What is phlegmon
This is purulent necrotization of soft tissues, which has no clear boundaries. Unlike an abscess, it tends to affect adjacent intercellular spaces. It can occur anywhere in the human body. But the head and neck area is the most dangerous, due to the presence of a large number of blood vessels through which the infection can spread to the brain.
Types of inflammation
Depending on how and why phlegmon arose, inflammation can be primary and secondary. The primary type of phlegmon is an independent disease that occurs due to the penetration of pathogenic microflora into the body, the development of which is accelerated against the background of a weak immune system. Secondary phlegmon occurs as a result of the spread of purulent masses through the soft tissues of internal organs due to a burst boil, abscess and other accumulations of purulent masses.
The incubation period, signs and possible complications depend on the type of soft tissue destruction. There are several types of phlegmon - serous, putrefactive, necrotic and purulent. This type of inflammatory process with the accumulation of purulent masses can spread throughout the body, forming on the muscles, in the abdominal cavity, between internal organs, and under the skin. There is phlegmon of the shoulder, foot, and neck.
Each erysipelas has its own name, depending on its location. It consists of two words - the prefix “para”, which means “about”, and the name of the organ in Latin, in the soft tissues of which inflammation has occurred. For example, phlegmon on the tissues of the rectum is paraproctitis, accumulation of pus between organs in the pelvis is parametritis. An abscess that occurs on soft tissues near the kidneys is paranephritis. The cause of phlegmon on the kidneys is untreated infectious diseases of the genitourinary system, which were accompanied by inflammatory processes.
In the absence of timely treatment in the early stages of the development of purulent inflammation, phlegmon can spread throughout the body, affecting the soft tissues of not only internal organs, but also the thighs, legs, perineum, upper and lower extremities.
How inflammation manifests itself
The symptomatic picture of phlegmon depends on its type. Chronic inflammation does not have pronounced signs in the first stages of development and does not particularly bother a person until the purulent masses have fully matured. In acute phlegmon, symptoms increase quickly, the incubation period lasts no more than a day:
- a sharp increase in temperature up to 40°C;
- fever and chills;
- Strong headache;
- prostration;
- constant feeling of thirst;
- enlarged lymph nodes;
- muscle pain;
- aching joints.
phlegmon of the leg.
The place where purulent masses accumulate, for example, if it is phlegmon of the shoulder, begins to rapidly swell and turn red. Any movement of the limb brings pain, at first slight, and with the development of inflammation the patient is no longer able to move his arm due to severe pain. Upon palpation, phlegmon is easily palpable. The accumulation of purulent masses is a solid, hot formation that does not have clear boundaries. The skin over the site of inflammation begins to become shiny.
As soon as the phlegmon matures, the inflammation bursts. Pus may come out in the form of a fistula (better known as a boil). The danger is erysipelas, when ruptured, the pus does not come to the surface of the skin, but penetrates deeper, spreading to the internal tissues of neighboring organs, causing destruction of the muscular system and bones. With internal infection, the patient experiences:
- severe weakness;
- blood pressure rises;
- shortness of breath, chills, internal heat occurs;
- the condition is rapidly deteriorating;
- pressure drops;
- the pulse is weakly palpable;
- headache increases;
- kidney function is impaired;
- the amount of urine decreases significantly.
In particularly severe conditions, the fingers on the upper and lower extremities turn blue, the skin becomes yellowish due to liver dysfunction.
Causes
In 99% of cases, this disease develops due to dental problems. As practice shows, it is always a consequence of untreated caries. However, purulent melting does not develop immediately. This must be preceded by other pathologies, such as inflammation of the pulp, periodontium, development of a radicular cyst, or osteomyelitis. An obligatory element leading to infection must always be a source with microbial contamination.
Not always purulent-inflammatory processes can lead to the spread of infection. The human body’s immunity plays a huge role. When it decreases, pathogenic microbes in the purulent focus can lead to necrosis of nearby tissues. The head and neck area is rich in cellular spaces that smoothly merge into each other. Therefore, pus can freely move from the lower jaw area down the neck.
The following may be subject to melting:
- Subcutaneous fat tissue;
- Fiber of the intermuscular space;
- Interfascial tissue;
- The lymph nodes;
But there is another factor - an infected wound, which could be the result of injuries. The development of a purulent process is very rarely observed in this case, but with reduced immunity it occurs. Therefore, every wound must be subjected to antiseptic treatment.
Forms of inflammation
With the development of phlegmon, the inflammatory process goes through several stages of formation. The initial stage is serous. With serous phlegmon, fluid—exudate—forms and accumulates under the skin, and leukocytes penetrate into the cells of the adipose tissue. Fatty tissue takes the form of jelly, completely saturated with exudate. There is a gradual spread of inflammation to healthy areas of soft tissue. If treatment is not carried out at this stage, the phlegmon passes into the next stage, putrefactive or purulent. It depends on what type of pathogenic microflora led to inflammation.
The purulent form provokes histolysis (in which the tissues melt and fill with pus). Due to histolysis, fluid begins to accumulate and may be greenish, cloudy white or yellow. The purulent type of neoplasm can lead to ulcers and fistulas. Without timely treatment, inflammation of purulent masses spreads to healthy tissue, cartilage and bones. At this stage of development of the inflammatory process, the muscles become loose, completely surrounded by pus, and appear gray and dirty. There is no internal bleeding.
The putrefactive form of phlegmon is characterized by rapid infection of soft tissues, which begin to deteriorate, and an unpleasant odor emanates from them. The tissues become brownish or greenish, their consistency is slippery and loose. With further development of phlegmon, soft tissues turn into a solid liquid mass. The main symptom of the putrefactive form of inflammation is severe intoxication of the body with a rapid deterioration in the patient’s condition.
Necrotic phlegmon is the death of destroyed soft tissues that are completely affected by purulent masses. If the tissues do not melt on their own, the body begins to reject them. At this stage of development of phlegmon, the inflammatory process begins to localize, multiple foci of abscess are formed, which can be opened independently. If there is too much accumulation of purulent masses that are deep under the skin, it is necessary to surgically open them and install drainage.
Anaerobic is the most severe stage of phlegmon, in which purulent masses infect adjacent healthy tissues, leading to their death, and gas is released. The fabrics have a fetid odor and are dark gray in color. If you press on the phlegmon, you can hear a crunch with which gas bubbles burst. The skin surrounding the source of inflammation becomes soft and loose, there is no redness.
Possible complications
Cellulitis is an extremely dangerous condition of the body, which without proper treatment can lead to severe intoxication and death of large areas of soft tissue. Chronic phlegmon is characterized by the absence of pronounced symptoms. The slow growth of pathogenic microflora allows the body to fight inflammation. During an exacerbation, a thickening occurs under the skin caused by the accumulation of infiltrate, which becomes woody. The skin around the inflammation becomes bluish.
The development of phlegmon on the lymph nodes is especially dangerous. This condition is fraught with the development of blood clots and sepsis. If the inflammatory process has not been completely treated and a small amount of pus remains on the soft tissues, a repeated purulent abscess may occur. Cellulitis that occurs on the face can lead to purulent meningitis.
cellulitis of the century
With further development of phlegmon, during which healthy tissues are affected, purulent arthritis, pleurisy, and osteomyelitis may occur. The most severe complication is the development of purulent arteritis, in which inflammation of the walls of large blood vessels - arteries - occurs, as a result of which the vessel begins to stratify and disintegrate. This pathological process can lead to severe internal bleeding.
Odontogenic phlegmon
The cause of the development of this kind of disease is always a dental problem. Any pathology of the masticatory organs can lead to this outcome.
Problems may arise at the following stages:
- Before tooth eruption;
- At the moment when he is already in the row;
- After removing it.
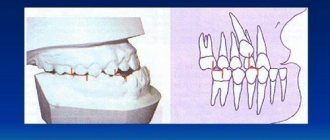
The most common cause of this disease is untreated caries. The pathological process in hard tissues, having gone through certain stages of disease development (pulpitis -> periodontitis), can lead to the development of a radicular cyst. When immunity decreases, it can fester, and then the contents surrounded by the capsule have the opportunity to go beyond its limits.
Wisdom teeth can also cause problems as they are the most advanced teeth and may not have enough space in the row. Having appeared at least half, they become vulnerable to the carious process. Under the gingival hood, which is located above the tubercles, food begins to accumulate. Then cariogenic microorganisms join this substrate and begin to ferment leftover food into organic acids. As a result, a cavity forms in the hard tissues. The wisdom tooth is anatomically designed in such a way that it is very difficult to treat, and if preservation is not practical, then it is better to remove it.
A very rare phenomenon occurs when the disease develops after tooth extraction. The following reasons may contribute to this:
- Part of the organ was left in the socket;
- Food getting into an unhealed hole;
- Permanent injury to the socket with a blood clot, followed by infection.
If any element of the tooth remains inside, then in most cases it will lead to inflammation, since it will be perceived by its own tissues as a foreign body. In addition, local immunity will be activated, which will actively produce lymphocytes. When pathogenic microflora attaches, this phenomenon can spread to nearby tissues. Therefore, it is necessary to remove everything that remains in the hole after tooth extraction.
At first, a person complains of swelling in the area of the extracted tooth and painful opening of the mouth. Throughout the course of the disease, the puffiness of the face becomes more and more. Then, every day the person’s general condition begins to deteriorate. The temperature rises, and blood tests change, which begin to indicate an inflammatory process occurring in the body.
Cellulitis of the floor of the mouth
Oral phlegmon is a diffuse purulent melting of the subcutaneous tissue located between the muscles that make up the floor of the oral cavity. Either one side or both can be affected. This disease is expressed in severe clinical symptoms.
Externally, the patient has a disturbance in the configuration of the face and its asymmetry due to edema. The nearby submandibular and submental areas also have inflammatory swelling. The skin over the purulent infiltrate is hyperemic and does not fold. Nearby lymph nodes are enlarged.
Patients complain of increased salivation, difficulty moving the tongue and lower jaw due to pain. Due to swelling, the tongue does not fit in the oral cavity, so it sticks out slightly. There are teeth marks on its surface. From the outside it seems that the person is thirsty.
The tongue and teeth are coated with plaque, since the patient’s condition does not allow for proper oral hygiene. The composition of saliva also changes, it becomes cloudy and viscous. Body temperature ranges from febrile to pyretic. Depressed or, on the contrary, excited behavior is observed. The general condition of the body is characterized as serious.
The centers of microbial contamination are the lower teeth, and especially the wisdom tooth. The teeth of the upper jaw are not anatomically connected to the area of the diaphragm of the mouth, so they cannot cause this disease. Infection from the upper dentition will only spread to nearby tissues.
Phlegmons of the pterygopalatine and infratemporal fossae
The local symptoms of phlegmon of the pterygoid - palatine and infratemporal fossae are essentially the same, because these 2 anatomical and topographic spaces are widely interconnected.
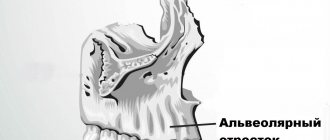
Scheme of localization of phlegmon in the pterygopalatine and infratemporal fossae:
1. head of the mandible
2. inflammatory infiltrate
3. medial pterygoid muscle
Inflammatory infiltrates formed in the infratemporal and pterygopalatine fossae are located between the posterior wall of the maxillary bone and the lateral pterygoid muscle, the lateral plate of the pterygoid process of the sphenoid bone, then spreading along the branch of the lower jaw along the course of the pterygoid muscle. The spread of the inflammatory infiltrate into the pharyngeal fossa, the peripharyngeal space and the infratemporal fossa usually does not occur from here, since the powerful aponeurotic and fascial formations passing here exclude such a possibility.
Phlegmon of the infratemporal and pterygopalatine fossae can be the result of infection of the fiber from the periapical tissues, more often 8I8, less often - 7 6I6 7 teeth. The inflammatory process can spread from other adjacent anatomical and topographic spaces, in particular from the pterygomaxillary, where the most common cause of the development of phlegmon of the infratemporal and pterygopalatine fossae is infection of the hematomas formed here during the vicious implementation of anesthesia of the tissues of the upper jaw. By penetrating deeply into the infratemporal fossa with an injection needle, the doctor easily injures the venous plexus, and the developing hematoma becomes infected. Cellulitis of “injection” origin is formed. Therefore, the sign of a “causal” tooth in the etiology of phlegmon of this localization is relative. The sign of inflammatory infiltrate when examining the patient’s face is weakly expressed or not determined. However, palpation of tissue along the transitional fold of the vestibule of the mouth in the area of the lateral teeth of the upper jaw always reveals infiltration and pain. The infiltrate can spread, descending along the anterior edge of the mandibular ramus. The sign of inflammatory contracture of the lower jaw is expressed due to the involvement of primarily the lateral pterygoid muscle in the process; an attempt at lateral movements to the “healthy side” is unsuccessful. The opening of the mouth may also be limited to some extent.
Thus, with phlegmon of the pterygopalatine and infratemporal fossae, the sign of the “causal” tooth is relative; the sign of inflammatory contracture of the lower jaw is positive due to the involvement of the lateral pterygoid muscle in the inflammatory process, but mouth opening can be maintained in full; the sign of inflammatory infiltrate is negative. There is no sign of difficulty swallowing.
Operative access – intraoral. An incision of the mucous membrane 2-3 cm long is made along the transitional fold in the posterior part of the vault of the vestibule of the mouth. Then, advancing the rasp to the bone, they go deeper into the tubercle of the upper jaw, thus penetrating into the infratemporal and pterygopalatine fossae. After evacuation of the pus, the wound is drained. The prognosis is usually favorable, but one must keep in mind the possibility of rapid spread of purulent exudate to the temporal region, orbit and pterygo-maxillary space.
Putrefactive-necrotic phlegmon of the mouth, or Ludwig's angina
This pathology is similar in appearance to the previous disease, but its main difference is that with soft tissue necrosis there is no accumulation of pus. Symptoms of Ludwig's angina are very specific. This disease carries a huge danger, since sepsis can develop if you do not consult a doctor in a timely manner. Fortunately, the incidence is very low.
The specificity of Ludwig's angina is that basically only the muscles are the main point of damage. The perimuscular tissues may be in a state of inflammation, but it is the muscles that take the main “blow”. Their consistency becomes very dense and woody.
With this disease, patients complain of headaches and high fever. Moreover, in the first two days it may not reach high levels. However, every day the patient gets worse. Externally, a person’s face looks asymmetrical, the chin and neck are swollen. It is impossible to remove the tongue inside as the swelling prevents this from happening. There is a putrid odor and abundant gas formation from the source of infection.
Forecast and prevention of the disease
Active treatment undertaken at the initial stages of the disease contributes to a favorable outcome. True, in the long-term period after suffering from orbital phlegmon, a number of complications may arise: limited eye mobility, secondary strabismus, corneal cataract, amblyopia, optic nerve atrophy.
The spread of purulent infection often leads to panophthalmitis, brain abscess, meningitis or thrombosis of the cavernous sinus, as well as generalized sepsis with a fatal outcome.
Prevention of orbital phlegmon consists of timely sanitation of foci of purulent infection of the facial skin, dental system, ENT organs, and eyes. In case of mechanical damage to the eyes or ingestion of foreign bodies, mandatory local antibacterial therapy is necessary to prevent infectious complications.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic is open seven days a week and operates daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
In our clinic, appointments are carried out by the best ophthalmologists with extensive professional experience, the highest qualifications, and a huge amount of knowledge. The clinic examines and treats adults and children over 4 years of age. Our specialists have developed and are actively using effective programs for the prevention and treatment of eye pathologies.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the online registration form.
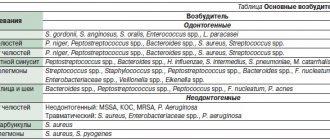
Diagnosis of oral phlegmon
Pathology can be diagnosed through external examination and examination of the oral cavity. The doctor collects complaints and detailed information about what preceded the disease. Visually identifies the source of infection. If the purulent process is located in the superficial layers, then diagnosis is usually not difficult. But if the pus is localized in deep places, then additional clinical and laboratory tests will need to be done. And also carry out microbiological seeding in order to establish the microbial flora. This is necessary in order to prescribe appropriate antibacterial drugs in the future.
Treatment methods for phlegmon of the floor of the mouth
The first place a person comes with this disease is dentistry. Although this is a dental problem, the doctor should send him to the hospital. Since such patients are treated only by maxillofacial surgery.
Treatment of phlegmon of the floor of the mouth combines conservative and surgical methods. If there is pus, it is always necessary to open the source of infection, otherwise it will not resolve on its own. Access for drainage of infiltrate can be made through the mouth or through the skin, here the surgeon starts from where the infection is closest.
The most rational access to the purulent contents is an external incision along the midline going down from the lower jaw. It is safe and cosmetic. The scar remains practically invisible. Then a drain is inserted into the wound for several days. And the causative tooth is removed.
Afterwards, during the recovery period, the doctor must prescribe antiseptic care and antibiotics to eliminate the development and proliferation of microorganisms. In order for the wound to heal faster, vitamins and physical therapy can also be prescribed.
In Moscow, any maxillofacial hospitals, as well as specialized clinics, provide such treatment, each of which has its own price list for such an operation.
Treatment
Despite the severity of the disease, in general, with timely treatment, perimandibular phlegmon has a favorable prognosis. Treatment is carried out only in a hospital setting, but at the initial stage everything is often limited to the use of conservative methods - antibiotic therapy, the prescription of restoratives, vitamins, and a special diet. But if the process has already started and the spread of infection is observed, complex surgical treatment is indicated, which includes the following points:
- opening the inflammation site under general anesthesia;
- cleansing the wound from pus;
- installation of drains for drainage of wound contents;
- daily treatment with bactericidal solutions;
- powerful antibiotic therapy - often a complex of several drugs is prescribed;
- detoxification of the body;
- use of antipyretic and painkillers;
- prescription of immunomodulating, restorative agents, vitamins;
- physiotherapy – ultraviolet irradiation, UHF, magnetic therapy, etc.
If treatment is successful and there are no complications, the patient’s recovery occurs on average in 14-21 days.
What are the consequences
Oral phlegmon can lead to various complications. The most severe consequence will be the development of sepsis. This condition occurs when germs travel through the blood throughout the body, colonizing internal organs. Also, the purulent process through the lymphatic and blood vessels can penetrate through their walls, and then the development of thrombophlebitis of the facial veins is possible. The surrounding tissues also do not remain unchanged. The location of a purulent focus close to the bone can provoke the development of osteomyelitis.
A threatening situation is the development of bleeding due to damage to the walls of blood vessels. Such complications arise when the process is advanced and are much more difficult to treat. Therefore, to avoid such consequences, you must immediately seek help.