Young people often don’t think about whether stomatitis is transmitted through kissing, and carefreely kiss their other halves. At the same time, they do not take any measures for treatment, considering this disease to be trivial. Is stomatitis so dangerous that you can’t contact other people?
Stomatitis is an inflammation of the oral mucosa, which in most cases is accompanied by the formation of ulcers. Along with this, swelling of the mucous membrane is observed, and a white or yellow-white coating forms. When communicating, a person feels discomfort, and pain occurs while eating. Increased salivation, gums often bleed, and bad breath appears.
What is stomatitis
Stomatitis (mucositis) is a disease that is accompanied by damage to soft tissues in the oral cavity.
It can be either an independent disease or a complication of various pathological processes, for example, measles, influenza, scarlet fever, etc. Until recently, stomatitis was considered a childhood disease. Today it is becoming more common in adults too. This trend raises questions about whether stomatitis is transmitted and, if so, how to protect yourself and your child. It all depends on the form of manifestation of the disease
Hepatitis A
This is an infectious disease that affects the liver. Hepatitis A in most cases ends in complete recovery. The disease does not become chronic. But the danger is that the disease is extremely contagious and a sick person can infect a huge number of people without even knowing that he is a carrier of the virus. The infection is most contagious in the last days of the incubation period, while there are no symptoms. In this case, infection can occur not only through a kiss, but even through objects touched by the patient.
Symptoms of stomatitis
Stomatitis can be recognized by the following signs:
- ulcers, wounds, erosions and rashes on tissues;
- red color of the mucous membrane;
- plaque on the tongue, inner surface of the cheeks, palate;
- unpleasant taste;
- swelling of tissues;
- heavy salivation;
- bad breath;
- itching and burning – in some cases;
- discomfort and pain;
- bleeding gums – occasionally;
- increased body temperature;
- lymphadenitis.
Symptoms in children are always more pronounced. The child often feels severe pain. Adults tolerate the disease easily. Its symptoms usually do not cause severe discomfort.
When the first symptoms appear, you should immediately consult a doctor to protect yourself and, possibly, others.
How is stomatitis transmitted, is it contagious or not?
Changes in the mucous membrane of the oral cavity in a person, whether ulcers or scratches, cause discomfort and interfere with normal life. When such changes are detected, many immediately believe that it is stomatitis. How to distinguish characteristic rashes from other diseases of an inflammatory nature and what it is, whether it poses a threat to others and the victim’s body as a whole are questions that plague those who are faced with this problem.
What is stomatitis: causes and symptoms
Stomatitis is an inflammatory disease that affects the oral mucosa, which is caused by various infectious and non-infectious factors.
Over time, the usual form of the sore can become complicated, when ulcers and hemorrhages appear at the site of inflammation, causing even greater discomfort for the patient at the time of eating. Against this background, body temperature rises, malaise and drowsiness appear.
Based on the etiological factor, you can understand whether stomatitis is contagious or not for surrounding people.
For non-infectious stomatitis, the trigger is often a weakened immune system. Young children often face this problem, since their immunity is still defective.
The most common causes of the disease are:
- oral care;
- cleaning your mouth with someone else's personal hygiene devices;
- reduced immune system due to concomitant diseases;
- infectious nature;
- allergic reactions to the active components of toothpastes or rinses;
- mechanical damage from a toothbrush with rough bristles or dental sticks.
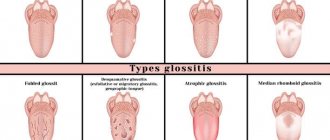
Types of stomatitis and routes of infection
In order to figure out whether the patient is contagious to others or not, it is important to distinguish between the types of stomatitis.
- Infectious etiology:
- viruses;
- bacteria;
- fungal flora.
- Non-infectious nature:
- traumatic;
- aphthous.
An examination of the patient’s oral cavity and a survey will help you understand which type is present in the patient. It is important to know with whom this person communicated the day before and what complaints he had. Knowledge of the distinctive features of each listed species will be able to correctly guide the doctor as to whether there is a risk of becoming infectious or not.
Is stomatitis in adults contagious or not?
Due to the fact that there are many etiological factors, not all of them are dangerous. Infectious stomatitis is contagious in adults and children, non-infectious diseases (traumatic and aphthous) are not contagious.
Viral lesions of the mouth, regardless of the pathogen, are transmitted to others through any contact (domestic, hematogenous, etc.) with an infectious person. This species is contagious.
In children, the main cause of stomatitis is the proliferation of bacterial pathogenic flora, due to their curiosity and mania for putting everything in their mouth.
Is stomatitis transmitted through a kiss or not?
Some types of stomatitis can be transmitted through saliva (kissing). Any pimple of infectious etiology poses a certain threat to the health of the person in contact with the patient.
How can stomatitis be transmitted?
- airborne droplets (at the time of communication);
- hematogenous route (through blood);
- contact or household route (unwashed hands, use of shared utensils or other personal hygiene devices);
- from mother to child (breastfeeding);
- interaction with other biological fluids (saliva during kissing, the entry of amniotic fluid into the baby’s oral cavity, sexual intercourse).
Since stomatitis of infectious etiology is contagious for any person, you should familiarize yourself with each type in detail and learn to distinguish them from non-infectious inflammation.
Viral
The viral form is one of the most contagious among other types. This disease is characterized by the presence of a specific pathogen that causes this condition. In this regard, the following are highlighted:
- herpetic;
- enterovirus;
- influenza and parainfluenza;
- associated with the causative agent of chickenpox;
- adenoviral.
Depending on the incubation period, which lasts 5–14 days, characteristic symptomatic manifestations appear. During this period of time, the patient is contagious to others, but danger threatens when symptoms appear (presence of ulcers with blisters, soreness, elevated body temperature). More often, stomatitis is transmitted by airborne droplets.
When kissing an infected person, there is an increased risk of stomatitis (contact with infectious biological fluid).
It is important not to confuse the clinical manifestations of infectious stomatitis with signs of tonsillitis (during examination, the mucous membrane of the tonsils is affected).
Bacterial
Bacterial stomatitis - manifests itself in children. This is due to a weak immune system and frequent injuries to the oral mucosa. Damaged tissue is an entry point for bacteria. In the area of implantation, local inflammation, swelling, and pain appear. There is an unpleasant odor from the mouth. When foreign microorganisms enter the blood, intoxication syndrome increases (body temperature rises, malaise, drowsiness, loss of appetite).
This species is as contagious as a viral one, and is most often transmitted through the air and through household contact.
Fungal
Fungal stomatitis in the mouth is contagious for healthy people if they use shared, poorly washed dishes, etc. The household route of transmission predominates here.
A characteristic feature of this type of stomatitis will be a white coating over the inflamed area of the mucous membrane. Intoxication syndrome is unlikely, since the fungal infection occurs only in the mucous (mucosal) layer.
Aphthous
Aphthous stomatitis is an inflammation of the oral mucosa that is not associated with an infectious nature. It occurs most often against a background of stress or as a manifestation of a local allergic reaction.
Upon examination, there will be a white or yellow sore - aphtha, which brings discomfort while eating. Don't worry about your loved ones - it's not contagious!
Traumatic prosthetic stomatitis
Sores or ulcers often appear in the oral cavity due to damage from foreign bodies (solid food, dentures, toothbrush with coarse bristles, etc.). Since the dentures are not tightly fixed, their movement causes irritation and injury to the mucous membrane. At the site of unstable fixation, the tissue becomes inflamed.
Despite the safe form of the disease in this category of people, the question arises whether it is possible to become infected with traumatic stomatitis in general or not.
With ordinary prosthetic stomatitis, there is no danger to others, but if complications are detected after infection, the patient becomes infected.
Preventive measures. How to protect yourself when communicating with a sick person
In order to prevent the development of stomatitis and not become contagious, you need to learn a few points:
- oral hygiene (using your own toothbrush);
- thoroughly wash shared utensils (it is advisable to have your own cup, plate, fork, etc.);
- interrupt contact with an infectious person (wearing a medical mask, keeping a distance at the time of conversation);
- the use of vitamin complexes with reduced immunity;
- proper nutrition;
- visit the dentist once a year.
If signs of illness are detected and in order to avoid possible infection of relatives, you should immediately seek medical help from a dentist.
As a result, it should be remembered that stomatitis that has an infectious etiology is contagious. It is not difficult to distinguish this species from a non-infectious one. Knowledge of the clinical picture of the disease can preserve not only the health of the infected person, but also the health of the people around him.
Types of disease
Stomatitis has different forms, depending on which the doctor determines whether it is contagious or not, and also prescribes appropriate treatment.
Allergic stomatitis
This is a common form of the disease that is difficult to treat. From the name it is clear that the cause of its development is an allergy, but it is necessary to find out what exactly it is. These could be medications, food, materials used for prosthetics. The disease is accompanied by the appearance of ulcers, which provoke pain.
Viral stomatitis
The most common type of viral stomatitis is herpetic stomatitis, the causative agent of which is the herpes virus. There are other forms that are provoked by adenovirus, enterovirus, etc. They are often found in children under 5–6 years of age, but are also common among older age groups. A feature of viral stomatitis is its erosive spread, when one ulcer appears next to another. Herpes mucositis may cause complications such as fever, nausea, vomiting and diarrhea.
This form of the disease is transmitted to others by contact and airborne droplets. If it is diagnosed, for example, in someone in kindergarten, then quarantine must be introduced. Infection occurs through dishes and toys, so the disease can quickly spread from child to child.
The virus spreads from nursing mothers to children if hygiene rules are violated. Adults become infected even through handshakes. Sneezing also causes the disease to develop.
Aphthous stomatitis
This form is common among adults. It develops against the background of a weakening of the body’s immune forces, so aphthous stomatitis is a common occurrence in spring and autumn. With this type of disease, characteristic aphthae appear - small ulcers. They can be single or group. Aphthous mucositis is not spread from person to person.
Fungal stomatitis
The disease manifests itself in children and adults, mainly in infants and women. It is provoked by fungi of the genus Candida, which are activated in the oral cavity when the immune system is weakened. The cause of fungal stomatitis can be long-term use of antibiotics. In addition to ulcers, its characteristic feature is a cheesy coating on the tongue, palate and inner surface of the cheeks.
Bacterial stomatitis
This type of disease is diagnosed when the oral cavity is affected by microorganisms, most often streptococci, staphylococci. The manifestation of bacterial stomatitis is provoked by tuberculosis, as well as sexually transmitted diseases, for example, gonorrhea, syphilis. More often, children whose immunity is not strong enough suffer from it. But everyone must be careful. The disease is transmitted from children to adults through dishes, toys, and damage to the mucous membrane.
This form is characterized by swelling in the oral cavity, redness of the mucous membrane and hardening of the palate, as well as an unpleasant odor, ulceration and cracks. Symptoms of intoxication may appear: vomiting, weakness, rapid pulse.
Other forms of stomatitis
In addition to the above types of disease, the following can also be distinguished:
- chemical stomatitis - occurs as a result of burns to the oral cavity with alkaline substances or acid;
- traumatic - ulcers are formed as a result of impact and disruption of tissue integrity;
- radiation – develops as a result of radiation.
Such forms are non-contagious and therefore do not pose a danger to other people.
Mononucleosis
This disease is also caused by the herpes virus, but not the first type, but the fourth. This virus is also called the Epstein-Barr virus. The virus enters the body through saliva and begins to multiply in the mouth and throat. For this reason, it is very easy to become infected with mononucleosis through a kiss. This disease even has a third name - “kissing disease.” Symptoms of mononucleosis are high fever, sore throat, and swollen lymph nodes. Symptoms do not begin to appear immediately, but after a couple of weeks.
Ways of transmission of stomatitis
Let's summarize. Viral, bacterial and herpetic forms of stomatitis are contagious. Knowing how the disease is transmitted, you can protect yourself and your loved ones. Ways of transmission of infection:
- airborne - sneezing, coughing;
- household items - common dishes, linen, personal items;
- toys, raw pacifiers, rattles;
- dirty hands;
- unwashed food;
- biological fluids - through saliva, blood, breast milk;
- Pets can carry the virus.
It is possible to catch the infection anywhere – from the street to your own home. You can get infected from both a child and an adult.
Cytomegalovirus
This is another member of the herpes virus family. It is very common and in most cases is in an inactive state in the body. Its activation occurs when the immune system is weakened, as well as during stressful situations. The virus is contained in all biological fluids of the infected person, and therefore can easily be transmitted through saliva during a kiss. Cytomegalovirus is especially dangerous for pregnant women, since when infected with it, the child often dies in utero. Surviving children who were infected in utero subsequently develop various abnormalities.
Bacterial stomatitis
The bacterial form often occurs against the background of an underlying disease. Risk factors:
- Pharyngitis.
- Laryngitis.
- Rhinitis.
- Chronic tonsillitis.
- Angina.
When the immune system is significantly weakened, bacteria begin to multiply rapidly. Staphylococcus and streptococcus are common. Bacteria lead to the appearance of a purulent rash. The bubbles open, erosions and ulcers form.
Children transmit the disease to each other through household and contact routes. Toys and personal items become a breeding ground for pathogenic bacteria. One bath towel in a family for several members contributes to the fact that stomatitis will be detected immediately in a brother and sister or in a grandson and grandmother.
Transmission of bacterial stomatitis is not uncommon in children's groups. Adults become infected less frequently. For bacteria to get inside and begin their destructive activity, there must be damage to the skin or mucous membrane.
The slightest scratch may be enough if the body's defenses are reduced. But if an adult has a strong immune system, there is little chance of contracting bacterial stomatitis. The exception is representatives of the older age group. They experience an age-related decline in their defenses.
The likelihood of contracting aphthous stomatitis
People with serious chronic diseases are susceptible to aphthous stomatitis. Most often these are diseases:
- Oral cavity.
- Throat.
- Upper respiratory tract.
The presence of a focus of infection weakens local immunity. The consequence is the appearance of blisters, ulcers, and plaque. A yellow-white coating is characteristic. Erosive changes become pronounced if left untreated.
The disease may not cause concern for a long time. In any disease, with exacerbation of chronic diseases, the eroded surfaces become painful.
The risk of developing aphthous stomatitis increases:
- Poor nutrition .
- The presence of long-term non-healing wounds in the mouth.
- Presence of untreated teeth.
- Gum diseases .
- Incorrectly fitted dentures .
- Oral injuries
Diet for stomatitis
Stomatitis often worries children, becoming a consequence of insufficient immune forces of the body, weakened by some disease.
Aphthous stomatitis is typical for those suffering from diabetes.
Aphthous stomatitis itself is not contagious. Communication with a person who has signs of the disease is not dangerous. The risk of infection arises when a patient with aphthous stomatitis “adds” a viral infection to the underlying disease.
Redness of the throat may indicate pharyngitis, purulent discharge from the tonsils may indicate tonsillitis. In these cases, the pathogen is transmitted to a healthy person through contact with a sick person.
Is it possible to get stomatitis through a kiss?
Young people often don’t think about whether stomatitis is transmitted through kissing, and carefreely kiss their other halves. At the same time, they do not take any measures for treatment, considering this disease to be trivial. Is stomatitis so dangerous that you can’t contact other people?
Stomatitis is an inflammation of the oral mucosa, which in most cases is accompanied by the formation of ulcers. Along with this, swelling of the mucous membrane is observed, and a white or yellow-white coating forms. When communicating, a person feels discomfort, and pain occurs while eating. Increased salivation, gums often bleed, and bad breath appears.
Infection with stomatitis through kissing
The symptoms of the disease are quite different, as are the pathogens. Despite the seemingly complete study of stomatitis, scientists to this day do not know the exact method of its appearance; one version is inclined to believe that stomatitis is a reaction of the immune system to irritating substances unfamiliar to the body that have entered the oral cavity. As a result, the body sends lymphocytes to fight them, and so ulcers are obtained, which clearly indicate the presence of the disease.
In addition, a fungal infection in the mouth can also play the role of a pathogen. In such a situation, kissing is also best avoided.
If we are talking about herpes, it is very easy to catch it by using the patient’s dishes, so during the period of illness it is strongly recommended to maintain personal hygiene and scald the dishes with boiling water. Upon completion of treatment, you should change your toothbrush.
There is an excellent remedy against the herpes (aphthous) form of the disease. The use of acyclovir for stomatitis helps get rid of inflammation and pain.
What if stomatitis cannot infect a partner?
There are situations when kissing does not transmit stomatitis to a partner - for example, if the cause of stomatitis is a gastrointestinal disease, poor personal hygiene, or poor-quality fitting of dentures. But even in this case, it is better to refrain from kissing. After all, the altered microflora of the mouth during stomatitis creates a bad odor from the oral cavity, which is unlikely to please your partner . To eliminate the bad odor, you can use Metrogyl Denta. Plus, Metrogyl Denta helps with stomatitis.
You should first undergo a course of treatment, and then you can move on to kissing. As a rule, the illness does not last longer than 10 days if patients adhere to good personal hygiene and take medications responsibly for topical or internal use.
Prevention of stomatitis
All measures aimed at preventing stomatitis in adults and children coincide with preventive measures against the occurrence of caries and other dental problems. The main recommendations are a healthy lifestyle, adequate oral hygiene and timely visits to the dentist.
We remind you that for preventive purposes you need to visit the dentist’s office once every 6 months - even if nothing bothers you.
We invite you to Genesis for a preventive examination! ←Return to list of articles
Stomatitis in adults
Stomatitis affects the oral mucosa, causing inflammation and the appearance of painful ulcers (ulcers) of varying sizes. If left untreated, erosions can affect the pharynx, tongue, lips and cheeks. The disease mainly affects children, however, among the adult population, the incidence of stomatitis is at a fairly high level - according to WHO statistics, every fifth person experiences the disease. Stomatitis in adults can develop for various reasons, the main ones include:
- diseases of the gastrointestinal tract,
- nerve diseases,
- taking certain medications,
- incorrectly installed dentures,
- avitaminosis,
- allergic reaction.
The risk group also includes people with bad habits and weakened immune systems.
A kiss that tastes like “stomatitis”: is the disease contagious and how is it transmitted?
Stomatitis is a disease that is a lesion of the oral mucosa.
Often occurs as a result of an immune response to the appearance of molecules that are difficult to recognize by the body.
The appearance of such elements causes an attack on lymphocytes, forming ulcers. The body reacts in a similar way to a human organ transplant.
Stomatitis is transmitted through kissing or any other type of contact . The cause of the disease can be a simple lack of oral hygiene.
Ulcers heal within 7-14 days. People who have had stomatitis are susceptible to recurrent illness, however, with a fairly variable frequency. Sometimes the disease appears several times throughout the year, which indicates a chronic form of the disease.
Is stomatitis contagious?
The question of whether stomatitis is contagious should be considered at the level of the root cause of the outbreak of the disease.
Of course, there are contagious types - herpes and candidal stomatitis are especially dangerous. However, each disease is considered by specialists individually.
The following types of stomatitis exist:
- Viral. Generated by viruses caused by diseases such as chickenpox, herpes or influenza. Symptoms include pain in the oral cavity and fever. It manifests itself in the form of the appearance of purulent blisters, which, bursting, form wounds. This type of disease is contagious;
- Bacterial. It affects not only the mucous membrane, but also the gums, palate or sublingual area with the appearance of cracks and bad breath, as well as nausea, dizziness, increased heart rate and general weakness. In most cases, it poses a danger to newborns who do not have a sufficiently developed immune system due to their age. For adults, viral stomatitis is dangerous only through airborne droplets or in the case of sharing cutlery with a patient;
- It is known that about 20% of the population suffers from this disease, of which pregnant women predominate.
Transmission routes
As mentioned earlier, the routes of transmission of stomatitis can be completely different - from airborne droplets to traumatic.
Children often suffer from stomatitis due to poorly developed immunity, which is not yet able to fully cope with surrounding viruses.
Is stomatitis transmitted through kissing?
Prolonged contact with a sick person can also lead to infection with stomatitis.Constant exposure of the oral mucosa to foreign pathogenic microorganisms causes a decrease in the immune system and a reduction in the protective mechanisms of the oral cavity itself.
That is why the transmission of stomatitis through kissing is quite common.
How to protect yourself?
In order to protect yourself from stomatitis, first of all, you must adhere to the rules of hygiene of the gums and teeth.One of the main protective measures is strengthening the immune system through a healthy diet.
Often stomatitis can be caused by a deficiency of B vitamins, zinc or iron in the body.
A preventive examination by a dentist and timely dental treatment are mandatory.
If the infection with stomatitis is permanent, then it is necessary that all family members living with the patient be examined by a doctor.
The cause of frequent stomatitis may unexpectedly be someone from your close circle, without even knowing it.
Causes of stomatitis
Many factors contribute to the development of stomatitis. One of the common causes of the disease is the action of an irritant . The mucous membrane can be affected by constant mechanical trauma (biting the cheeks and tongue, trauma from tartar, incorrectly made prosthesis or crown) [5]. Injury can be caused by exposure to a thermal or chemical agent, for example, when a mucous membrane is burned by hot food or when an allergy occurs to certain foods (for example, citrus fruits) or medications. The risk group includes smokers, since nicotine also acts as an irritant to the mucous membranes.
Oral hygiene plays a major role in the development of stomatitis. With improper oral care, plaque and tartar accumulate; the microorganisms present in them (staphylococci, streptococci) can cause irritation and inflammation of the oral mucosa. As a result, stomatitis occurs as a protective reaction of the body.
Sometimes inflammation of the mucous membrane occurs in various chronic diseases and pathologies with an unclear etiology (cause). Stomatitis can manifest itself in the oral cavity against the background of diseases of the gastrointestinal tract (with helminthic infection), cardiovascular system, blood diseases (anemia), endocrine disorders (diabetes mellitus). Very often, stomatitis develops during HIV infections and can be one of the diagnostic signs when identifying HIV.
Reason/Example
| Fungal infections | ⠀•⠀Candidiasis |
| Bacterial infections | ⠀•⠀Acute necrotic ulcerative gingivitis ⠀•⠀Syphilis ⠀•⠀Tuberculosis |
| Viral infections | ⠀•⠀Chicken pox ⠀•⠀Herpes simplex virus |
| Physical factors | ⠀•⠀Poorly fitting denture ⠀•⠀Improperly made crown ⠀•⠀Improper bite ⠀•⠀Biting cheeks and lips ⠀•⠀Tartar |
| Medicines | ⠀•⠀Antibiotics ⠀•⠀Barbiturates ⠀•⠀Chemotherapy drugs |
| Allergens | ⠀•⠀Occupational exposure to dyes, acid fumes, heavy metals ⠀•⠀Allergic reaction to food |
| Chronic diseases | ⠀•⠀Diabetes mellitus ⠀•⠀Anemia ⠀•⠀HIV infection |
If you notice similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Causes of acute stomatitis
Acute stomatitis occurs most often after damage to the mucous membrane or against the background of a viral disease. Injuries create favorable conditions for the proliferation of pathogenic microorganisms, including the herpes virus. Stomatitis in adults usually has a herpetic form.
Relapses of the inflammatory process usually occur in the cold season, when acute respiratory viral infections, in particular influenza, progress. This coincidence is not accidental. Viral diseases contribute to the appearance of stomatitis in adults and children.
Causes of chronic stomatitis
Chronic stomatitis in the oral cavity regularly worsens. In the summer, a temporary remission is observed. Chronic inflammation is caused by concomitant pathologies of the endocrine system, digestive tract, and diseases of an autoimmune nature. Dental diseases, including caries, periodontal disease, and gingivitis, also contribute to the protracted course of the inflammatory process.
Treatment of stomatitis with folk remedies
Treatment of diseases, especially in the early stages, is possible at home. How is stomatitis in the mouth treated in adults ? Anti-inflammatory and healing folk remedies:
- chamomile with honey;
- burdock root and chicory herb;
- grated raw potatoes (keep in mouth for 5-7 minutes);
- yarrow decoction;
- crushed burdock seeds;
- garlic mixed with curdled milk (or sour cream).
If your body lacks vitamins, you can prepare a vitamin salad.
Burdock leaves, horseradish roots, green onions, sour cream and salt are added to it. Effective treatment of stomatitis at home is possible. The patient must also:
- perform daily oral hygiene;
- follow a diet;
- limit alcohol consumption;
- give up sweets, chips, crackers.
There is a high probability of this disease appearing again. But if you carry out the right treatment, this will not happen.
How to treat stomatitis in children?
Parents who discover ulcers in their child’s mouth are required to contact a pediatric dentist. The following will help prevent the spread of infection:
- limiting contact with other children;
- allocation of separate dishes;
- own personal hygiene items.
The course of therapy consists of taking medications:
- painkillers;
- antiseptic;
- antiviral;
- healing.
How to treat stomatitis in children ? Allowed to process places:
- Oxolinic ointment. Apply 2-3 times daily.
- Acyclovir. The interval between applications is 8 hours.
- Tebrofen gel. No more than 4 times a day.
Pain-relieving ointments can be used. For example, Lidochlor and Kamistad (allowed for 3 months).
Ointments and gels
1. Acyclovir An antiviral drug that has a highly selective effect on herpes viruses. In case of herpes, it prevents the formation of new rash elements, reduces the likelihood of complications, accelerates the formation of crusts, and reduces pain in the acute phase of herpes zoster. The ointment is applied to the affected areas of the skin 4-6 times a day (as early as possible after the onset of infection). Cost: up to 220 rub.
2. Metrogyl denta
A combined antimicrobial drug, the effectiveness of which is due to the presence of two antibacterial components in its composition.
For aphthous stomatitis, the gel is applied to the affected area of the oral mucosa 2 times a day for 7-10 days. The drug is contraindicated in people under 18 years of age. Cost: up to 300 rub.
3. Oxolinic ointment Demonstrates antiviral activity against herpes simplex viruses, herpes zoster, and influenza viruses (mainly type A2). For external use. Non-toxic, non-irritating if the required amount and concentration have been applied and the skin at the application site has not been damaged. Cost: up to 100 rub.
4. Vinilin is a drug that has an antimicrobial, anti-inflammatory, enveloping effect, promotes the cleansing and healing of wounds and ulcers. The antimicrobial effect of the drug inhibits the growth and development of microorganisms. Envelops and regenerates. Vinilin acts as a local anesthetic. Vinylin is usually prescribed by dentists for the treatment of stomatitis, because it has not only antimicrobial, antiviral and antifungal effects, but also healing. A protective film is formed, which protects the wound from irritation upon contact with products, thereby reducing pain. Vinilin does an excellent job of treating stomatitis, but it should be used as prescribed by a dentist. Suitable for any type of stomatitis. Cost: up to 200 rub.
1. Anaferon Lozenges. Immunomodulatory agent. When used prophylactically and therapeutically, it has an antiviral effect. It is used for complex treatment of infections caused by herpes viruses, as well as acute and chronic viral infections. Allergic reactions and increased individual sensitivity to the components of the drug are possible. Contraindications include individual sensitivity to the components of the drug. It is not recommended for use by people with congenital lactose deficiency syndrome. Cost: up to 240 rub.
2. Immunal The drug is in the form of drops for oral administration. Used in cases of decreased immunity, stimulates the immune system in uncomplicated acute infectious diseases. Contraindicated during breastfeeding without prior consultation with a doctor. Cost: up to 340 rub.
3. Givalex Antibacterial and antifungal agent. It has a bacteriostatic and weak bactericidal effect. The drug is in the form of a spray and solution in bottles. It is used as a means for the local treatment of infectious and inflammatory lesions of the oral cavity and pharynx, which are caused by microflora that are sensitive to the action of the drug. It is used to prevent the development of infectious and inflammatory lesions after dental surgery. During pregnancy, use according to strict medical indications. If breastfeeding, use of Givalex should be discontinued. Cost: up to 150 rub.
4. Clotrimazole
Clotrimazole is an antifungal medicine.
Has a wide range of antifungal effects. The active ingredient of the drug is an imidazole antimycotic agent. . This medicine is effective against dermatophytes and yeast fungi. In addition, the drug has an antimicrobial effect. Clotrimazole should not be used if you are hypersensitive (allergic) to clotrimazole, its auxiliary ingredients, or in the first trimester of pregnancy. Cost: up to 360 rub.
5. Ketotifen Ketotifen is produced in tablets and syrup. The main ingredient of the product is ketotifena fumarate. The drug is intended for long-term use. The maximum effect can be achieved only after several weeks of treatment. The average course of therapy can last from 2 to 3 months. Discontinuation of the drug is carried out gradually - from 2 to 4 weeks. Ketotifen is not prescribed to those whose profession involves driving vehicles or potentially dangerous machinery. Cost: up to 100 rub.
6. Tavegil Tavegil in solution for injection is used in the prevention and treatment of pseudoallergic and allergic reactions. Tavegil is not prescribed to patients undergoing treatment with monoamine oxidase inhibitors. In addition, the drug is not prescribed to patients with damage to the lower respiratory system. Cost: up to 200 rub.
Drugs that accelerate the healing of the mucous membrane
1. Vitamin A Has a general strengthening effect, normalizes tissue metabolism, and participates in redox processes. Increases the body's resistance to infection. The drug is taken orally early in the morning or late in the evening, 10-15 minutes after meals, 1 capsule 1 time per day. Long-term daily use can cause intoxication, hypervitaminosis A (headache, nausea, vomiting). Contraindicated during pregnancy and breastfeeding. Cost: up to 100 rub.
2. Sea buckthorn oil Oil preparations always act more gently than aqueous or alcoholic medicinal solutions. This oil can be used if there is no allergy to natural oils. Treatment is carried out by lubricating the areas of erosion a maximum of three times a day. A cotton swab or disk should be dipped in oil and then applied to the mucous membrane. Cost: up to 150 rub.
Anti-inflammatory drugs, antiseptics
Anesthetic (painkiller) drugs dull pain in the mouth for a short time. 1. Hexoral Antiseptic for topical use in ENT practice and dentistry. The drug has a wide spectrum of antibacterial and antifungal effects, in particular against gram-positive bacteria and fungi of the genus Candida. It is prescribed as a symptomatic remedy. The drug is sprayed into the mouth or pharynx, and the affected areas are treated while holding your breath. One injection for 1-2 seconds 2 times a day. The duration of treatment is determined by the doctor. Cost: up to 310 rub.
2. Lidocaine Asept Available in aerosol form. The drug can be used for local anesthesia in dentistry. Apply topically, externally. The dosage varies depending on the doctor's indications. You can also apply it using a cotton swab soaked in it. Contraindications include hypersensitivity to lidocaine. Cost: up to 280 rub.
3. Decathylene Has antibacterial and antifungal effects. Affects microorganisms that cause mixed infections of the mouth and throat. Decathylene does not contain sugar, so it is suitable for people with diabetes. Recommended for aphthous stomatitis. Contraindications – hypersensitivity to any of the substances that are part of the drug. Cost: up to 1300 rub.
Prevention
Prevention helps avoid relapses of stomatitis. First of all, it is worth protecting the mucous membrane from the action of aggressive factors: poor-quality hygiene products, cold or, conversely, scalding food, traumatic dentures and uneven edges of teeth, cigarette smoke, and alcoholic beverages.
Strengthening local immunity plays an important role in preventive measures. The oral mucosa is a protective barrier. If the normal microflora is disrupted, the number of potentially dangerous infectious pathogens increases, they actively multiply and cause a response - an inflammatory process.
To strengthen the immune system, you can use natural factors (hardening with water, sun, air) or natural and artificial immunostimulants.
It is recommended to consume honey in courses, which has antimicrobial activity and functions as a biostimulator. Among medications to strengthen local immunity, it is useful to chew Echinacea tablets and use the drug Imudon.
The presence of bad habits, especially frequent smoking, disrupts the local microflora, irritates the mucous membrane and causes inflammation. Try to gradually reduce the number of cigarettes to give up them painlessly.
Several times a year it is necessary to take courses of multivitamin preparations. Prophylactic treatment usually takes 1-2 months. Pay attention to the quality of your diet. Your daily diet must include vegetables and fruits. Avoid foods that irritate or damage the mucous membrane. Be sure to promptly treat tooth decay and remove tartar at the dentist's office. Carefully choose a specialist who selects the prosthesis and installs it. During the period of adaptation to prosthetics, use the dental gel Cholisal with antimicrobial activity or Metrogyl denta.
Sources:
- https://ProBolezny.ru/stomatit/
- https://stom-info.ru/stomatit/
- https://stomatita.ru/
- https://atvmedia.ru/materials/stomatit-vo-rtu-u-vzroslyh