What does dental pulp consist of?
Anatomical structure of the dental pulp
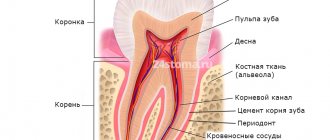
From an anatomical point of view, the tissue is divided into two zones. The coronal dental pulp has a loose structure and is involved in dentinogenesis; all layers of the dental pulp in this part are penetrated by an extensive network of capillaries and nerve cells. The root pulp of a tooth is denser because it does not contain a large number of cellular elements, but is saturated with collagen fibers. Through the apical foramen, the canals communicate with the periodontal tissues and allow minerals and nutrients to reach the tooth walls.
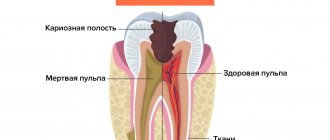
The pulp and dentin of the tooth form a strong complex - the hard tissue protects the tooth pulp from external irritants, and it, in turn, helps the formation of dentin.
The pulp of the front tooth smoothly passes from the crown to the root part, the dental pulp of the molars has clear boundaries - the mouths of the dental canals.
Histological structure of dental pulp
The pulp contains a large number of different elements:
- Elastin and collagen fibers supply the organ with hyaluronic acid, reducing susceptibility to toxins and bacteria.
- Odontoblasts and stellate cells are responsible for the regeneration of dental pulp.
- Leukocytes, lymphocytes and fibroblasts support the vital activity of the epithelium and organize communication between cells.
- A branched network of nerve processes forms Rashkov's plexus and provokes the occurrence of pain sensitivity when exposed to stimuli - the innervation of the dental pulp occurs due to the trigeminal nerve.
- Vessels and capillaries provide the blood supply to the dental pulp, which is necessary to nourish the tissues.
Composition of dental pulp
The fabric is 74% water, the remainder being organic and inorganic layers. Pulp cells include protein compounds, acids, lipids, glucose and various enzymes, which allows the epithelium to actively consume and process oxygen.
Many people mistakenly believe that the pulp is a nerve. The opinion is incorrect, since in addition to nerve plexuses, the tissue contains blood vessels and collagen fibers. |
Vital pulp extirpation
Author: John Whitworth
Teeth with vital pulp contain oxygenated pulp tissue, which in most cases responds clinically to thermal and electronic sensitivity tests. From an intact tooth with an absolutely healthy pulp to a destroyed carious tooth with extensive, irreversible pulpitis. An important finding is that teeth with viable pulp contain little or no microbial infection, at least in the apical areas. Thus, the treatment approach will be different for teeth with completely necrotic, infected pulp and for mature apical periodontitis.
Assuming that the desired outcome of endodontic treatment is the prevention or treatment of apical periodontitis, teeth without preoperative infection or radiographically detectable periapical lesions have a higher treatment success rate than teeth with necrotic/infected pulp and periapical inflammation. In light of the above, dentists can approach the treatment of vital pulp teeth as a simple technical exercise—a quick and predictable mechanical task rewarded with immediate pain relief, satisfactory postoperative radiographs, and assured long-term periapical health. Often overlooked is the attention to detail required to treat the vital pulp under aseptic conditions, to prevent clinically acquired (nosocomial) infection during treatment procedures, and to protect against microbial colonization throughout the period of operation. To ensure long-term function of pulpless teeth, dentists must also minimize the risk of unnecessary, excessive mechanical and chemical treatment of structurally important hard tissues and restore them appropriately after treatment.
Although a report of this nature should include a discussion of instruments, materials and techniques, whenever possible the emphasis should be on the biological principles of infection control and tissue preservation principles in the treatment of teeth with compromised vital pulp.
Figure 1 Deep pulpectomy in an immature tooth with partial pulp necrosis. (a) Presented tooth with recurrent caries and apical periodontitis. Root formation is not complete.
Figure 1 (b) After isolating the tooth, removing carious tissue and restorative material, deep excision of the pulp is performed, not reaching 5 mm from the root apex, using a long-stemmed ball bur. A non-hardening material based on calcium hydroxide was applied to the wound surface for a long time with repeated replacement. (c) One year after treatment, the formation of the apical foramen was completed, the root walls were compacted and a mineralized bridge separated the pulp from the overlying filling material.
Pulpectomy - definition and rationale
A pulpectomy is the fairly simple removal of vital pulp from a tooth, extracted close to the apical foramen, in an area that is likely to be sterile. The empty canal space is then filled and a coronal restoration is performed to protect the pulp from the oral environment and protect the tooth from fracture
Age-related changes in dental pulp
The pulp of temporary and permanent teeth has a similar structure and only becomes thinner over time. Before the roots are formed, the pulp of a baby tooth is concentrated in the coronal part. Later, the tissue begins to spread into the dental canals through the apical foramen and grow into a wide network. The dental pulp in a child has a massive and dense structure, as well as a large fiber size.
The development of dental pulp continues throughout life, but with age, regeneration processes slow down: the number of active cells decreases, which leads to vascular fragility, insufficient tissue nutrition, the tooth suffers from odontoblast atrophy, that is, the impossibility of dentin formation. The described changes apply to older people.
Symptoms that may indicate the development of pulpitis
Knowing the symptoms characteristic of pulpitis will help you promptly suspect the development of this disease and seek treatment for it. The following symptoms will be common to any form of pulpitis:
- Hypersensitivity of the diseased tooth to temperature stimuli;
- Changing the color of the natural enamel coating of the tooth;
- Redness, inflammation of the soft tissues of the oral cavity near the diseased dental unit;
- The appearance of putrid odor from the mouth.
But the main symptom of pulp inflammation will be excruciating pain, which patients describe as shooting, rolling in attacks. The attacks become most intense at night; unpleasant sensations during the initial phases of development are localized in the area of the diseased tooth, and later begin to radiate to different parts of the face, head and even neck. USEFUL TO KNOW: in some cases, pulpitis develops in the tooth without any external manifestations. Moreover, it can at any time turn into periodontitis and periostitis - diseases in which the risk of losing a tooth increases significantly. For timely diagnosis of latent pulpitis and the beginning of its treatment, you should regularly visit the dentist and undergo a preventive examination.
Functions of the dental pulp
The main role of the pulp is to perform several tasks to support the vital functions of the tooth.
- Plastic function.
Formation of basic dentin, as well as the formation of hard tissue in case of damage. - Protective function.
Preventing infections from entering the periodontium through canals, removing dead cells, maintaining regeneration processes. - Sensory function.
A signal about the presence of an external or internal irritant to preserve tooth health. - Trophic function.
Supply of nutrients to dentin and tooth enamel.
Dentinal tubules.
They are pathways connecting the pulp and periodontium, the separating barrier between which is cement covering the tooth root. Normal, intact cement is an obstacle to the penetration of microorganisms and their metabolic products through these structures. Exposed dentinal tubules in areas of damaged cementum may serve as important communication routes between the dental cavity and the periodontium. Exposure of dentinal tubules can be a result of developmental defects, pathological processes, often inflammatory, or iatrogenic procedures. At the root of the tooth, dentinal tubules extend from the pulp to the dentin-cementum junction. They run in a relatively perpendicular direction to this boundary and vary in size from 1 to 3 mm in diameter. The diameter of dentinal tubules changes with age or in response to chronic low-intensity stimuli due to the formation of highly mineralized peritubular dentin. The number of dentinal tubules in the area of the dentinal-cementum junction is approximately 8000 per square millimeter. Simple arithmetic calculations show that the total area of dentinal tubules, providing communication between the tooth cavity and the periodontium, significantly exceeds the size of the apical foramen, around which inflammation most often occurs during pulp necrosis. There are approximately 15,000 tubules per square millimeter in the cervical root region, these tubules can be exposed by periodontitis or periodontal disease, as a result of iatrogenic interventions or developmental defects where cementum and enamel do not join at the enamel-cementum junction, thus leaving or creating areas exposed cement.
Another way of communication between the tooth cavity and the periodontium can be lateral and additional canals. They are located along the root of the tooth. Their prevalence and location have been well studied and documented in papers. 30-40% of teeth have additional canals and most of them are located in the apical third of the tooth root. 17% were shown to have additional canals in the apical portion, 9% in the middle third, and 2% in the upper third. However, there are relatively few destructive changes in the periodontium associated with the lateral canals. Studies show that out of 1000 patients examined, only 2% had the process located in the area of the lateral canals. Additional channels in the area of molar furcation are also pathways of communication between the pulp and periodontium. The prevalence of additional channels in this area is very high and reaches 76%. However, not all of these canals extend throughout the entire thickness of dentin to the bottom of the furcation. Seltzer showed that inflammation can spread to these areas, but the percentage of their involvement in pulp necrosis is relatively low.
What can cause pulpitis?
Burn of tooth pulp
As a rule, a pulp burn during tooth grinding occurs as a result of medical error or carelessness. Before prosthetics, the crown part is treated at high temperatures. Insufficient cooling during the preparation process can lead to a burn, which will provoke subsequent inflammation of the dental pulp.
Dental pulp hematoma
After a tooth injury, there is a possibility of getting a hematoma, that is, bleeding into the dentin. The crown acquires a reddish tint and painful sensations occur when pressure is applied. However, a bruise that has not turned into pulpitis or necrosis does not need treatment and goes away on its own over time.
Caries
Through the smallest cracks in the tooth cavity, infection and pathogenic bacteria penetrate into the pulp. Advanced caries is one of the most common causes of pulpitis.
Any damage or complications of diseases can lead to disastrous consequences if left untreated. Dental pulp necrosis is the process of tissue death due to the spread of infected cells. The anomaly can be recognized by the grayish color of the tooth and incessant aching pain. During treatment, the doctor will perform depulpation, clean and seal the canals. |
Treatment of acute K04.01 (according to MMSI acute focal) PULPTIS
The first thing you need to do is stop the inflammatory process, that is, stop the inflammation.
First, painkillers are prescribed to reduce or relieve pain.
First way.
In young people, at the beginning of the inflammatory process, it is possible to stop the inflammatory processes and preserve the pulp using conservative processes. To do this, the carious cavity is prepared with modern instruments that are available in our clinic, and then
is treated with medication and an anti-inflammatory, regenerating and odonotropic paste is applied, mainly based on calcium hydroxide paste for 4-6 days, and then if there are no complaints, the tooth is filled with permanent fillings.
Second way
When performing this method, first infiltration or conduction anesthesia is carried out, and then the softened tissues of enamel and dentin, as well as the inflammatory pulp at the level of the canal mouth are removed with a diamond bur, then the tooth cavity is cleaned, the bleeding stops and a paste based on calcium hydroxide is applied without any pressure. And ionomer cement is applied to it. The first control after three, and the next controls after 6 months and 1 year.
This method is called vital pulp amputation or pulpotomy .
Clinical picture of acute purulent K04.02 (pulp abscess) (according to MMSI acute diffuse) pulpitis.
- spontaneous pain;
- prolonged pain with short light intervals;
- radiating pain along the branches of the trigeminal nerve;
- intense, unbearable pain;
- increased pain from hot foods;
- short-term relief of pain from cold;
- EDI 30 – 50 mA;
- deep carious cavity with a large amount of softened dentin;
- the tooth cavity is not opened;
- probing is painful;
- percussion is painless;
- palpation of the transitional fold at the level of the inflammatory tooth is painless, but may be sensitive;
- with unformed root apices, percussion and palpation are painful;
- Severe swelling and disturbances in the general condition of the whole body may be observed.
- X-ray – no changes;
Therapeutic methods for treating dental pulp
Therapeutic or conservative are methods of treatment that make it possible to do without removing tissue. These methods of preserving dental pulp are not available to all patients; there are certain indications:
- age not older than 40 years;
- deep caries;
- acute serous-purulent or fibrous pulpitis;
- opening of the dental pulp due to trauma;
- lack of medical intervention in the inflammation process to date.
As a rule, the dentist treats the surgical field with antiseptic solutions, removes the affected tissue and places the drug into the cavity. There are two methods for performing this procedure.
- Indirect covering of the dental pulp.
An antibacterial agent is placed at the bottom of the cavity to stimulate the production of bone substance. Regeneration occurs naturally. - Direct covering of the dental pulp.
The medication is applied directly to the soft tissue to preserve the viability of healthy cells, then isolated with a pad.
Next, the tooth is restored with temporary materials, and after a secondary examination, it is finally restored.
Types (classification) of pulpitis
In 1989, the MMSI proposed the following classification of pulpitis:
1. Acute pulpitis:
- a) acute focal pulpitis;
- b) acute diffuse pulpitis.
2. Chronic pulpitis:
- a) chronic fibrous pulpitis;
- b) chronic hypertrophic (proliferative) pulpitis;
- c) chronic gangrenous pulpitis.
3. Exacerbation of chronic pulpitis.
In Russia, the transition to ICD-10 was carried out in all health authorities and institutions in 1999.
The diagnosis is indicated according to ICD-10. In brackets you can indicate the corresponding form of pulpitis according to MMSI.
Surgical methods for treating dental pulp
In cases where therapeutic methods are powerless, the only option left is to remove the dental pulp. This option is used in cases where the patient’s immunity is weakened, the disease is at an acute stage, or the tooth will be used in the future as a support for prosthetics. Surgery involves amputation or extirpation of the dental pulp.
- Amputation of the dental pulp
- during the procedure, only the coronal part is removed. Prescribed for acute pulpitis or mechanical damage to the dental pulp. - Extirpation
is the complete removal of the pulp. Used for all forms of pulpitis.
The pulp can be removed vitally, that is, under anesthesia without prior killing. If this method is not possible, the doctor resorts to devitalization of the dental pulp - the toxic substance is left in the cavity for about a day, after which the dead tissue is painlessly removed. Means for devitalizing dental pulp include arsenic or paraformaldehyde paste.
How is the operation performed?
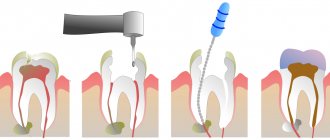
Most often, dentists perform vital pulp extirpation. It includes the following steps:
- professional cleaning of the affected tooth,
- pain relief using local anesthetics,
- isolation of the working area from salivary secretions,
- incision in the arch of the dental cavity,
- removal of the neurovascular bundle,
- restoration of the correct shape of the root canal,
- antiseptic treatment of the tooth cavity,
- installation and grinding of the filling.
How to Keep Your Pulp Healthy
Fortunately, there are steps you can take to keep your pulp healthy. First of all, try to curb your love for sweets. By feeding on sugar, bacteria in the oral cavity produce acids that damage tooth enamel. If you cannot completely give up sweets, eat them immediately after your main meal, and not as a snack during the day, and also rinse your mouth after sweets with mouthwash or, as a last resort, water. Also, don't forget about regular oral hygiene. Floss and brush your teeth twice daily with a quality fluoride toothpaste that fights bacteria and helps prevent tooth decay.
If you feel discomfort in the oral cavity, do not put off visiting the dentist! The sooner you turn to him for help when problems arise, the longer you can maintain healthy teeth and a beautiful smile.
Apical foramen.
It is the main route of communication between the pulp and periodontium. Bacteria and their metabolic products can enter the periodontium and cause inflammation, with corresponding destruction of the bone and tooth root.
When the pulp is necrotic, microorganisms, inflammatory pathogens of various natures, lead to periodontal inflammation. However, it is extremely important and interesting that the same situation occurs when analyzing the opposite situation. It has been shown that in periodontal pathology the pulp is not involved in the process, at least until the pathological pocket reaches the apical foramen.
It appears that as long as the accessory and lateral canals are protected by intact cementum, inflammation does not spread to either side. This is confirmed by the preservation of the vital activity of the pulp in deep pathological pockets that do not reach the apical foramen. However, during surgical treatment of dental periodontium, when removing a layer of cement from the surface of the root, the pulp is often involved in the inflammatory process. Surgical intervention must be justified, and biological, mechanical and aesthetic feasibility must be taken into account.