From this article you will learn:
- what to do if a child has an abscess on his gum,
- Do I need to remove a baby tooth?
- how the treatment is carried out (video),
- how to distinguish a purulent lump from a cyst on a child’s gum.
The article was written by a dentist with more than 20 years of experience.
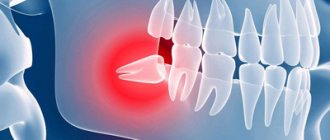
An abscess on the gum in children usually looks like a red or yellowish lump located in the projection of the root of one of the teeth, which caused the inflammation. The inside of such a lump is filled with pus, and it has a yellowish color if the mucous membrane is thin and then the pus shines through it. The appearance of such a lump on the gum above a tooth in a child is always evidence of the development of purulent inflammation at the apex of the roots of a baby or permanent tooth, and indicates the development of apical periodontitis.
Apical periodontitis of primary and permanent teeth in children is most often associated with the lack of timely treatment of caries and pulpitis, as well as with mechanical trauma to the front teeth, for example, due to a fall. Therefore, caries or an old filling can always be found on the causative tooth, and if we are talking about an injury, there may be a chip of the enamel or a fracture of the tooth crown. In cases where the traumatic impact does not lead to damage to the hard tissues of the tooth, the crown of the tooth may be stained bluish or gray.
Abscess on a child’s gum: photo
Immediately before an abscess appears on the gum, children usually complain of pain or discomfort in one of the teeth, which is associated with the formation of pus at the apex of the tooth root. But after a pus-filled lump forms on the gum, children in most cases immediately feel relief (only pressing on the lump with your fingers can remain painful). Next, the lump may spontaneously open with the formation of a fistula, from which pus will leak into the oral cavity, or this may require an incision in the gums.
Important: however, not every lump on the gum indicates the development of purulent inflammation. There are also so-called eruption cysts. For example, even 2-3 weeks before the eruption of a baby or permanent tooth, a cyst may form on the child’s gum, which will have a bluish color (Fig. 7-8). We will also talk about such cysts at the end of the article.
What does a purulent abscess on a child’s gum look like (video) –
A child has a lump on his gum - causes and treatment
This section is very important because... will show how untimely dental treatment, parents ignoring changes in the color of baby teeth or their superficial destruction - leads to the rapid development of periodontitis of the baby tooth, against the background of which a purulent abscess forms on the gum. Usually parents believe that they cannot do anything about it, because... The child still won’t let his teeth be treated. But modern dentistry allows even infants to have their teeth treated under sedation, allowing them to sanitize all their teeth in one visit without fear.
Reasons for the appearance of an abscess/bump on the gum –
- Untreated caries of one of the teeth is the main reason for the appearance of such ulcers. Caries in children occurs against the background of irregular hygiene and constant snacking between main meals. Caries sooner or later turns into pulpitis (at this stage, infection from the carious cavity penetrates into the tooth pulp, causing inflammation in it). Inflammation of the pulp leads to the gradual death of the neurovascular bundle inside the tooth - as a result of which a focus of purulent inflammation develops at the apex of the tooth root (apical periodontitis).
- Poorly treated teeth - in public dental clinics, usually no one will bother with your child, persuading him to be patient while the doctor carefully drills out the carious tissue and puts a filling.
Usually, the maximum that dentists offer to children under 3-5 years of age is the method of silvering teeth. But this method only slows down the development of caries and is not a complete treatment method. In addition, silvering of the same tooth must be carried out repeatedly (after a certain time). As a result, in most teeth treated with the silvering method, first pulpitis (inflammation of the nerve in the tooth) always develops, and then periodontitis.
- Traumatic damage to a tooth is the second most common reason why a lump appears on a child’s gum.
A strong mechanical impact on the tooth (fall, bruise, blow) can lead to the death of the nerve in the tooth, and even to a fracture of the crown or root of the tooth. Dental injuries do not always lead to these consequences; for example, if the blow was not very strong, then everything may well end well. If an abscess has nevertheless formed, and there is no caries or filling on the tooth (in the projection of the abscess), then the obvious reason for the development of purulent inflammation will be mechanical trauma to the tooth. This reason will also be supported if you find mobility of the tooth crown (in the projection of the abscess that has formed on the gum), or a change in the color of the tooth crown - to bluish or gray.
How does a purulent abscess form further?
The formation of a purulent abscess on the gum of a child occurs as follows... In general, periodontitis of the tooth for a long time in a child can be asymptomatic, but with hypothermia or decreased immunity, chronic inflammation at the apex of the root worsens - with the formation of pus at the site of inflammation. The pus tends to come out and therefore it gradually “makes” its way through the bone tissue, first falling under the periosteum of the jaw, where a subperiosteal abscess is formed.
Let us recall that the surface of the jaw bone tissue is covered with periosteum, and only on top of the periosteum is the mucous membrane located. When a purulent abscess is located between the surface of the bone and the periosteum, dentists call such inflammation the term “periostitis.” With periostitis, there will be a characteristic swelling on the gum that is dense to the touch, touching which will be very painful (but there will not yet be a clearly contoured lump with pus).
Next, purulent melting of the periosteum may occur, and then pus enters the submucosal membrane, forming a so-called “submucosal abscess.” The mucous membrane has high elasticity, and therefore a “bump”, soft to the touch, with clear contours, filled with pus (usually painless when touched) is formed on the gum. It should also be noted that in parallel with inflammation of the gums, swelling of the soft tissues of the face, as well as lymphadenitis of the submandibular lymph nodes, can also be observed.
Features of treatment for children with small pimples on the gums
Whatever the diagnosis, dad and mom should be very careful. It is necessary to understand that self-medication of an infant is fraught with dangerous consequences. Once the reasons for the formation of pimples on the upper or lower gums have been accurately determined, the recommendations of the pediatrician should be strictly followed. The treatment method will depend on the diagnosis:
- Plaque must be carefully removed using a regular gauze pad.
- For thrush and infectious stomatitis, it is necessary to eliminate the cause of the disease. Only a doctor can accurately determine the nature of the disease and correctly prescribe medication. It is important to understand that viruses can only be effectively treated with antiviral drugs. To eliminate diseases caused by streptococci and staphylococci, antibacterial drugs will be needed. For fungal infections, antifungal drugs are prescribed.
If white pimples appear on the gums and the baby’s body temperature quickly rises, you need to monitor the water balance and let the baby drink as much as possible. Hot drinks are not recommended; it is better to drink the child with plain clean water. If necessary, you can give your baby an antipyretic, after consulting with your pediatrician. If the dentist diagnoses a malignant tumor, surgical intervention will be required. For Epstein pearls, no treatment is necessary; small spots will go away on their own. To avoid complications and recurrence of the problem, parents should monitor the condition of their children's oral cavity. In the autumn-spring period, children are more vulnerable to colds and viral diseases, which can cause problems.
Real clinical case (baby tooth) –
- In Fig. 4a, you can see that in the projection of the roots of one of the baby teeth of the upper jaw, a purulent lump has formed on the child’s gum. Depending on the degree of filling with pus, the lump can be soft or dense when pressed; in the latter case, pressure will cause acute pain.
- Figure 4c shows an x-ray of the causative tooth that caused inflammation in this case. The area on the radiograph, limited by the white circle, is a zone of purulent inflammation in the area of the roots of the baby tooth. Above this zone we can see the germ of a permanent tooth, which is located almost between the roots of a milk tooth (24stoma.ru).
Important: what to do if the lump bursts...
Sometimes spontaneous opening of a purulent abscess may occur, i.e. the lump can simply burst, and in its place a fistula is formed (Fig. 5). A fistula is usually called a hole in the gum, which through the fistula canal is connected to the source of inflammation at the apex of the root of the “sick” tooth. Purulent discharge will gradually be released from the fistula.
It is important to understand that the opening of a lump and the formation of fistulas does not mean the cessation of inflammation, even if the fistulas also disappeared over time. The inflammation will simply become chronic and will proceed unnoticed until the next decrease in the child’s immunity - after which the inflammatory process will worsen (pus will begin to form again and swelling of the gums will occur).
Treatment
When an abscess appears in the area of a baby tooth, the doctor will first numb the site of manipulation, then open the formation and remove pus from its cavity, after which he will remove the baby tooth, the damage to which caused the development of purulent inflammation. Next, the child will be prescribed a course of antibiotics and rinses.
If an abscess forms over a permanent tooth, the doctor, after examination and local anesthesia, will make an incision in the gum and, if the abscess is very large, install drainage. If the pulp is infected, the tooth canals are opened, depulpation is performed, and then a filling is installed.
Abscess on the gum of a child: treatment
Thus, if a lump or fistula appears on a child’s gum, you should immediately go to the dentist. The strategy for temporary and permanent teeth in this case will be very different, and below we will describe in detail when such teeth can be treated and when they must be removed. If you find it difficult and cannot decide if it is a temporary or permanent tooth, use the tables with the timing of teething in primary and permanent dentition in children.
White pimples on the gums are not a pathology
Only a pediatric dentist can convince worried parents that there is no need to worry and that white spots in the child’s mouth are not an anomaly. Below we consider phenomena that are not dangerous to children's health:
- Bohn's nodules are small whitish formations that appear on the upper or lower gums. They are cysts in nature, but they do not pose a danger to the baby’s health. Over time, the nodules will go away on their own. In some cases, parents may mistake such formations for teeth that are beginning to erupt.
- Epstein's pearls look like small spots and are often located on the palate. This phenomenon also cannot be treated, since it does not pose a threat. The pearl oyster will go away on its own.
Whitish spots may be the remains of food that the baby consumed and then regurgitated. They should go away on their own within a short period of time because they are washed away by saliva. If the plaque does not go away for a long time, this is a reason to contact an experienced specialist.
If the causative tooth is still a baby tooth -
When writing this section, we used the “National Guide to Pediatric Therapeutic Dentistry” (edited by Professor V.K. Leontyev). Let's figure out what parents need to know... The presence of a swelling/bump on the gum, or a fistula, indicates the development of acute periodontitis, or an exacerbation of chronic periodontitis. In the vast majority of cases, baby teeth that have caused the appearance of ulcers on the gums must be subject to mandatory removal. The fact is that in most cases the roots of baby teeth will either not yet be formed or will already have signs of resorption (see photo below).
In both cases, this will not allow for high-quality obturation (filling) of the root canal lumen with filling material. Poor quality filling will certainly lead to the development of purulent inflammation, and in severe cases, sepsis, which even poses a threat to life. Injury to the permanent tooth germ is also possible, both during root canal treatment and as a result of the development of purulent inflammation in the area of the apex of the roots of a baby tooth.
Milk teeth for removal (with signs of resorption) –
But the physiological immaturity of the immune system of children also poses a problem for the treatment of such teeth, which in this situation also contributes to the development of purulent complications. Therefore, to determine the possibility of treatment, we first need a targeted Rg image, which will show the degree of resorption, as well as the presence of foci of inflammation at the apex of the roots of a baby tooth. Below we will list when such teeth require mandatory removal, and in what situations you can try endodontic root canal treatment in baby teeth.
Indications for mandatory removal:
- if there are less than 2 years left before the physiological change,
- if the tooth crown is severely damaged and cannot be restored,
- the tooth has degree II-III mobility,
- in the presence of a fistula tract,
- if the x-ray shows signs of root resorption (we are talking not only about external root resorption, but also about internal one),
- if the image shows a pronounced inflammatory focus of bone tissue destruction (at the apex of the root of a baby tooth), i.e. we are talking about an exacerbation of chronic granulating periodontitis,
- if the child belongs to health groups III, IV, V,
- if the child has caries in the area of most teeth (decompensated form of the carious process).
Possibility of endodontic treatment:
- if the root of the baby tooth is formed and does not show signs of resorption,
- in the absence of tooth mobility,
- in the absence of a fistula tract,
- if the focus of inflammatory destruction at the apex of the root of a baby tooth is very small in size, and at the same time is separated from the permanent tooth germ by a layer of unchanged bone tissue. Filling the canals of a baby tooth (before and after photos) –
Important: you should also take into account that such treatment is very complex and requires a highly qualified pediatric dentist, as well as a large amount of time per patient. Therefore, this is unlikely to be a good idea – if we are talking about public medicine. Also, endodontic treatment will require several visits, and subsequently regular follow-up with radiography (parents must be prepared for this). You also need to consider how important this tooth is in terms of preventing malocclusion.
Filling canals in a baby tooth (video):
In the video below you can see the process of filling root canals in the 1st primary molar. Please note that mechanical treatment of root canals was performed using an endodontic tip and modern rotary files (created specifically for children's teeth). The most modern paste based on calcium hydroxide and iodoform was used as a material for filling root canals in baby teeth. At the end of the video, you will be able to see an x-ray that shows the quality of root canal filling. In this case, I would like to say about the excellent work of the doctor.
A few more things parents should know:
Unfortunately, in recent years, due to the deterioration in the quality of training of doctors, you can hear that many pediatric dentists recommend not removing such teeth, citing the fact that removal will cause malocclusion. And therefore, very often children continue to walk with chronic inflammation at the roots of their baby teeth. In part, the effect of early removal of baby teeth on the bite is true (but primarily only in relation to baby molars, the removal of which can lead to a shift in the rudiments of permanent teeth). But this is not the only thing to consider.
The fact is that the purulent focus of inflammation in the area of the roots of a baby tooth is separated from the permanent tooth germ by only 1-2 mm of bone (Fig. 6). Studies have shown that disruption of the eruption of permanent teeth is caused not only by the early removal of baby teeth, but also by the influence of pyogenic bacteria and their toxins on the rudiments of permanent teeth. For example, you did not remove a child’s baby tooth with inflammation at the apex of the root, and this will also delay the eruption of a permanent tooth. In addition, inflammation at the root of a baby tooth can even lead to the death of a permanent tooth germ (this happens especially often if inflammation occurs before the start of mineralization processes in the permanent tooth germ).
Important: you also need to take into account the effect of a pyogenic infection on the general health of the child. For example, the fact that infection from the source of inflammation will constantly enter the submandibular lymph nodes, causing the development of lymphadenitis. In addition, once in the blood, waste products of pyogenic bacteria affect the entire body as a whole - they increase the risk of developing allergies, bronchial asthma, diabetes, heart and joint diseases.
If purulent inflammation is accompanied by the formation of a fistula, then you must understand that pus will constantly enter the oral cavity through the fistula, the child will swallow it, and this will lead to the colonization of the tonsils with a pyogenic infection and the development of chronic tonsillitis. And in this case, the development of a sore throat or constant regular exacerbations of chronic tonsillitis is guaranteed for the child.
Course of therapy
Moms and dads should understand that buying medications on their own and giving them to infants is strictly prohibited. Many tablets, ointments and gels are contraindicated for children. You can treat your baby only with the drugs that your pediatric dentist recommends. After the baby has eaten, you can give him one tablespoon of clean water, this will help get rid of food residues on the tongue. Before each feeding, the mother should wash her breasts well. It is not advisable to use aromatic shower gels. Also, some doctors recommend that nursing mothers wash their breasts with a weak soda solution. The drug Candide effectively helps with thrush. If the pediatrician determines that the baby has vitamin deficiency, he will prescribe the necessary medications and suggest that the mother reconsider her diet. Such remedies as Nurofen or Panadol will help relieve fever and relieve pain. Acyclovir is popular among antiviral drugs. If the bumps are filled with pus, the doctor will prescribe antibiotics. Among folk remedies, decoctions and infusions of calendula, chamomile and sage work well. Before adding a traditional method to your course of therapy, you must consult with a specialist.
If the causative tooth is permanent –
In this case, the tooth is not only possible, but also necessary to be saved.
If permanent teeth in children have already formed roots, then treatment of permanent teeth with periodontitis will be carried out as in adults. However, treating a permanent tooth with incomplete root formation will present some difficulty, because such teeth may have very wide root canals as well as gaping apical foramina (see photo below). And this poses a great difficulty for high-quality filling. Permanent tooth with incomplete root formation –
Currently, in pediatric therapeutic dentistry, there are 2 main approaches to the treatment of periodontitis in permanent teeth with incomplete root formation. The first method is based on temporary filling of root canals with materials based on calcium hydroxide or calcium oxide. This requires a long, months-long exposure of these materials in the root canals (with periodic replacement of the material with fresh portions). This will narrow the width of the apical foramen by creating an osteocement apical barrier, after which it will be possible to perform permanent filling of the root canals.
The duration of such treatment usually ranges from 0.5 to 1.5 years. If a water-based material with calcium hydroxide is used, then it needs to be changed in the root canals monthly, but if it is oil-based - only once every few months. The disadvantage of this method is the need for frequent repeat visits, and the effectiveness is only about 70-90%, because the emerging osteocement barrier has a loose porous structure and does not guarantee 100% reliable sealing of the root canal lumen.
The second method is a one-step technique for forming a barrier in the area of the apical foramen using materials from the MTA group (mineral trioxide aggregate). An example of such material is “Pro Root”. The method assumes that the apical part of the root canal for 3-4 mm will be permanently sealed with MTA. Thus, in this case, only 1 visit is required, but it is best to use this method only in the last stages of root formation (otherwise, it will be best to combine temporary filling with calcium hydroxide-based material for 1-2 months + subsequent permanent filling with MTA) .
Important:
You must understand that if your child has a lump on the gum or a fistula with purulent discharge, it is useless to self-medicate. No amount of rinsing, application, herbs or even the strongest antibiotics will cope with the source of inflammation at the apex of the root. At best, you will only contribute to the transition of acute inflammation to chronic. Those. if the lump bursts or the fistula closes, all this only indicates a temporary subsidence of the process, which will proceed more imperceptibly, still negatively affecting the germ of the permanent tooth and the entire body as a whole.
Such chronic foci of purulent inflammation are especially dangerous if the child already has concomitant diseases (heart, respiratory organs, joints, etc.). But if there are no such diseases, then the presence of a chronic purulent focus of inflammation increases the risk of many somatic diseases, including lymphadenitis, sore throat, constant exacerbations of chronic tonsillitis and colds.
How to prevent ulcers on the gums - only proper oral hygiene of the child, as well as proper nutrition, can help with this, which will reduce the activity of the carious process in the oral cavity. Read about the age at which you should brush your teeth and how to do it correctly in our article at the link above. The use of additional methods of protection against caries, which include:
- remineralizing therapy,
- fluoridation of teeth,
- sealing dental fissures.
What is that white ball on the gum?
Pimples on the gums, bumps and holes occur for various reasons. The symptoms accompanying the formation are also different. Among the common causes:
- Poor oral hygiene. Even people who brush their teeth twice a day can face the problem. The reason often lies in improper cleaning.
- Unbalanced diet leading to a lack of vitamins in the body.
- Bad habits. Smoking and alcohol are common provocateurs of diseases that occur in the oral cavity.
- Diseases and long-term use of medications (especially antibiotics), which lead to a general weakening of the immune system.
- An allergic reaction to products used for oral hygiene or to food.
- Diseases of the gums or teeth - advanced caries, periodontitis, periodontitis, osteomyelitis or other pathologies.
- Viral infection of the body. Among the most common viral diseases is herpes. Because of it, many small pimples with a white coating appear in the mouth. Most often, a scattering of pimples collects in one place.
Long-term inflammation can lead to deterioration in the fixation of the tooth - it becomes loose and there is a risk of falling out. The inflammatory process is a threat to bone tissue. Chronic acute course can even cause jaw deformation. To avoid such consequences, you can make an appointment with us. Doctor Fedorov’s clinic will help you cope with the most difficult cases.
A cyst on the gum of a child (in place of a tooth that has not yet erupted) –
A bluish-colored cyst on the gum can form 2-3 weeks before the eruption of a baby or permanent tooth (Fig. 7-9). Such a cyst does not at all look like an abscess on the gum, but looks like a lump filled with clear or bluish liquid. When touched, such a cyst is painless. Such cysts are not a pathology of dental development, are not associated with inflammation, and in most cases do not require any intervention (except for periodic examination by parents).
Cyst on a child’s gum: photo
A eruption cyst occurs in only a very small percentage of children. Dentist intervention may be necessary only if inflammation occurs, but this is extremely rare. The addition of inflammation will be indicated by pain when touched, temperature, swelling and redness of the mucous membrane.
If this lump bothers you, you can make a small incision under local anesthesia and release the fluid contained inside. Moreover, if part of the cyst wall is removed, then, as a rule, you can immediately see the upper part of the crown of the erupting tooth (Fig. 9). We hope that our article on the topic: A child has an abscess on his gum, what to do, was useful to you!
Sources:
1. Dental education of the author of the article, 2. Personal experience as a dentist, 3. The European Academy of Paediatric Dentistry (EU), 4. National Library of Medicine (USA), 5. “Pediatric therapeutic dentistry. National leadership" (Leontyev V.K.).
What is the danger of candidiasis and how to prevent it
Babies under the age of six months are especially susceptible to the disease. Fungi from the genus Candida contribute to the development of pathology. Obvious symptoms are the formation of a white coating, which is accompanied by inflammation and the appearance of spots. With severe lesions, the spots may begin to bleed. In their advanced form, the spots resemble a fairly strong and dense film that completely covers the oral cavity. As a result, cracks appear, causing further slight bleeding. On many sites and forums you can familiarize yourself in detail with the pathology from the photo. Babies, when eating and swallowing, experience pain, become lethargic and capricious. The temperature may rise. In case of such damage, it is necessary to show the child to a pediatric dentist as soon as possible. Ways to prevent illness:
- After each breastfeeding, you should give your baby a drink of warm water. The liquid will remove any remaining milk in your mouth.
- Mothers should wash their hands thoroughly and maintain good body hygiene.
- If the disease has already been cured, do not allow it to recur. Regularly treat children's accessories with boiling water.
Preventive measures must be taken to ensure that pimples on the gums no longer appear. Avoid sugary drinks as they can trigger a recurrence of thrush as fungi multiply quite quickly in such an environment.