Purulent nasal discharge can appear for many reasons and necessarily require treatment. You should not carry out therapy on your own due to the risk of severe complications if treated incorrectly. As soon as purulent discharge from the nose is noticed, you should immediately seek medical help from an otolaryngologist, or, in his absence, a therapist. The fact that pus, and not ordinary snot, began to come out of the nose can be understood by a special, extremely unpleasant odor, which does not occur with a simple runny nose. The yellow-green color of the discharge also differs from the usual one.
The appearance of pus from the nose can be associated with a number of diseases. In order to effectively treat a problem, it is necessary to accurately determine the reason why it occurs. If you seek medical help in a timely manner, the therapy quickly produces positive results and nasal discharge disappears. If for some reason the disease turns out to be advanced, then treatment may take a long time and sometimes require surgical intervention. The appearance of pus from the nose occurs equally in adults and children and requires similar therapy. It is not uncommon for purulent nasal discharge to appear after viral infections as a complication of the disease. In order to prevent this phenomenon, it is necessary to fully treat the primary disease without suffering it on your feet.
When the pus is liquid and white, this is an indicator of the initial stage of the disease. In this case, it is released in large quantities, and also often flows down the back wall of the pharynx. If the particles of pus are viscous and more like lumps, then this is an indicator of severe neglect of the purulent process. Most often, with long-term disturbance, green nasal discharge occurs. The formation of pus is always associated with the penetration of pathogenic bacteria into the nasal cavity. If they are absent, then a purulent process cannot occur. Because of this, in the viral form of rhinitis, the appearance of pus always indicates a secondary bacterial infection.
PUS
PUS
(Latin
pus
, Greek
pyon
) - a cloudy exudate of a yellowish-greenish color, inconsistent consistency, with a cloying, often foul odor. The formation of pus is associated, as a rule, with the impact of pyogenic microorganisms on tissue and is characterized by a complex of vascular-tissue reactions that develop at the site of inflammation and occur with their participation. Purulent inflammation can develop without the participation of microbes as a result of the introduction of turpentine, croton oil and some other chemicals into the tissue. substances. The process of formation of pus is called suppuration.
The liquid part of the exudate is the so-called. purulent serum containing albumins and globulins, almost transparent in the settled Pus. The most characteristic component of Pus are partially disintegrated leukocytes (see), the vast majority are neutrophils. In children's pus, monocytic cells (monocyte G.) often predominate. Sometimes pus consists predominantly of eosinophils (eosinophilic G.). In addition, G. contains dead cells of inflamed tissue and a large number of microorganisms that cause purulent inflammation: bacteria of the pyogenic group (see Pyogenic bacteria), pathogens of typhoid fever, tuberculosis, dysentery, plague, Pseudomonas aeruginosa and Escherichia coli, fungi, etc. Presence in G., proteolytic, amylolytic, and glycolytic enzymes, released during the life and death of microbes, leukocytes, and local tissue elements, determine the peculiarity of purulent inflammation—the ability to melt tissue. G. also contains cholesterol, lecithin, fats, soaps, and DNA.
Phys., Chem. and biol, G.'s properties are not constant. They depend on the nature of the pathogen, the duration of inflammation, the nature of the enzymatic processes occurring in the liver and are largely determined by the general condition of the body (its reactive abilities). Ud. the weight of pus is 1020-1040. Fresh pus has a more liquid consistency; as the inflammation subsides, it becomes thicker, so for a long time the course of inflammation has been judged by its consistency. G.'s color depends on the pathogen and decay products: yellowish - from Staphylococcus aureus and fatty detritus, greenish - from a large number of decaying leukocytes, dirty gray - from the addition of putrefactive microorganisms. The smell of G. depends on the nature of the microflora. Thus, a fetid odor is characteristic of putrefactive (ichorous, putrid) gas, which is formed when bacteria enter the site of inflammation, causing decomposition of tissues with the formation of gases.
The content of microbes is especially high in fresh gland. Subsequently, they undergo bacteriolysis (see) and in old gland they may be completely absent (sterile gland). Pus in a wound (wound G.) in some cases is a product of wound infection by pyogenic microbes and can cause various complications in the course of the wound process; at the same time, an almost pure culture of one or another pyogenic coccus is found in G. In other cases, for example, when a wound heals by secondary intention, the gland is constantly renewed due to the sweating of fluid and leukocytes from the capillaries of the granulation tissue, which is therefore called the “pyogenic membrane.” This G., in which a variety of aerobic and anaerobic flora can be found, plays a large role in the self-cleaning of the wound. The process of suppuration tends to spread along the interstitial crevices, forming streaks, or to be delimited in the form of an abscess. Emptying of the latter can occur spontaneously with the formation of fistulous tracts, but most often the accumulation of G. requires surgical intervention. Sometimes the pus thickens and turns into necrotic detritus that undergoes petrification.
See also Abscess, Purulent infection, Cellulitis, Exudate.
Bibliography:
Davydovsky I.V. General human pathology, p. 392, 415, M., 1969;
Strukov A.I. Pathological anatomy, p. 141, M., 1971; aka, Some modern aspects in the doctrine of inflammation, Arch. pathol., t. 34, no. 4, p. 9, 1972, bibliogr.
I. M. Vertkin.
Causes of purulent vaginal discharge
Gynecological infections
With gonorrhea, thick yellow or green pus with an unpleasant putrid odor is released from the vagina. The amount of purulent leucorrhoea may increase after sexual intercourse. Yellow-green discharge from the vagina is accompanied by pain in the perineum with radiation to the sacrum and coccyx. When the infection spreads upward to the overlying genital organs, abundant purulent, creamy discharge with a characteristic odor is observed, sometimes streaks of blood are visible in it. Other infectious pathologies (mycoplasmosis, ureaplasmosis) may occur with scanty greenish leucorrhoea.
Pathologies of the uterus and appendages
Purulent vaginal discharge is characteristic of severe lesions of the uterus and its appendages - pyometra, pyosalpinx. Women note a constant flow of thick pus from the vagina with a foul odor, in which fragments of necrotic tissue or blood are found. The symptom is accompanied by severe pain in the lower abdomen, fever, problems with urination and defecation. Inflammatory causes of the disorder are endometritis (including postpartum) and endocervicitis, in which scanty purulent discharge is observed.
Bartholinitis
When the Bartholin gland is affected (bartholinitis), patients are bothered by the periodic leakage of yellow or greenish pus with a specific odor from the vagina. In the posterior third of the labia majora, the woman feels a lump; when pressing on it, suppuration intensifies. There may be throbbing pain in the perineum, worsening while walking. Lack of timely treatment and other unfavorable reasons provoke the formation of an abscess of the Bartholin gland, which, when spontaneously opened, produces abundant purulent discharge with a pungent odor.
Rare causes
- Staphylococcal infections of the genital tract
: bacterial vaginitis, cervicitis. - Intestinal-vaginal fistulas.
- Boils and carbuncles of the skin of the perineum
.
There may be explicit images of genitals hidden here.
Are you over 18 years of age?
Yes
No
Purulent discharge from gonorrhea
Diagnostics
Purulent vaginal discharge with an unpleasant odor is a serious reason to contact an obstetrician-gynecologist to find out the causes of suppuration. The examination of patients involves a physical and instrumental examination of the genitals, various laboratory methods aimed at clarifying the etiological factor. The following have the greatest diagnostic value:
- Gynecological examination
. To obtain a complete picture of the disease, examination of patients with purulent leucorrhoea is carried out without preliminary preparation and toileting of the external genitalia. When examined in speculums, accumulations of thick pus can be detected on the walls of the vagina; hyperemia and swelling of the mucous membrane are typical. - Ultrasonography
. Ultrasound of the pelvic organs allows you to find out the reasons associated with purulent vaginal discharge. During standard or transvaginal sonography, the condition of the genital organs is assessed, the accumulation of hypoechoic fluid in the uterine cavity is detected, and signs of an inflammatory process are detected. - Endoscopic methods
. To determine the cause of scanty purulent discharge streaked with blood, colposcopy is necessary for a targeted examination of the cervix and cervical canal. The method helps to identify erosive changes and areas of tissue atypia. - Bacteriological method
. In order to identify the causative agent of a gynecological infection, microscopy of a vaginal smear is performed after staining, then the secretions are cultured on nutrient media. Modern methods - ELISA, RSK, PCR - are intended for rapid diagnosis of the cause of suppuration.
To identify laboratory signs of inflammation, general and biochemical blood tests are done. Serological tests help confirm the etiological factor of vaginal leucorrhoea with a pungent putrid odor. To exclude lesions of other pelvic organs, CT or MRI of the pelvic cavity is used. Diagnostic laparoscopy is prescribed if it is impossible to determine the causes of purulent discharge using other methods.
A vaginal smear examination is carried out to identify the causative agent of infection.
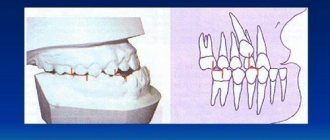
Why gums fester: reasons
1) With an exacerbation of chronic periodontitis , infection in the root canals leads to the formation of a focus of purulent inflammation at the apex of the tooth root. Depending on the type and size of such lesions, dentists call them by terms: granuloma, cyst or granulating periodontitis. You may not be aware of the presence of such foci for years, but sooner or later an exacerbation of chronic inflammation occurs, and then pus-filled abscesses form in the projection of these foci on the gums (Fig. 1-2).
2) Against the background of inflammation of the gums (with periodontitis) - in slightly less than half of all cases when the patient's gums near the tooth fester - the cause is a local or generalized form of periodontitis. Despite the fact that the causes of these two forms of periodontitis are different, the common thing is that the formation of a purulent abscess occurs in a deep periodontal pocket formed between the gum and the surface of the tooth root. Below you can see what an abscess on the gum looks like during periodontitis (Fig. 3).
The causes and treatment of an abscess on the gum will always be interconnected, and therefore, depending on the background of what disease (periodontitis or periodontitis) the suppuration occurred, either treatment of the root canals and the source of inflammation at the apex of the tooth root will be indicated, or treatment of the periodontal pocket using anti-inflammatory therapy , curettage and other methods. Below we will discuss in detail the treatment of gum suppuration in both cases.
Treatment
Help before diagnosis
The discharge of pus from the vagina is a symptom of serious disorders of the reproductive system, for which it is necessary to seek medical help as soon as possible. Self-medication can lead to the spread of the process to other pelvic organs or the peritoneum. Until the reasons for the purulent, foul-smelling discharge are determined, it is permissible to take analgesics to reduce pain. For high febrile fever, antipyretics are used.
Conservative therapy
Medical tactics depend on the prevalence of purulent inflammation, the etiological factor of the disease and the presence of concomitant pathology in the patient. In the acute period, physiotherapy methods are not used; after the main manifestations subside, drug therapy is supplemented with UHF, electrophoresis, and ultraviolet radiation. Local treatment includes instillation of antiseptic solutions (miramistin, chlorhexidine) into the vagina. For sexually transmitted infections, medications are prescribed to both sexual partners. The most commonly indicated medications are:
- Antibiotics
. They are selected taking into account the causative agent of the infection and its antibiotic sensitivity. If severe purulent processes are detected in the uterus and appendages, a combination of 2-3 drugs with a wide spectrum of action is necessary. - Detoxification solutions
. Diseases combined with suppuration are characterized by severe intoxication of the body. To eliminate intoxication, glucose-salt agents are used for parenteral administration. - Immunomodulators
. Medicines increase the overall reactivity of the body, stimulate local immunity, and speed up the healing process. For chronic gonorrhea, a gonococcal vaccine is used for the purpose of immunostimulation.
Is it possible to cure an abscess at home?
Patients with acute conditions are admitted to dentistry without a queue. Therefore, if your health worsens, you should not postpone your visit.
The first question that a patient has is: why does pus appear in the gums and how to treat the pathology? The cause of infiltration is a weakened immune system and non-compliance with dental care measures. At the first symptoms of inflammation, you should immediately consult a dentist. Self-opening of a flux neoplasm threatens the addition of a secondary infection.
It is strictly forbidden to heat the inflamed area. Heat activates purulent-necrotic processes and accelerates the spread of infectious agents.
Timely sanitation of the inflammatory focus in a clinical setting prevents complications.