The main cause of cerebrovascular accidents is atherosclerosis of the carotid arteries. Atherosclerotic plaques cause narrowing of the carotid arteries, which is an obstacle to normal blood circulation in the brain. Gradually, a complete blockage of the carotid artery develops, which is called occlusion. Impaired patency of the carotid artery is the main cause of ischemic stroke in the modern world. The risk of developing a stroke if the carotid artery is narrowed symptomatically by 70% or more is about 15% per year.
Many people die or become disabled from stroke every year, although modern vascular surgery can prevent it in most patients. Only regular diagnosis and trust in doctors will significantly reduce the risk of stroke. It is much easier to treat atherosclerosis of the carotid artery than ischemic stroke and its consequences.
General information
Vascular occlusion is a blockage (more often of arteries than veins), which is characterized by a pronounced decrease in the speed and quality of blood flow. Occlusion can cause necrosis and, as a result, lead to death.
The pathology is quite common and can affect the organs of visual perception, the central nervous system, limbs and great vessels. sepsis and peritonitis develop . Abdominal ischemic syndrome develops against the background of a lack of adequate blood circulation in the digestive tract. The pathology is associated with occlusion of the unpaired visceral branches of the abdominal aorta - the celiac trunk and mesenteric arteries (superior, inferior). Abdominal toad can develop under the influence of both internal ( thrombosis ) and external factors (traumatic occlusion).
What is an occlusive dressing?
This method of sealing the lesion is used for wounds that require maintaining sterile conditions and protection from the external environment.
Applying an occlusive dressing to the knee joint requires certain skills and technique:
- cover the wound surface with sterile gauze;
- Place the top of the scarf on the thigh area and wrap it around the waist;
- bend the bandage at the base by 2 cm;
- cross the ends under the thigh, tie knots on the thigh;
- Throw the top over the knot formed and then pass it under the knot.
Consequences of distal occlusion
The patient's appearance is typical. The face is deformed, the lower jaw and chin are light, the upper jaw protrudes forward. A constantly open mouth gives the face a specific expression. Such people have complexes because of their appearance and have difficulty communicating with others.
The anomaly increases the risk of disease of the teeth and soft tissues of the oral cavity. Due to non-closing teeth, the load during chewing is distributed unevenly. Usually, only molars are involved in chewing, which wear out prematurely and are often affected by caries. The temporomandibular joint suffers. Improper loading leads to wear of the articular surfaces, chronic inflammation, and limited range of motion of the lower jaw.
When using prosthetics, people with abnormal bites face difficulties. To correctly install removable dentures and bridges, it is necessary to file down healthy teeth that interfere with the closure of the jaws.
It is better to correct the bite in childhood, without waiting for complications or irreversible disorders.
Pathogenesis
When the blood thickens, there is an accumulation of fibrin in its composition, which leads to thrombus formation . Venous formations are characterized by constancy - they are located in one area and clog the vessels of the extremities, leading to necrosis and gangrene . Arterial formations are characterized by migration; they often break away from the original source and disrupt the blood supply to large organs, provoking the development of stroke , heart attack and other dangerous conditions.
Forecast and preventive recommendations
If the arterial lumen is blocked by half, the disease may occur without obvious signs. With such a picture, the risk of developing apoplexy is 10% of all cases within five years. A 75% vascular blockage leads to a 6% stroke rate in the first year. Complete thrombosis of the canal leads to inevitable neurological damage in 40% of incidents. Preventive surgical intervention with or without prosthetics makes it possible to reduce these risks to a minimum.
To prevent the closure of vascular walls, it is recommended to get rid of bad habits, balance your diet, and monitor weight gain. The lipid composition of the blood is determined by regular testing. If necessary, therapeutic recommendations help adjust the composition of the blood solution. If cardiac abnormalities are present, supportive treatment should be provided promptly. In case of congenital diseases of the cardiovascular system, it is also recommended to undergo regular examination as prescribed by a cardiologist.
Classification, types of occlusion
It is customary to distinguish between arterial and venous occlusion.
Types of occlusion by localization:
- Occlusion of mesenteric vessels . It is characterized by an acute circulatory disorder in the mesenteric vessels, which inevitably leads to intestinal ischemia. As a result of thrombosis, the trophism (nutrition) of the intestinal walls is disrupted, and an acute inflammatory process develops, including peritonitis .
- Occlusion of cerebral vessels. The gradual growth of cholesterol plaques in volume can lead to complete blockage of the vessels supplying blood to the brain. The vessels lose their elasticity and a blood clot forms at the site of attachment of the cholesterol plaque as a result of platelets adhering to the damaged vascular wall.
- Occlusion of the arteries of the lower extremities. In this case, a sharp closure of the lumen of the peripheral artery and the development of an acute form of ischemic syndrome are characteristic. Such changes lead to disruption of trophism and nutrition of the lower extremities, paralysis and even gangrene . With occlusion of the femoral artery, extensive circulatory disorders develop not only in the lower extremities, but also in the pelvic organs, which can pose a real threat to the life and health of the patient. Both the superficial (SFA) and deep femoral artery can be affected.
- Occlusion of cardiac vessels. Damage to the coronary arteries is very common. When the supply vessel is completely blocked, irreversible consequences develop in the form of necrosis - myocardial infarction . ischemia develops , which manifests itself as signs of angina pectoris . The blockage can occur due to a blood clot or atherosclerotic plaque. With long-term, chronic occlusion, bypass pathways are formed - collaterals, through which nutrients are supplied. In 98% of cases, the coronary arteries are affected by atherosclerosis .
- Occlusion of the subclavian artery. As a result of blockage, ischemia occurs not only in the upper extremities, but also in the brain. Dizziness , weakness in the arms, problems with speech and visual perception appear The consequences of occlusion of the subclavian arteries are severe.
- Occlusion of the carotid artery. There is both complete and partial blockage of the vessels that supply blood to the brain. Occlusion of the internal carotid artery, which nourishes and supplies the brain and is responsible for intracranial circulation, is rare. Damage to the common carotid artery can lead to problems with visual perception.
- Occlusion of the iliac artery. The first manifestation of the lesion is numbness in the legs, fatigue, ischemia of the legs, and the appearance of pain when walking. Gradually, damage manifests itself in the functioning of the pelvic organs, impotence , and the functioning of the abdominal organs is disrupted.
- Occlusion of the eye or occlusion of the retinal artery. It is extremely rare. It is characterized by a completely asymptomatic course and a sudden deterioration in vision up to complete blindness.
Occlusion in dentistry
In dentistry, occlusion is closure, i.e. the most complete and dense contact of the chewing surfaces with each other. In simple words, dental occlusion is the relationship of the jaws relative to each other.
The occlusal surface of the tooth is that part of the tooth surface that is located from the deepest part of the central fissure to the top of the cusps.
6 keys of occlusion according to Andrews
Andrews is credited with formulating his own theory based on crown morphology and evaluating 120 models with “ideal” occlusion in orthodontically untreated patients. He developed rules (keys) for the relationship of a single tooth to both the adjacent and the antagonist tooth, taking into account its position.
- Key 1 – ratio of painters;
- Key 2 – mesiodistal type (crown angulation);
- Key 3 – torque and inclination of tooth crowns;
- Key 4 – rotation;
- Key 5 – contact point;
- Key 6 – Spee curve.
Central occlusion
The definition includes other names:
- intertubercular contact;
- maximum closure of teeth;
- intertubercular contact position;
- intercuspation.
Central occlusion determines the position of the lower jaw, which is characterized by:
- uniform, symmetrical contraction of the muscles that raise the lower jaw;
- the central position of the heads of the temporomandibular joint in the articular fossae;
- maximum fissure-tubercle contacts of the dental rows.
Dental signs of central occlusion:
- Between the teeth of the lower and upper jaws there is the most dense tubercle-fissure contact.
- Each tooth intersects with two antagonists. The only exceptions are the lower central incisors and upper third incisors.
- The midlines between the central lower and upper incisors are located in the same sagittal plane.
- The lower teeth overlap the upper teeth by no more than a third of the length of the crown in the frontal region.
- The cutting edge of the lower incisors contacts the palatal cusps of the upper incisors.
- The upper first molar occludes the 2 lower molars, covering two-thirds of the first molar and one-third of the second.
- The buccal cusps of the lower teeth overlap the buccal cusps of the upper teeth in the transverse direction.
You can learn more about occlusion in dentistry in the book “Functional Occlusion” by Peter Dawson.
Treatment methods for femoral artery occlusion
With limited occlusion, the body can compensate for the blood circulation of the limb using blood flow through the lateral branches of the arterial system (collateral circulation). In this case, conservative treatment is possible.
With increasing severity of ischemic symptoms, intermittent claudication occurring after less than 100 meters of walking, pain at rest, it is necessary to resort to surgical treatment. Such symptoms mean that circulatory compensation is insufficient, and this threatens the development of ulcerative-necrotic changes, gangrene and loss of limb.
Surgery
In the surgical treatment of occlusion, depending on the area of artery damage, the following are used:
- endarterectomy (removal of atherosclerotic deposits from the lumen of the artery);
- femoropopliteal bypass surgery;
- femoral-tibial bypass (if there is concomitant occlusion of the popliteal artery).
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Causes
Most often, occlusion develops as a result of embolism, blockage of a blood vessel by a dense formation. This process can develop as a result of:
- Infectious disease . In this case, the blood flow is blocked by inflammatory-purulent blood clots or the accumulation of a large number of pathogenic microorganisms.
- Air embolism . It develops as a result of an air bubble entering the systemic bloodstream. It is determined after traumatic damage to a vessel or after an incorrectly performed injection.
- Fat embolism . As a result of metabolic , fat particles accumulate and a fat clot forms from them.
- Arterial embolism . Thrombi form on the valve apparatus of the heart and are characterized by instability and mobility, which can lead to separation of thrombotic masses and blockage.
Occlusion of the vessels of the neck and coronary arteries is formed in the area of their branching or narrowing.
Causes of thrombosis:
- malignant neoplasms;
- atherosclerosis;
- traumatic injuries;
- aneurysms;
- thromboembolism.
As a result of traumatic damage to muscle tissue and the skeletal system, compression occurs and blood flow is blocked.
Anatomical description of the disease
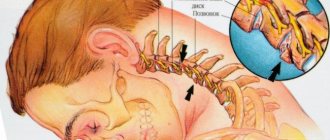
Occlusion of the carotid (carotid) arteries is a partial narrowing or complete occlusion of the large canals supplying the brain. There are episodes of asymptomatic progression, often accompanied by systematic oxygen deprivation of brain areas and arterial strokes. According to medical statistics, ischemia is most often caused by damage to the extracranial parts of the circulatory system. Intracerebral degeneration of vascular tracts is detected four times less frequently. Blockage of the carotid ducts is the cause of ischemic disease of the central nervous system in 56% of cases. A third of all recorded impacts occur as a result of the closure of these channels.
The narrowing of the bloodstream may be partial, then a diagnosis of stenosis is made. When the vessel is completely blocked, a stroke occurs, and sometimes the disease causes sudden death.
Symptoms
Against the background of damage to the brachiocephalic vessels, there is a decrease in performance, weakness and dizziness . The brachiocephalic trunk is responsible for the blood supply to the soft tissues of the head and the brain. If the left artery is additionally involved in the pathological process, then the clinical picture worsens significantly. Main manifestations:
- pale skin;
- nausea;
- headache;
- pain during physical activity;
- confusion;
- paraplegia;
- swelling and development of necrosis;
- burning sensation or numbness;
- deterioration of visual perception;
- hallucinations;
- difficulty breathing, swallowing;
- speech disorders;
- cardiopalmus;
- absence of pulse in the affected area.
If any of the above symptoms appear, it is necessary to conduct a thorough analysis and diagnosis to identify the true cause and subsequently prevent the development of severe complications.
Occlusion of blood vessels supplying blood to the brain
Occlusive processes in the arteries supplying the brain are fraught with dangerous consequences. Impairment of cerebral blood supply is fraught with the development of a stroke or ischemic cerebral infarction, and this often ends in the patient’s death, paralysis or dementia. A common cause of this is carotid artery occlusion. It is accompanied by loss of consciousness, nausea and vomiting, impaired coordination, speech and vision, weakness and numbness of the limbs. A harbinger of strokes are transient (cerebral) ischemic attacks, which we described in detail earlier.
Tests and diagnostics
It is recommended to consult a doctor at the first manifestations of the disease. After examination, collecting anamnesis and assessing the manifestations of clinical symptoms, they begin diagnostics, which includes:
- CT arteriography;
- Doppler ultrasound;
- cerebral angiography;
- MR angiography;
- coagulogram;
- MRI of the brain.
Only after a comprehensive examination is appropriate treatment prescribed, which is selected individually for each patient.
What manifestations are accompanied by the pathology?
The clinical manifestations of the disease depend on where the problem is located. Also, the nature of the onset of the disease, which can be sudden or gradual, plays an important role. It is worth remembering that in the first stages of the disease, compensatory mechanisms always turn on. For example, if the blood flow is partially disrupted, a system of collaterals develops, which will provide alternative routes for blood supply to the brain. The lack of oxygen supply is also compensated - the pulse and breathing become more frequent, intracellular processes change. For short-term conditions this is enough, but for serious pathologies it is not. In such cases, symptoms of the condition develop. Naturally, with an abrupt onset and significant stenosis, compensatory forces do not work and the clinical picture has a pronounced character, which indicates a stroke.
One of the first alarm signals is transient cerebral ischemia. These are short-term episodes of circulatory disturbance that can be compensated by collateral blood flow. The condition can be recognized by decreased sensitivity and motor activity, as well as visual disturbances. Patients usually complain of a feeling of numbness in the upper limb, half of the face, and loss of visual fields. Decreased muscle strength in the arm or forearm. The patient feels the movement of dark spots in front of the eyes, as well as a decrease in visual acuity. In some cases, the section of the artery that supplies the retina is affected. In some localizations, corresponding disorders occur - difficulty speaking, hearing, swallowing, facial asymmetry, severe pain. More common symptoms are dizziness, feeling unwell, weakness, and convulsions.
If stenosis develops gradually, the clinical picture also develops slowly. In some cases, it is so nonspecific that it is difficult to recognize the disease. For a long time, both the patient and the doctor may mistakenly believe that the cause of poor health is fatigue or increased stress. Also, the symptoms of occlusion overlap with the symptoms of a tumor process and dementia. This is indicated by increased irritability, depressive disorders, sudden changes in mood, increased drowsiness, decreased memory and mental abilities.
Nonspecific symptoms require a high level of responsibility from the patient and the doctor, since high-quality diagnosis is necessary. The diagnosis determines how correct the treatment of the pathology and the result will be.
Diet for occlusion
To restore the elasticity of the vascular wall, strengthen it and reduce the severity of occlusion, it is recommended to adhere to certain dietary rules. In case of occlusion, it is recommended to adhere to a special cholesterol-lowering diet, which includes:
- Legumes . Beans and legumes are sources of protein, iron, folic acid and contain absolutely no fatty acids.
- Whole grains (wheat bread, buckwheat, oatmeal and brown rice).
- Cabbage (all types, especially broccoli). Prevents salt deposition, normalizes the lipid spectrum of cholesterol, enriches the body with vitamins K and C.
- Asparagus . Helps lower blood pressure and reduce cholesterol in the blood.
- Persimmon . Rich in fiber and has a pronounced antioxidant effect.
- Spinach . Allows you to reduce blood pressure in hypertensive patients.
- Turmeric . It has an anti-atherosclerotic effect, reduces the volume of cholesterol plaques, and reduces the severity of the inflammatory process.
Signs of prognathic occlusion (2)
Malocclusion is characterized by changes in the way the teeth fit together, but additional external signs may also be present. All manifestations of distal occlusion can be divided into 3 groups:
- 1. Intraoral : protruding front teeth, the presence of a distance between the incisors of the upper and lower rows when closing.
- 2. Functional : discomfort when swallowing and chewing, impaired diction, difficulty in nasal breathing. At the same time, an adult who has suffered from the problem since childhood will most likely adapt and will not feel such inconveniences.
- 3. External : protrusion of the nose and upper lip, but sinking of the lower lip, reduction of the chin, in advanced cases the mouth is constantly slightly open. A distal bite can also affect posture: there is a stoop, the body is tilted forward, and the stomach protrudes.
If signs of distal occlusion are detected in a child or adult, you should contact the doctors at Leonid Gorbunov’s orthodontic studio for comprehensive diagnosis and treatment.
List of sources
- Matyushenko A.A. “Pulmonary embolism as a general medical problem”, article in the journal RMZh No. 13 dated 07/03/1999
- Atayan A.A., Kosenkov A.N., Kuznetsov M.R., Chernookov A.I., Ivanova M.I., Khachatryan E.O. “Hybrid tactics in the treatment of acute disorders of mesenteric circulation”, RMZh No. 8(II) dated 10.25.2019
- Yavelov I.S. “The use of anticoagulants during thrombolytic therapy in patients with signs of acute occlusion of the coronary artery: how to individualize treatment?”, RMZh No. 26 of November 30, 2011
Diagnosis of distal bite
Only a professional orthodontist can accurately determine the presence of distal occlusion. First, the doctor examines the oral cavity and can first judge what malocclusion the patient has. However, to confirm the diagnosis and draw up a further treatment plan, additional studies are carried out:
- 1. Computed tomography . Obtaining three-dimensional images of the dentofacial apparatus allows you to determine: the size of the jaws, their relationship, bone structure, the condition of the TMJ, and so on.
- 2. Casts . Taking impressions of the dentition allows you to determine the characteristics of the closure of the teeth. The study helps create a plan for further tooth movement to form a correct bite.
- 3. Photo protocol . Photos are taken with the mouth open and closed, in front and in profile, with a smile and from different angles. This allows you to track the dynamics of bite correction.
Contact our clinic, where diagnostics are performed using modern, precise equipment with a guarantee of reliable results.