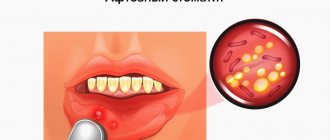
What does aphthous stomatitis look like?
Aphthae occur on the inside of the cheeks or lips, under the tongue, at the base of the gums, or on the soft palate.
https://img.medscapestatic.com/pi/meds/ckb/75/43075.jpg
They can be confused with manifestations of herpetic infection , but the latter usually appears at the red border of the lips, rarely in the oral cavity - usually on the gums or hard palate.
Aphthae first look like red bumps (papules), which then quickly turn into ulcers, surrounded by a red rim and covered with a gray-yellow coating (exudate). 1-2 days before the appearance of aphtha, there may be a local burning sensation of the mucous membrane.
Sometimes the child or family members notice what often triggers the appearance of aphthae. Journaling can help with this.
According to American data, about 20% of the population suffered from recurrent aphthous stomatitis at one time or another in their lives.
Most often children suffer and usually these are minor canker sores.
The peak incidence of aphthae is 1-19 years.
How to treat ulcerative stomatitis?
Effective treatment of Vincent's ulcerative stomatitis should be comprehensive:
- Anesthesia – performed to relieve acute pain. Experts recommend applying compresses with pain-relieving solutions.
- Removing rashes. This should only be done by a doctor. First, compresses with a softening composition are applied to the ulcers, after which the crusts are gradually cleared from the surface of the mucosa, treating with hydrogen peroxide, potassium permanganate, chlorhexidine, etc.
- General treatment. It involves taking antihistamines that relieve general tissue irritation and the inflammatory process. For severe manifestations and complex symptoms, antibiotic therapy is prescribed. It is also recommended to take a course of vitamin therapy.
- Sanitation of the oral cavity. Effective treatment of caries, removal of pathological teeth. For wound healing, treatment with keratoplasty preparations, gels and ointments is recommended.
It is important! The disease cannot be treated at home! The maximum you can do on your own is to rinse your mouth with a decoction of chamomile or calendula, but strictly after professional dental care.
Types of aft.
Small aphthae is the most common type of aphthae (80-85%). Their size ranges from 1 to 10 mm. Ulcers can appear singly or several at a time (up to five).
Usually heal in 7-10 days.
Large aphthae (10-15%) - more than 10 mm in diameter, can even be up to 3 cm, deeper, take longer to heal (10-30 days).
They may leave scars behind. Very rare in children.
Herpetiform aphthae (5-10%) are small, from 1 to 3 mm, located in groups like herpetic vesicles. They heal quickly, within 10 days. They are not typical for children; they usually occur in the elderly.
The rest of the oral cavity looks normal - there is no inflammation of the gums, redness of the tonsils and pharynx, enlarged and painful cervical lymph nodes.
There is no fever or other general manifestations.
Aphthae in children is manifested primarily by refusal to eat and drink due to pain in the mouth.
The reasons for the recurrence of aphthae are not completely clear; the most popular theory is related to errors in the immune system.
Doctors most often do not find a specific cause of the failure; most likely it is a combination of several factors.
But doctors still have assumptions about some factors.
What is stomatitis?
Stomatitis is an inflammatory disease of the oral mucosa. It occurs for various reasons - due to bacterial, viral or fungal infections, due to injuries, biting the tongue or cheek, rubbing the gums with a prosthesis, etc. If we keep in mind the various causes of occurrence, different localization and nature of the course, then we can even say that stomatitis is not one disease, but a whole group with similar symptoms.
Many people are interested in whether stomatitis is contagious. No, it itself is not contagious, but if you consider that it can be caused by a viral or bacterial infection, then contact with the patient must be limited - no kissing or drinking from the same cup. This is especially true for children, since they are more direct in expressing feelings and tend to often forget about hygiene requirements.
Considering the question of how stomatitis is transmitted, we emphasize once again that stomatitis as an inflammation of the mucous membrane is not transmitted to other people. But if it is caused by a herpes virus, streptococcal or candida infection, then the patient may well transmit this infection to others through close contact (for example, parents often try baby drink by drinking from the child’s cup - this cannot be done with stomatitis). Whether this infection will lead to a similar disease in the infected person largely depends on his individual immunity.
Sometimes they ask how long it takes for stomatitis to go away. It is important to understand that this directly depends on the cause of the disease, the stability of the immune system and the treatment methods used. If acute stomatitis is caused by injury (for example, a burn from a hot drink or injury to the mucous membrane by a sharp edge of a tooth), and the immune system is strong enough, then the disease can go away in 3-4 days. If the cause is infection, but the patient strictly follows the doctor’s recommendations, then treatment of the acute phase of the disease may take 10-14 days. With reduced immunity (diabetes mellitus, HIV and other problems), treatment of stomatitis may be delayed indefinitely.
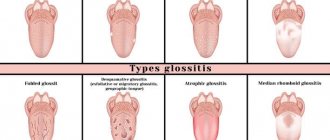
In the mouth, stomatitis can have different localizations. Simply put, the lesion can affect various places on the tongue, gums, roof of the mouth, lips and even the throat. As a rule, this does not affect the treatment method, but it can simplify, or, on the contrary, complicate treatment (if the damage affects hard-to-reach or constantly exposed areas).
Stomatitis on the lip occurs almost most often. Often it is the herpes virus that causes painful swelling, pimples or sores on the lips. At the same time, damage to the mucous membrane of the lips may be a symptom not of stomatitis, but of a lack of B vitamins.
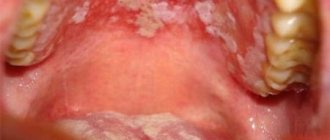
Stomatitis on the palate is also one of the characteristic signs of herpetic stomatitis. But it can also be caused by other reasons.
Stomatitis on the tongue often occurs as a result of biting, injury from a chipped tooth with a sharp edge, or a burn. If the tongue is covered with a white cheesy coating, then it may be candidal stomatitis.
Stomatitis on the gums can be the result of tooth extraction, damage from a toothbrush with too hard bristles, or pieces of hard food.
Stomatitis in the throat is sometimes confused with sore throat. The symptoms are similar - sore throat, especially when swallowing, redness, increased salivation. But if a careful examination reveals blisters and ulcers, then this is most likely stomatitis.
You need to know that the location of ulcers, redness and swelling in a particular place is not an unambiguous sign of a particular type of stomatitis. The reasons must be determined by a doctor based on examination and test results.
What predisposes to recurrent oral aphthae?
Perhaps the microflora of the oral cavity, herpes group viruses, and maybe Helicobacter pylori, a microorganism that causes stomach and duodenal ulcers, play some role.
Also influence:
- injuries to the oral mucosa
- stress
- deficiency of vitamins B12, B1
- vitamin D deficiency
- zinc deficiency
- poor oral hygiene
- nitrates in drinking water
- Sodium lauryl sulfate is a very popular surfactant in the industry, which is often added to toothpastes for better cleaning and foaming effect.
- food allergies (eg, cow's milk protein) or food hypersensitivity (cinnamon, coffee, chocolate, cheese, figs, pineapple, citrus fruits, some spices)
- non-steroidal anti-inflammatory drugs
It is very important to understand: recurrent aphthae is an independent disease (most often this happens) or a manifestation of some systemic disease.
The latter option is rare, but the doctor should always keep in mind the possibility of this situation.
Signs and symptoms of stomatitis
The symptoms of acute stomatitis are very similar for different types of this disease, although there are differences that make it possible to more accurately diagnose the disease. The location of the rash does not always indicate the form or causes of the pathology. The symptoms of stomatitis on the tongue or in the throat are generally the same; much more important is the nature of the manifestations, the presence of rashes - small blisters or one large ulcer. The severity of the inflammatory process allows us to judge whether the disease is milder, catarrhal, or more severe. For example, the symptoms of catarrhal stomatitis include only:
- redness and swelling of the mucous membrane,
- soreness, sometimes bleeding gums,
- bad breath,
- increased (or, on the contrary, decreased salivation),
- Sometimes a white sticky coating appears.
But at the same time, there are no rashes or ulcers, the temperature rises very rarely and slightly, the lymph nodes are not enlarged. It would seem that this indicates the stability of the immune defense and an easy and quick cure, however, even this form of stomatitis needs treatment, otherwise, once neglected, it can become more severe, ulcers will appear, a bacterial infection will join, which will spread to neighboring organs, causing serious complications.
So, let us highlight the symptoms of the disease characteristic of stomatitis:
- redness and swelling of certain areas of the mucous membrane,
- blisters, blisters or sores (not always),
- pain, burning, itching in the affected areas, which intensifies when touched, eating, talking,
- bad breath,
- plaque (white or grayish-yellow) on the affected areas,
- fever, chills (not always, more often in children than in adults),
- signs of intoxication - weakness, headache, nausea (not always).
Symptoms of stomatitis in newborns are slightly different. Most often this is:
- temperature increase,
- baby's refusal to breastfeed,
- restlessness and moodiness of the baby,
- small blisters or sores on the oral mucosa.
The most common causes of stomatitis in newborns are the herpes simplex virus (65%) or the Candida fungus (30%). In the case of herpes, blisters with transparent contents appear on the mucous membrane, which soon burst, forming ulcers. With candidal stomatitis, white dots appear that merge to form a solid white coating. Since damage to the mucous membrane causes pain and burning, the baby refuses to eat, which is very dangerous, as it leads to weight loss and dehydration.
Temperature with stomatitis
The question of whether there can be a fever with stomatitis usually worries the parents of a sick child, who are trying to understand whether it is worth seeing a doctor. Yes, with stomatitis in children, the temperature very often rises. In general, the signs of stomatitis in children are usually more pronounced than in adults, due to the fact that the child’s immune system still reacts to infections and inflammation quite violently.
But even in adults with stomatitis, the temperature may rise, especially with a more severe course of the disease.
You need to know how long the temperature lasts for stomatitis. Usually this is several days, but depending on the cause of the disease and the severity of its course, this time may be shorter or longer. In any case, you should definitely consult a doctor - correct diagnosis and proper treatment can shorten this period and prevent the disease from developing into a complicated form.
Which doctor should I contact if I have signs of stomatitis?
Which doctor treats stomatitis? At the first signs of stomatitis, you should go to a doctor who treats diseases of the oral cavity - a dentist. He will determine the type of disease and its causes, prescribe treatment, and, if necessary, refer you for tests or to a specialized doctor to clarify the diagnosis.
If manifestations of stomatitis are noticeable in a child, then you should contact your local pediatrician.
Diagnosis of stomatitis
Successful healing requires correct diagnosis of stomatitis. Only a doctor with the necessary knowledge and professional experience can accurately determine the type of disease, establish the causes and propose treatment tactics taking into account the individual characteristics of a particular patient.
On the one hand, this disease has very characteristic symptoms and stomatitis is relatively easy to diagnose. On the other hand, stomatitis may be concomitant with another, more serious disease. The effectiveness of the medications and treatment methods used directly depends on the correct identification of the causes that caused stomatitis.
Treatment of stomatitis in adults
Adults usually tolerate stomatitis more easily than children, however, stomatitis in adults also requires treatment, since if it is neglected, it can become more severe, cause serious complications, and become chronic.
Treatment of stomatitis in adults should always be based on identifying the causes of the disease. If the cause is an allergy, then it is necessary to identify the allergen and eliminate contact with it. If the cause is a bacterial or viral infection, then a course of antibacterial or antiviral therapy should be administered. Depending on the specific diagnosis, the most effective painkillers, antiseptic, anti-inflammatory and healing agents in a particular case are selected. To the question - how to treat stomatitis in adults? — the dentist must answer. In no case should you self-medicate, as this can have the opposite effect and lead to a worsening of the situation.
Treatment of stomatitis includes:
- Elimination of the cause of the disease (allergy or viral infection, bacterial contamination).
- Local treatment - rinsing with antiseptics and herbal decoctions, using anti-inflammatory and healing gels.
- Suppression of acute conditions - reduction of high temperature, pain relief.
In addition to systemic treatment aimed at suppressing infection, antihistamines are often used, and local treatment - rinses, applications, ointments and gels, the purpose of which is to clean the surface of the mucous membrane from plaque with microorganisms, prevent the proliferation of pathogenic microflora, reduce inflammation, eliminate pain, and stimulate regeneration of damaged tissue.
How to rinse
Mouth rinsing for stomatitis is aimed at mechanical removal of dead epithelial cells, mucus containing pathogenic microflora, as well as the death of harmful microorganisms and suppression of their reproduction.
One of the best antiseptics is Miramistin - it has not only antimicrobial activity, but also antiviral activity (including against both herpes simplex viruses). It also restores local immunity of the mucous membrane.
The second rinse option is chlorhexidine. It has less antiviral protection, but more actively suppresses bacteria, and most importantly, it leaves an indelible layer of the drug on the mucous membrane, which prolongs the rinsing effect.
Furacilin and other antiseptics give good results. Hexoral contains not only an antiseptic, but also anti-inflammatory and analgesic components.
Rinsing with herbal decoctions helps with stomatitis: chamomile, sage, calendula, eucalyptus, etc. But you need to understand that these remedies are auxiliary, not primary - you should not rely on them alone in the treatment of such a serious disease as stomatitis.
Soda for stomatitis
Rinsing with soda for stomatitis has two advantages: first of all, soda softens and helps remove mucus and bacterial plaque. In addition, it creates an alkaline environment, which is destructive for many harmful bacteria, fungi and viruses.
Soda solution for stomatitis does not cause burning or pain, has no contraindications, and is suitable even for children. To prepare it, you need to dissolve 1 teaspoon in 200 ml of warm water. The solution will help reduce swelling and pain, soothe the mucous membranes, and slow down the development of harmful microorganisms.
Stomatitis during pregnancy
Stomatitis occurs very often in pregnant women. The reason for this is weakened immunity, lack of vitamins, and hormonal changes in the body. It is necessary to treat this disease only under the supervision of a doctor, since only a doctor can prescribe medications that will not harm the health of the mother and her unborn baby.
To avoid stomatitis during pregnancy, it is necessary to visit the dentist in advance and perform a complete sanitation of the oral cavity - cure caries, remove tartar, and solve all other problems. And also regularly and carefully care for your oral cavity throughout the entire period of pregnancy, take care of your health and follow all doctor’s recommendations.
Antibiotics for stomatitis
In all cases, antibiotics are prescribed only by a doctor. They are effective only against bacterial infections and the forms of stomatitis caused by them (for example, with Vincent's ulcerative necrotizing stomatitis). Viral types of stomatitis cannot be cured with antibiotics. The success of treating stomatitis with antibiotics directly depends on correct diagnosis and accurate selection of the most effective drugs and dosages in a particular case.
What systemic diseases can manifest as aphthae?
- Reiter's syndrome
- Behçet's disease
- AIDS
- cyclic neutropenia
- PFAPA syndrome
The gastroenterologist is especially interested in the connection between recurrent ulcers and specialized systemic diseases.
Celiac disease is found in 5% , and for a long time canker sores may be the only manifestation of a reaction to gluten.
Let me remind you that the estimated prevalence of celiac disease in the general population is about 1%.
Enamel defects and aphthous stomatitis in celiac and healthy subjects: Systematic review and meta-analysis of controlled studies
Other important conditions that manifest as canker sores are inflammatory bowel diseases: Crohn's disease and ulcerative colitis.
Extraintestinal Manifestations of Pediatric Inflammatory Bowel Disease: Prevalence, Presentation, and Anti-TNF Treatment
Is treatment possible at home?
Treating stomatitis at home is quite possible, especially if it is not severe. However, it is still necessary to consult a doctor for an accurate diagnosis and choice of medications than to treat stomatitis at home.
To treat herpetic stomatitis at home, local remedies are sufficient: rinsing with miramistin (3-4 times a day) or hexoral. To suppress inflammation, you can use Cholisal gel, for faster healing of ulcers - solcoseryl gel (or Actovegin), sea buckthorn or rosehip oil, oil solutions of vitamins A or E. If rashes appear on the lips or skin around the mouth, you can use Zovirax cream or acyclovir. In severe cases of the disease, it is necessary to use drugs against the herpes virus, but they must be prescribed by a doctor.
In general, it is dangerous to treat severe forms of stomatitis at home, especially such as Vincent’s ulcerative necrotizing stomatitis. To combat it, antibiotics will be required, which should be selected by the attending physician.
What can help in finding the cause of aphthae?
A conversation sometimes helps to find out whether relatives have important diseases with a family predisposition - celiac disease, Crohn's disease, lupus erythematosus.
During the examination, the doctor can evaluate the general manifestations of the disease (not typical with ordinary recurrent aphthous stomatitis) and check for the presence of ulcers outside the oral cavity.
The simplest laboratory examination is carried out - this is most often enough.
A general blood test may show anemia due to deficiency of iron, folic acid, and vitamin B12.
The level of neutrophils is also assessed - their decrease may be a sign of the rare systemic disease cyclic neutropenia
A high ESR may be a sign of Crohn's disease and ulcerative colitis.
Serum iron levels may be reduced in up to 20% of recurrent canker sores.
Stomatitis and coronavirus
There is a lot of talk now that many people develop stomatitis due to coronavirus. And so the question arises - how are they connected? It is quite obvious that coronavirus infection greatly weakens the body, undermines the immune defense, and leads to various complications. And with a decrease in immunity, as we know, many dormant infections in the body are activated, which lead to stomatitis. Therefore, it is impossible to consider stomatitis as a symptom of Covid. But it is more logical to look at stomatitis as a concomitant disease that occurs in approximately half of those suffering from coronavirus infection.
After coronavirus, stomatitis can also occur as one of the possible complications. Particularly susceptible to this are those patients who did not closely monitor the condition of the oral cavity, rarely visited the dentist, who had advanced caries or problems with the gums (gingivitis, periodontitis), and tartar deposits. In order to avoid contracting stomatitis after Covid, it is important to regularly and thoroughly perform oral hygiene, brush your teeth, and visit the dentist in a timely manner.
Stomatitis rarely occurs after vaccination against coronavirus. Some patients have a more difficult time with vaccination, so a decrease in immunity may result in a recurrence of stomatitis, especially in those who have had it before or in those who are at risk.
Treatment of aphthous stomatitis.
There is no radical and quick treatment.
The main task of the doctor is to fight the pain caused by aphthae. This is especially important for young children, who may refuse to eat or drink due to pain and become easily dehydrated.
For this purpose, local painkillers and drugs are used that form protective films on the aphthae.
The second goal is to speed up healing.
The most popular drugs for healing are anti-inflammatory corticosteroids for aphthae, in rare, especially severe situations - even orally for a short course (prednisolone tablets).
The third task is to avoid or at least reduce the frequency of recurrent aphthae.
For some people, regular intake of vitamins (especially B12), zinc, and iron helps.
Avoiding oral hygiene products containing lauryl sulfate may be helpful.
Together with your dental hygienist, you can consider ways to improve your oral hygiene.
A gluten-free diet will help with celiac disease.
Types of stomatitis for treatment
There are four levels of classification of the disease, each of which has its own subtypes. To determine treatment methods, you must know the correct diagnosis. Therefore, it is necessary to consider the types of Vincent’s infectious disease:
- In the division regarding the nature of the course of the disease, acute, subacute, chronic ulcerative-necrotic degrees and relapse are distinguished.
- Regarding the complexity of the disease, stomatitis is mild, moderate and severe.
Each type manifests itself in different symptoms, so in the next section we will look at what the patient feels at each stage of the disease.
Conclusions:
Aphthae in the mouth recur at some point in life in almost 20% of all people, most often in the second decade of life.
It is difficult to establish a clear and unambiguous reason.
If recurrent aphthae occurs, the pediatrician, physician, or dentist should consider the possibility that rare aphthae are a manifestation of a serious systemic disease.
In such situations, the gastroenterologist must exclude celiac disease, Crohn's disease and ulcerative colitis.
5, total, today
Treatment of stomatitis in children
How to treat stomatitis in a child depends on the cause of the disease. Fungal candidiasis infection, or herpes virus, enterovirus require different treatment tactics and the use of different drugs. This is why it is important to see a doctor as soon as possible.
Children's stomatitis is usually treated with gentle means, limited to rinses, anti-inflammatory and painkillers, and vitamins. But in cases where the disease is more severe, antifungal, antibacterial or antiviral agents are used, the choice and dosage of which is prescribed by the attending physician.