Purulent-inflammatory infections of the skin and subcutaneous tissue are damage to a certain layer of the skin, subcutaneous tissue with the involvement of nearby tissues (muscle and mucous layers, fascia and parenchymal tissue). The depth of the lesion depends on the number of pathogens, the size of the affected area and the level of the immune system. A common cause of pyodermatosis and purulent wounds is staphylococcal and streptococcal infections. Pseudomonas aeruginosa, Proteus vulgaris, mycoplasmas, Escherichia coli, etc. are less often involved in the purulent process.
What diseases are there?
Staphylococcal and streptococcal infections include:
- boils,
- carbuncles,
- hidradenitis,
- abscesses,
- purulent wounds with damage to the integrity of the skin.
The most common ways of charging are your own skin, skin folds, subungual area, nasopharyngeal mucosa, as well as contact with an infected person. Reduced immunity is a predisposing factor in the occurrence and development of purulent infections.
Boils
A furuncle is an inflammatory process of the hair follicle of the skin. Staphylococcus aureus is the cause of the disease. Clinically, a boil looks like this: the appearance of a pustule in the form of tension and soreness of the skin in the hair area, with redness of the affected area. The affected area has a clear rounded outline and over time takes on a dark purple color with a purulent grain in the middle. The size of boils reaches from 0.5 cm to 1.5 cm. Favorite localization: neck, face and back. But it can develop on any part of the body.
Carbuncles
A carbuncle is the same boil that involves several hair follicles and sebaceous glands in the process. It has many heads with purulent contents. The cause of development is: staphylococci and streptococci. In terms of the size of the skin lesion, the carbuncle is larger (up to 2.5 cm) and clinically develops more clearly. When developing, a multi-headed carbuncle causes fever and general malaise. The favorite localization of the carbuncle is the skin of the back, shoulders and neck.
Carbuncles often give complications in the form of lymphadenitis, thrombophlebitis, meningitis and the development of sepsis.
Hidradenitis
Hidradenitis (otherwise called “bitch udder”) is a purulent inflammation of the axillary sweat glands, as well as the apocrine glands of the perineal region. The routes of transmission of infection are through lymphatic vessels or damaged skin. The clinical picture begins with the development of a dense nodule accompanied by a painful symptom; a pustule does not form at the site of inflammation and there are no necrotic masses. With myomalacia of the affected area, pus comes out in the form of a fistula. If several glands are involved in the process, they merge. Intoxication increases with increasing temperature, malaise, etc.
Abscesses
An abscess is an infectious and inflammatory process involving the skin layers and subcutaneous tissue, with the formation of a purulent “sac”. The causes of abscesses are very different: superficial and deep injuries, hematomas involving secondary infection, post-injection complications, furunculosis, carbuncles, etc. Accompanied by pain in the developmental area, as well as increased temperature and fever.
Purulent wounds
A purulent wound is damage to the integrity of the skin (deep or superficial) with the addition of staphylococcal and streptococcal infections. Wounds of this kind do not have a specific localization due to the spontaneity of the occurrence of injuries of various etiologies (mechanical, chemical or somatic origin).
Purulent diseases of the skin and subcutaneous tissue
Purulent diseases of the skin and subcutaneous fat are the most common purulent diseases (about 30% of diseases in this group). At an outpatient clinic appointment with a surgeon, they account for almost 70%. The most common causative agent of these diseases is staphylococcal flora (70-90%).
The main conditions for the development of purulent-inflammatory diseases of the skin and subcutaneous fat are:
- reduction of local tissue resistance;
- reduction of general resistance and immune defense of the body;
- the presence of microflora in sufficient quantity for the development of the disease.
Furuncle
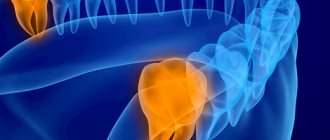
Furuncle is a purulent-necrotic inflammation of the hair follicle and surrounding tissues.
As the process develops, inflammation spreads to the sebaceous gland and surrounding tissues. The causative agent is most often Staphylococcus aureus. Their occurrence is facilitated by: dirt, cracks, skin abrasions, non-compliance with sanitary and hygienic requirements, diabetes mellitus, vitamin deficiencies, hypothermia, etc. Boils do not develop on hairless skin (palms, palmar surfaces of fingers, soles).
Clinic. A pustule with a small inflammatory infiltrate in the form of a nodule forms around the hair root. The skin over the infiltrate is hyperemic and painful on palpation. Boils in the vestibule of the nose, in the external auditory canal are accompanied by significant pain. Necrosis forms at the top of the infiltrate. For 3-7 days. the infiltrate melts, and the necrotic tissues, along with the remnants of hair, are excreted with pus. Boils on the face and scrotum are accompanied by severe swelling, which is explained by the looseness of the subcutaneous tissue. The resulting wound is cleaned, granulated, and a white scar is formed.
With boils in the area of the upper lip, nasolabial fold, nose, suborbital region, a serious condition is possible with the development of progressive thrombophlebitis and transition to the venous sinuses, dura mater, and the development of basal meningitis and sepsis (fever above 40°C, facial swelling, stiff neck).
A furuncle can be single, but sometimes many foci of inflammation appear simultaneously or sequentially one after another in different areas of the skin - furunculosis. The appearance of many boils on a limited area of the body is called local furunculosis, on a large surface of the skin - general furunculosis. Sometimes the appearance of boils in the form of multiple rashes continues with small remissions for several years. This process is called chronic, recurrent furunculosis.
Treatment. Treatment of boils is carried out according to the general principles of treatment of surgical infection. When the boil is localized above the nasolabial fold, antibacterial, detoxification, anti-inflammatory, restorative therapy, bed rest, prohibition of talking and chewing (liquid food) are required. “Squeezing a boil on the face is like death!”
For patients with chronic recurrent furunculosis, in addition to general and local treatment, it is advisable to prescribe nonspecific stimulating therapy in the form of autohemotherapy. Transfusion of small doses of preserved blood, subcutaneous administration of staphylococcal vaccine or autovaccine, immunization with staphylococcal toxoid, γ-globulin are also used. After analyzing the immunogram, immunostimulating therapy aimed at correcting immunodeficiency is indicated. Recently, ultraviolet irradiation and laser irradiation of autologous blood have been widely used.
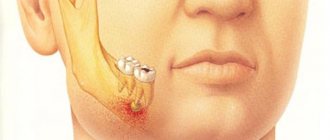
Carbuncle
Carbuncle is a confluent purulent-necrotic inflammation of several hair follicles and sebaceous glands with the formation of general extensive necrosis of the skin and subcutaneous tissue.
The disease is caused by staphylococcus, sometimes by streptococcus. Extensive necrosis forms, around which suppuration develops. The course of the disease is accompanied by symptoms of intoxication. Complications – lymphangitis, lymphadenitis, thrombophlebitis, meningitis, sepsis.
When differentially diagnosing a carbuncle, it is necessary to remember about anthrax carbuncle, which is characterized by a dense black painless necrotic scab in the center, the phenomenon of regional lymphadenitis and severe general intoxication.
Treatment Treatment of carbuncle is carried out in a hospital setting, bed rest is prescribed. Surgical treatment of the purulent-necrotic lesion (with excision of necrosis) is performed under general anesthesia. Antibacterial, detoxification, anti-inflammatory, and restorative therapy are mandatory. If the process is localized on the face - prohibition of talking, liquid nutrition.
Hidradenitis
Hidradenitis is a purulent inflammation of the apocrine sweat glands, which are located in the armpits, perineum, and nipple area (in women).
The infection enters through the ducts of the glands through the lymphatic vessels or through damaged skin. A dense, painful nodule appears in the thickness of the skin. When the latter melts, a symptom of fluctuation is determined, spontaneous opening of the abscess occurs with the formation of a fistula. Merging infiltrates form a conglomerate with multiple fistulas.
Differential diagnosis. Unlike a boil, hidradenitis does not form a pustule or necrosis. Hidradenitis also needs to be differentiated from lymphadenitis, tuberculosis of the lymph nodes, lymphogranulomatosis, and lymphosarcoma. The main difference is that hidradenitis develops in the thickness of the skin, and all types of lymph node lesions develop in the subcutaneous tissue.
Treatment. The main method of treatment is radical surgery to excise conglomerates of inflamed sweat glands. The second component of treatment choice is anti-inflammatory radiation therapy. For recurrent forms, specific immunotherapy and restoratives are indicated.
Abscess
An abscess (ulcer) is a limited accumulation of pus in tissues and various organs.
The cause of an abscess may be the penetration of infection through damaged skin, as a complication of other local infections (furuncle, lymphadenitis, hidradenitis, etc.), as well as metastatic abscesses during sepsis. A feature of the abscess is the presence of a pyogenic membrane, the inner wall of which is lined with granulations.
Clinic. The course of an abscess can be acute or chronic. With this purulent disease, all the typical signs of inflammation are revealed - color, dolor, tumor, rubor, functio lese. An abscess is characterized by a symptom of fluctuation (“fluctuating”). General symptoms depend on the location of the abscess.
Differential diagnosis. Chronic abscess must be differentiated from tuberculous leaks, aneurysm, and vascular tumors.
Treatment of abscesses is carried out according to the general principles of treatment of surgical infection, including surgery and drug therapy.
Phlegmon
Phlegmon is a diffuse inflammation of tissue (subcutaneous, intermuscular, retroperitoneal, etc.).
Cellulitis is caused by both aerobic and anaerobic (usually non-clostridial) microorganisms. According to the nature of the exudate, phlegmons are divided into serous, purulent and putrefactive. The difference between phlegmon and an abscess is the absence of a pyogenic membrane, which ensures a fairly rapid and extensive spread of the purulent process. Clinically, phlegmon is determined by all signs of inflammation.
In case of serous form of phlegmon, conservative treatment is allowed; other forms are treated according to the general principles of treatment of surgical infection.
To avoid purulent skin diseases or to receive professional treatment, you need to make an appointment with a surgeon.
Symptoms and causes, what to look for
Furunculosis and carbunculosis are serious pathological phenomena. Symptoms include general malaise and fever. Over time, the patient's general condition may worsen. Inflammation takes on a wide scale. The necrotic process can involve nearby tissues, penetrating deeper into the subcutaneous tissue and muscles, and pus can spread throughout the fascia. This is fraught with purulent meningitis, peritonitis and sepsis. When pustules with purulent contents appear, surgical intervention is necessary.
Hidradenitis, abscess and purulent wounds do not require delay, but immediate surgical treatment. These infectious diseases quickly cause complications, especially in patients with reduced immunity (patients with diabetes mellitus, lymogranulomatosis, tuberculosis, anemia, etc.).
Treatment methods. Modern methods (opening and drainage of the pathological process)
With a scalpel
Boils, carbuncles, hidradenitis, abscess after pre-treatment with antiseptics are opened using a scalpel, followed by removal of necrotic masses and treatment of wounds with disinfectant solutions. After cleansing, the wound is drained.
CO2 laser
This method is based on carbon dioxide and is widely used in the removal of purulent-inflammatory processes, with minimal burns. After this intervention, the skin does not form scars or depigmentation. This method has virtually no contraindications.
Radio wave method using the Surgitron apparatus
An ideal method for the treatment of boils, carbuncles, abscesses, hidradenitis and purulent wounds. The method is based on the effect of high-frequency waves on the affected area. Bloodlessly removes all pathological tissue with micron precision. After the intervention there is no swelling, redness and no scars.
Local physiotherapy
Local physiotherapy is aimed at increasing the skin's resistance to the infectious agent. The post-operation area, when exposed to physiotherapeutic procedures, quickly forms granular tissue with an obstacle to tissue sclerosis.
Systemic physical therapy (intravenous ozone therapy, ILBI, intravenous ultraviolet blood irradiation)
This procedure is appropriate for repeated furunculosis, carbunculosis and post-infectious complications. Autohemotransfusion using treated venous blood using special technology gives excellent results in case of relapses of pyodermal origin. There is regeneration of blood cells and an impulse to strengthen the immune system.
Purulent wound - symptoms and treatment
An infected wound should be treated immediately. It requires an integrated approach, i.e. it must affect both the wound and the body as a whole.
To combat the causative agent of wound infection, use:
- antibacterial drugs;
- antiseptics (miramistin, chlorhexidine, prontosan, betadine);
- immunological preparations (pentaglobin, gabryoglobin, imbioglobulin).
On the first day, empirical antibacterial therapy (amoxicillin/clavulanic acid, ciprofloxacin) is most often prescribed. Therapy is then adjusted depending on the results of bacterial cultures, taking into account the sensitivity of the identified infection to antibiotics. In addition to antibacterial drugs, patients are prescribed bacteriophages (viruses that selectively kill bacterial cells).
Also, in the case of a purulent wound, a comprehensive detoxification of the body :
- hemodilution - dosed dilution of blood with plasma-substituting fluids;
- accelerated neutralization, destruction and elimination of toxins, metabolites and biologically active substances using forced diuresis (increased urine volume), intravenous administration of solutions and blood purification methods - plasmapheresis, hemofiltration and hemodialysis.
Symptomatic therapy includes pain relief and correction of damaged organs and systems.
In addition to surgical treatment, wound drainage . It allows you to improve the outflow of pus. To do this, various tubes, half-tubes and glove drains are installed in the damaged area.
Hypertonic solutions, hydrogels, proteolytic enzymes in the form of powders or solutions, UHF therapy, various methods of cavitation (ultrasonic exposure), plasma and laser treatment of the wound can be used locally to cleanse the wound. In particular, proteolytic enzymes, acting as a “biological scalpel,” help remove dead tissue from the wound [14].
Treatment of a purulent wound should only be carried out under the supervision of a physician, since the drugs used can cause an allergic reaction [6].
To stimulate regeneration, zinc-containing ointments, vitamins, ultraviolet irradiation, sea buckthorn and rose hip oil are used. The method of applying secondary sutures is also widely used . They are applied only after the wound has been cleansed of pus. To speed up healing and prevent the formation of a hypertrophic scar, it is possible to use a laser, a pulsating magnetic field and electrophoresis with lidase (a special enzyme).
Modern treatment methods include systemic ozone therapy . It improves the utilization of oxygen in the body, has a detoxifying and immunostimulating effect [16].
There are several methods of ozone therapy. The most commonly used in the treatment of purulent wounds include:
- external use of a gaseous ozone-oxygen mixture (direct exposure to a device that supplies ozone to the wound);
- the use of special caps with normal or reduced gas pressure (for example, “ozone boots” - the limbs are placed in a hermetically sealed plastic bag, into which an ozone-oxygen mixture is then supplied at a certain pressure for 15-30 minutes).
Hyperbaric oxygenation (HBO) has also shown good results in the treatment of purulent wounds . It is carried out in special medical pressure chambers: the patient is placed for a certain period of time in a pressure chamber containing oxygen under high pressure. In addition to eliminating tissue hypoxia (lack of oxygen), HBOT suppresses the proliferation of anaerobic bacteria and destroys aerobic bacteria. This method also reduces the formation of toxins and increases the body's immunity.
Dermoplastic surgeries are used:
- with extensive defects against the background of a satisfactory general condition of the patient;
- after cleansing the wound;
- in the absence of inflammation and circulatory disorders in the tissues surrounding the wound;
- when bright granulations appear (young connective tissue with an abundance of blood vessels);
- in the presence of a small amount of serous discharge from the wound;
- when self-healing is impossible.
There is full-thickness skin grafting, which allows you to completely restore the skin, providing good cosmetic and functional results. It is divided into plasty using local tissues and a displaced skin flap (Indian plasty, Italian plasty on a feeding pedicle, as well as microvascular plasty techniques). These methods of surgical wound closure are not always feasible (for example, with extensive soft tissue defects, localization of wounds in sedentary areas of the skin). Therefore, in some cases, plastic surgery with a free split skin flap is used [12]. After this operation, the wound heals through a scar - the skin is not completely restored.
The choice of skin grafting method is carried out taking into account the type and location of the wound, the individual characteristics of the patient, the condition of the surrounding skin and the nature of the tissue.
The modern and most effective method of treating purulent wounds is the VAC (vacuum therapy) method [18]. Due to the effect of negative pressure on the bottom and edges of the wound, it accelerates the formation of granulation tissue, improves local blood supply and reduces swelling. All this promotes rapid wound healing and enhances the effect of drug treatment [20].
Vacuum therapy is carried out as follows:
- to begin with, dead and damaged tissue is completely removed from the wound;
- the cleaned wound cavity is filled with special foam (polyurethane sponge);
- a drainage tube is attached to the surface of the sponge to remove air and exudate;
- to fix the bandage and maintain the vacuum, the resulting structure, together with the edges of healthy skin, is covered with an adhesive transparent film;
- the drainage tube is connected to an aspirator (VAC device), which creates the required level of pressure and draws fluid from the wound [19].
Unlike aseptic gauze dressings, which need to be changed every day, vacuum dressings can be left in the wound for 3-7 days. Due to their tightness, they reduce the risk of new infection [17]. In this case, the destruction and removal of pathogenic microorganisms occurs two times faster than with other methods of treating a purulent wound [20].
Contraindications to vacuum therapy:
- incomplete cleansing of the wound;
- osteomyelitis (inflammation of bone tissue);
- blood clotting disorder;
- malignant tumor in the wound;
- skin fistulas;
- allergic reaction to the components used [20].