue increase the pain/burning sensation.
2) More than 70% of patients, in addition to pain/burning, note changes in taste, a decrease in its intensity, as well as the appearance of a foreign taste (bitter, metallic, or a combination of both). Most often, the sensation of sweet and salty tastes is reduced, and sour tastes are perceived more intensely.
3) Dry mouth (xerostomia) is noted by 46-67% of patients with SOP, while according to research data, an objective decrease in the amount of saliva is not observed in them.
4) Association with burning/pain from other mucous membranes has also been described in patients suffering from ROP. Most often this is a burning sensation in the rectum and genital tract. An alternative may be a feeling of dry mucous membranes (eyes, genital tract in women)
5) Night sleep disturbances are common (in 80% of cases) in people with SRS
6) Anxiety and depression are frequent companions of SOR and glossodynia separately. A meta-analysis of clinical studies showed that anxiety conditions increase the risk of developing RAS by 2.6 times, and depression by 3.2 times. Cancerophobia, social phobia, neuroticism, etc. are also often noted.
7) ODS is characterized by an association with other diseases that manifest as chronic pain: fibromyalgia, chronic back pain, chronic pelvic pain, irritable bowel syndrome, etc.
Treatment of SOR.
1) Patient information and support
Many patients with chronic oral burning and pain do not understand why their symptoms persist for so long. An important task of the doctor is to explain to patients with SRS the possible mechanisms of the formation of unpleasant sensations. Patients should be reassured that their symptoms are not imaginary or related to any form of cancer. This support will reduce anxiety, depression, fear and frustration, especially in individuals who have had previous unsuccessful treatment experiences.
2) Local therapy
Local use of clonazepam in the form of mouth rinses showed good results in reducing the severity of pain/burning in the mouth. There is encouraging evidence for the topical use of capsaicin (a chili pepper alkaloid) in low concentrations.
3) Systemic therapy
Tricyclic antidepressants, antidepressants from the group of serotonin and serotonin/norepinephrine reuptake inhibitors, clonazepam, and antiepileptic drugs (pregabalin and gabapentin) are actively used as drugs for the treatment of ORA. The use of alpha-lipoic acid has shown little effectiveness.
4) Non-drug psychotherapy
Given the frequent association of ODS with anxiety disorders, phobias and depression, non-pharmacological psychotherapy is an integral part of the treatment of this problem. Cognitive behavioral therapy, individual and group psychotherapy should be considered as methods of choice.
5) Physiotherapy and alternative treatments
Low-level laser therapy and acupuncture have been studied as methods for reducing pain. These methods were effective in some people with cerebral obstruction, but are not widely used.
Conclusion.
Identifying the causes of pain/burning in the oral cavity is a challenge for doctors of different specialties, but their friendly work allows us to solve the problem and improve the quality of life of patients.
Glossitis
Glossitis
is an inflammation of the tissues of the tongue, manifested in its soreness, changes in color and structure, and the appearance of a dense coating. There is a burning sensation, hyperemia (overflow of blood vessels), food loses its taste, and salivation increases.
If the doctor has diagnosed the patient with glossitis, then the next step is to find out whether this indicates a pathology of other organs. This could be a herpes virus, poisoning with heavy metal salts, etc. Treatment is prescribed depending on the initiating cause, trying to exclude it. It usually includes local antiseptic therapy.
What is in the sublingual area
The tissues located on the lower jaw under the tongue are called the floor of the mouth. Due to the complexity of the structure, as well as the natural functionality of this area, a person often experiences problems accompanied by pain.
Structure of the sublingual region:
- Hyoid muscles - have an elastic structure and are responsible for the motor function of the area;
- Hyoid bone - has an anatomical shape in the form of a horseshoe, located in the muscle layer. It is the only bone in the human body that has no connections with other bones of the body;
- Nerve endings are elements of the peripheral nervous system, responsible for the sensitivity of the sublingual area to various physical, mechanical and thermal stimuli;
- Salivary glands - responsible for the production of saliva, which is involved in the process of wetting the mucous membranes of the oral cavity and the digestion process;
- Blood vessels - provide nutrition to the tissues of the sublingual area;
- Frenules are connecting folds in the sublingual area, responsible for connecting the sublingual tissues with the tongue.
Each of the above elements ensures the natural functionality of the dentofacial apparatus and participates in all physiological processes of the oral cavity.
Catarrhal glossitis
If the tongue hurts on the side and a white coating covers its surface, then this is most likely catarrhal glossitis - a special case of this disease. It can be considered as a symptom of other pathologies. In particular, it is called:
- caries;
- stomatitis;
- gastrointestinal diseases;
- various infections (measles, diphtheria, etc.).
In addition to pain and plaque, symptoms of catarrhal glossitis include swelling of the tongue and a burning sensation, which is especially worse after eating or talking. The disease is treated by eliminating its causes and rinsing the mouth with antiseptic solutions.
Stomatitis: features of the disease
Stomatitis is a disease related to dental pathologies in which inflammation of the oral mucosa occurs. Infection of the tongue with stomatitis in adults is also called “glossitis.”
The inflammatory process affects the mucous membrane and causes severe symptoms:
- redness and swelling of the tongue;
- formation of white plaque;
- severe pain;
- the formation of many small blisters and ulcers.
Due to severe sensitivity and soreness of the tongue, the patient cannot eat food, fever, insomnia and irritability are possible.
Stomatitis under the tongue in adults, as in other parts of the oral cavity, is classified into two types.
- Aphthous. A form of inflammation in which the tongue becomes covered with papules and ulcers that turn into erosions (aphthae).
- Herpetic. The inflammatory process is manifested by swelling and redness of the tongue. Small bubbles are localized in groups.
Prosthetic stomatitis and ulcerative-necrotic form of pathology are extremely rare.
Without treatment, the signs of stomatitis completely disappear, but this does not mean that the patient is cured of the pathology. The inflammatory process becomes chronic and when the immune system is weakened or exposed to an irritant, a relapse occurs.
Inflammation of the salivary glands
This disease is called sialadenitis. Any salivary glands can be affected by it, but painful sensations in the tongue, closer to the base, occur if the sublingual gland is affected. Pathology is caused by viruses or bacteria. Symptoms of sialadenitis include:
- pain at the base of the tongue;
- the formation of a compacted swelling underneath;
- decreased salivation.
How to treat the disease if the tongue hurts on the side precisely for this reason? Antibacterial and antiviral drugs.
First aid
If the tongue or the inside of the cheek is bitten, two problems arise at once:
1. Stop bleeding
solution: rinse your mouth with cold water, if possible, apply ice (cooling helps to constrict blood vessels)
If you cannot stop the bleeding on your own, you must immediately consult a doctor!
2. Pain relief
solution: cold also relieves pain, but if the pain is severe, treat the area with a special “freezing” spray or take a painkiller tablet
What to do
If a patient has a swollen tongue, treatment primarily depends on what causes the swelling. First of all, the cause should be determined; only an experienced doctor can do this. If the cause is known and it is not life-threatening (for example, biting the tongue or being burned by too hot food), then you can try to relieve the unpleasant symptoms yourself. But if the cause of tongue swelling is an allergic reaction, self-medication is life-threatening.
There are many ways to relieve swelling using traditional methods. However, all of them are suitable only for cases where the cause of swelling is microtrauma of the tongue.
You can rinse your mouth with decoctions of medicinal herbs - chamomile, sage, calendula, eucalyptus. You can use baths and rinses made from chlorhexidine, various herbal balms and rinses. If the patient's tongue is swollen after tooth extraction, rinsing with herbal infusions will help. It should be remembered that in this case you should absolutely not rinse your mouth with hot infusion, it will only increase inflammation.