01.12.2019
Penetration of bones and tooth roots into the maxillary sinus indicates perforation of the latter. A similar complication may be accompanied by treatment at the dentist. Perforation of the maxillary sinus occurs quite often. From this article you will learn the causes of this pathology, signs of perforation, methods of diagnosis and treatment, as well as prevention. Photos of tooth roots in the maxillary sinus can also be seen in the sections of the article.
Reasons for the breakup
The sinus, called the sinus or maxillary sinus, is not characterized by tightness. It interacts with the nasal cavity through a small gap. As a rule, a sinus rupture occurs in the area of its lower part.
This happens due to the characteristic structural features and against the background of certain diseases, namely:
- The roots of molars and premolars are located very close to the sinus. In some cases, the bone layer is quite thick and reaches 1 cm. However, sometimes the barrier can be less than 1 mm in thickness.
- The first and second molars in the root part can be located directly in the sinus cavity and are separated only by the mucous membrane.
- Rapid thinning of the bone layer due to inflammatory diseases in acute or chronic form, including cysts, periodontitis and periodontitis.
- Thin trabeculae of bone in the maxillary tissues.
All these factors can cause a sinus rupture during dental treatment. In this case, there may be no violation of the technology of performing dental procedures. This may be a result of each patient's individual anatomy. Let's figure out why the tooth root penetrates the maxillary sinus.
Causes of perforation.
The dentist is not always to blame for this complication. It can often appear due to the individual anatomical characteristics of the patient. It may also be due to the course of the inflammatory process in the tissue surrounding the root.
The causes of perforation may be the following:
- Perforation of the maxillary sinus during tooth extraction occurs most often. Its bottom is perforated when a tooth is suddenly removed with great force.
- In some patients, the roots of the upper teeth penetrate into the sinus cavity. When teeth are removed, the integrity of the bone plate is automatically violated. During treatment, filling material may enter the cavity.
- For technically complex endodontic treatment. With this type of treatment, the inflammatory focus is located deep in the gums or under the root of the tooth. Instead of removing the diseased tooth, the dentist tries to save it. During this type of treatment, the bone plate is easily damaged.
- In the process of installing an implant in the upper jaw bone with subsequent dental prosthetics, the maxillary cavity can be easily damaged. This is because the implant is similar to a screw and must be screwed into the bone. If there are defects in this manipulation or anatomical and topographical features, the patient’s bone plate of the upper jaw may be damaged (the size of the implant was incorrectly selected, there were defects in preparation for implantation). Before placing an implant, the doctor does not take into account the fact that when a tooth is removed, the thickness of the bone plate quickly decreases.
- Perforation can occur due to chronic inflammation of the tissues surrounding the tooth (periodontitis). With this pathology, the bone plate delaminates and becomes thin. If a tooth has to be removed in such a situation, perforation almost always occurs.
- Carrying out manipulation to remove an impacted tooth from the maxillary cavity.
- Perforation often occurs during tooth root resection procedures. The need for this manipulation arises when extracting a root with a festering cyst.
Frequent cases
Perforations of the maxillary sinus occur, as a rule, as a result of the dentist’s work during dental treatment. Tissue ruptures are typical for the following situations:
- Tooth extraction.
- Dental implantation.
- Endodontic therapy.
- Tooth root resection.
If perforation occurred during a tooth extraction operation, this may be a consequence of unskilled and excessively rough work of the dentist, as well as the individual characteristics of the structure of the maxillary sinus of the patient himself. If the dental roots are located directly in the sinus cavity, perforations during the removal of molars are almost inevitable.
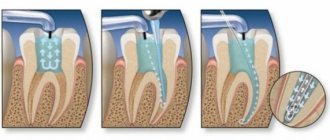
One of the complications during endodontic therapy can also be perforation of the tooth root, which in most cases is associated with perforation of the sinus floor. This situation can occur as a result of excessive expansion of the root canals, as well as when using brute force when installing pins and compacting cement for fillings. In this case, most often not only the root of the tooth may be in the maxillary sinus, but also its fragments and particles of filling material. And this is dangerous for the patient.
When a rupture occurs during installation of an implant or during filling a root canal, as well as as a result of inserting pins into the root of a tooth, this in the vast majority of cases is a therapeutic error by a specialist. Sometimes you can find the roots of a wisdom tooth in the maxillary sinus.
How and why can a tooth end up in the maxillary sinus?
The maxillary sinus is the largest in size of all the sinuses of the nose. Its volume in an adult can reach 10 cubic centimeters. The sinus is a steam room and is located to the right and left of the wings of the nose. Visually, its projection falls on the cheek, which becomes slightly swollen and red with sinusitis.
The oral cavity and maxillary sinus are separated from each other by a layer of bone, which is lined on both sides with mucous tissue. However, both the maxillary sinus and the oral cavity are not hermetically sealed. That is why the appearance of an infection on one side of a thin bone septum (for example, pulpitis) quickly entails inflammation in the adjacent chamber.
There are several factors that significantly increase the likelihood of infection spreading:
- Anatomically, the roots of premolars and molars are located very close to the sinus. The thickness of the bone layer between them in some patients may be only 1 mm instead of the ideal 10.
- In some lucky people, the roots of the teeth are generally located in the sinus itself, being separated from its internal space only by a thin layer of mucous membrane. What to do if your tooth roots are actually in the maxillary sinus? First of all, don't panic! And secondly, carefully monitor their health and regularly take a panoramic photo, which allows you to identify the slightest sign of trouble.
- The bony septum may become thinner over time. This occurs due to persistent inflammatory diseases - periodontitis, pulpitis and others. Therefore, if sinusitis is suspected, timely treatment and removal of teeth, including problematic wisdom teeth, is so important.
- Loose bone tissue as a result of systemic diseases, such as osteoporosis.
Tooth root cyst in the maxillary sinus
Removal of the tooth root is considered the most effective method of treating cysts localized in the apex area. When the patient has not been carefully examined, and the dentist does not have information about the thickness of the bone tissue that separates the cystic wall from the sinus floor, and also in the case when it is necessary to remove a large amount of jaw bone, rupture of the sinus tissue quite often occurs.
Angiofibroma
Benign vascular space-occupying lesion with slowly aggressive growth; localized in the nasal cavity; grows around the posterior wall of the nasal cavity, along the edges of the pterygopalatine foramen; in the early stages penetrates into the pterygopalatine fossa (arrows), grows into the medial pterygoid plate
a rare, but benign tumor characteristic of the nasal cavity and its sinuses. More common in men. As a rule, it occurs on the side wall of the nasal cavity, as well as in the paranasal sinuses. From the nasal cavity, a tumor can grow into the paranasal sinus and vice versa. Patients usually complain of nasal congestion, discharge, nosebleeds, and pain in the facial nerve area. Sometimes bone tissue is destroyed in the area of tumor growth.
Transitional cell papilloma with bone wall remodeling
A formation in the center of the middle nasal meatus, accumulating a contrast agent, spreads into the maxillary sinus and/or cells of the ethmoid bone labyrinth
Symptoms
When perforation and entry of the tooth root into the maxillary sinus occurs during dental resection procedures, characteristic signs of rupture appear, including:
- Bleeding from the tooth socket with small air bubbles, the number of which increases when you try to exhale sharply through your nose.
- Bloody nasal discharge from the side of the ruptured sinus.
- A sharp change in the timbre of the injured patient’s voice, characterized by nasal sound.
If there is a tooth root in the maxillary sinus, the symptoms cannot go unnoticed. Sometimes, after resection, the patient begins to complain about difficult passage of air through the resulting hole, as well as pressure and heaviness in the projection of the maxillary sinus.
When perforation occurs during implantation or endodontic therapy, signs of such a complication include:
- Specific failure of the instrument or material for implantation after some effort to move it into the jaw.
- Changing the position of the instrument used in the resulting wound.
- The appearance of small air bubbles and blood discharge from the hole.
Perforation may not be detected and repaired immediately after a sinus rupture, which leads to infection of the sinus cavity and is accompanied by signs of acute sinusitis or sinusitis.
The following symptoms are typical for such pathologies:
- Acute intense pain in the sinus area of the upper jaw.
- Swelling of the nasal mucosa on the side of the injury, accompanied by difficulty in nasal breathing.
- Discharge of purulent secretion from the nose.
Systemic complications and symptoms of intoxication appear, which are characterized by chills, headaches, weakness and increased body temperature. But how to detect the root of a tooth in the maxillary sinus?
Types of acute sinusitis
There are catarrhal and purulent forms of sinusitis.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
The name “catarrhal” comes from the medical term “catarrh,” meaning “to flow, drain.” That is, with this form of sinusitis, inflammation of the mucous membrane and its swelling develop quite quickly. Initially, the changes affect only the mucous membrane. Inflammation during sinusitis of this form is accompanied by severe swelling of the mucous membrane - it noticeably increases in size and, as a result, a little later transparent mucus forms. Only thanks to timely treatment, it is possible to prevent the transition of catarrhal forms into purulent sinusitis, which with a high degree of probability can become chronic.
With purulent sinusitis, direct contact of pus with the mucous membrane degenerates it, quite quickly and, what is most dangerous, irrevocably. Thus, with improper treatment or no treatment at all, you can very easily and simply join the army of people suffering from a chronic form of sinusitis.
The cause of the purulent form of sinusitis (acute sinusitis) is bacteria. The secreted mucus contains streptococci, staphylococci, and less commonly pneumococci and fungi, which leads to the appearance of purulent contents in the sinus itself.
Diagnostics
For an experienced dentist, specific testing may not be necessary to confirm a maxillary sinus perforation.
If we are talking about tooth resection, then such a complication as soft tissue rupture is accompanied by a typical clinical picture. If the dentist is in doubt when perforation occurs during endodontic treatment, the following additional examinations may be required:
- Probing the hole formed after tooth extraction, as well as the root canal. For this purpose, a thin probe is used. In this way, it is possible to establish the absence of a bone bottom in the wound. During the study, the instrument passes through soft tissues without hindrance.
- Carrying out an X-ray examination of the sinuses. The resulting images will show darkening in the sinus cavity, indicating the accumulation of blood in this area, as well as filling material and fragments of teeth and implant. In some cases, contrast radiography may be required with the introduction of a special substance into the perforation cavity.
- CT scan. This diagnostic method makes it possible to detect ruptures and the presence of foreign bodies. In this case, the image is as accurate and informative as possible.
- If the perforation is old, it is recommended to donate blood for a general examination, based on the results of which it will be possible to draw a conclusion about the presence or absence of an infectious focus in the body.
After carrying out the necessary diagnostic measures and confirming the fact of a rupture of the maxillary sinus, the dentist will prescribe appropriate treatment. So, a person has a tooth root in the maxillary sinus - what to do?
CT and x-ray of the maxillary sinuses
X-ray examination is an effective method for diagnosing the human body, including the condition of the ENT organs. If a person has a stuffy nose, there is discharge from it, or the timbre of his voice has changed, then this is an indication for an examination. X-rays are considered one of the most effective ways to detect sinusitis. With its help, it is possible to diagnose various pathological changes even at an early stage of their development, which is extremely important when prescribing appropriate treatment.
An examination is prescribed if the following symptoms are present:
- Nasal discharge (sometimes with pus).
- Problems with nasal breathing. As a rule, only one nostril is blocked.
- Frequent headaches.
- General fatigue, trouble sleeping and loss of previous activity.
- Nosebleeds.
- Soreness and swelling of the forehead.
If these symptoms are present, the doctor may suspect the presence of an inflammatory process, but it is necessary to determine the exact cause of this inflammatory process, because similar signs exist with polyps and a deviated septum. Therefore, an x-ray of the maxillary sinuses is a mandatory procedure, which allows us to determine the degree of development of the pathology, the presence of neoplasms and other aspects.
Content
- Why do you need an x-ray of the nose for sinusitis?
- How can you see sinusitis on an x-ray?
- How is an x-ray of the maxillary sinuses performed?
- X-ray in childhood
- How to determine sinusitis in an adult patient from an image?
- Computed tomography for sinusitis
- Is it possible to determine sinusitis without a picture?
Why do you need an x-ray of the nose for sinusitis?
Vivid symptoms will help the doctor make an appropriate diagnosis, but without an accurate diagnosis, further treatment will be impossible. It is important to first examine the condition of the sinuses, and then determine the medications and physiological procedures that can get rid of the disease.
When diagnosing, it is extremely important to know what sinusitis looks like on an x-ray. With this examination method, soft tissues are not visible, but bone structures are clearly visualized. If in the picture the shade of the paranasal sinuses and eye sockets is identical, then there is no inflammation. If there is purulent content, then visually it looks like large darkened areas.
An x-ray of the sinuses with sinusitis allows you to determine a number of pathological changes:
- Localization of lesions. They appear as dark spots.
- Presence of cystic formations. They have fairly clearly defined boundaries.
- The inflammatory process and the degree of its development. In the picture they are visible as white spots. Accordingly, the brighter they are, the stronger the inflammatory process.
- Various changes. You can see the level of filling of the nasal sinuses with pus, thickening of the mucous membrane and other pathological changes.
How can you see sinusitis on an x-ray?
Below you see a picture of sinusitis before and after treatment. The radiograph is interpreted by the attending physician or radiologist.
In the absence of pathological changes and abnormalities, the image will show the following information:
- The nose is in the form of a triangle of a light shade, in the middle of which there is a septum.
- On the side of the nasal cavity, the maxillary sinuses are located in the form of triangular clearings with not blurred boundaries.
- Symmetrical arrangement of the nasal passages on both sides of the nasal cavity.
- The frontal sinuses are located above the eye sockets. In the picture they look like clearings of various sizes.
The pathology develops from inflammation of the lateral sinuses. Further, it is localized in the region of the frontal lobes. This will be clearly visible in the darkened areas above the eye sockets and nose. Simultaneous inflammatory processes in the frontal and lateral sinuses indicate not only the presence of sinusitis, but also frontal sinusitis.
A specialist who takes pictures of the nose for sinusitis always determines the condition of the ethmoid bone. Infiltrative fluid often accumulates in the maxillary sinuses:
- mucous;
- catarrhal;
- purulent.
It is quite easy to notice - the liquid appears as a clearly formed white area. This is a clear sign of pathology, which is one of the grounds for making a final diagnosis.
How is an x-ray of the maxillary sinuses performed?
X-ray of the nasal sinuses for sinusitis is a completely standard diagnostic procedure. Before the examination, you must remove all metal objects and removable dentures. If implants, crowns or pins are installed, the radiologist should be notified about this.
To obtain an accurate picture of the disease, a photograph of the nasal sinuses with sinusitis is taken in several projections:
- Chin. Based on this image, the specialist analyzes the actual condition of the maxillary sinuses.
- Nasomental. This projection clearly shows the presence of an inflammatory process in the mucosa.
- Nasofrontal. In this picture you can see the state of the lattice labyrinth.
The examination takes 10-20 minutes, after which the doctor can clearly see the presence or absence of pathology.
X-ray in childhood
Experts agree that X-ray examinations are advisable from the age of 14. Here we are not talking about potential harm to the child’s body, because a single dose of radiation during an examination is absolutely safe for the child. The fact is that at an early age the paranasal sinuses are not yet fully formed, so the examination result cannot be 100% accurate.
In addition, x-rays require maintaining complete stillness throughout the entire examination, which, for obvious reasons, is very difficult to achieve in childhood.
How to determine sinusitis in an adult patient from an image?
Pictures of sinusitis in adult patients are quite characteristic, especially when compared with radiographs of people who do not have this pathology. X-ray will show the following changes:
- The eye sockets and sinuses will be of different shades.
- The presence of infiltrative fluid (a clear white spot against a darkened background).
- Thickened walls and blurred boundaries of the sinuses.
- Cystic formations of varying sizes with clearly defined boundaries.
The only thing that cannot be seen in a photo of the nose with sinusitis is the type of fluid that has accumulated in the sinuses. The study only shows its presence in the form of a white spot, but cannot show what kind of infiltrate (purulent, mucous or catarrhal fluid).
Computed tomography for sinusitis
In some cases, in addition to X-rays, a CT scan of the maxillary sinuses is used. This is a more informative diagnostic method, which has its advantages:
- This is the most reliable way to examine bone structures.
- The result of the study is a three-dimensional image that allows you to view the examined area from different angles and in all planes.
- The procedure takes the least time (when compared with X-rays and MRIs).
- The picture turns out to be as detailed as possible.
- The technique allows you to accurately determine the location and amount of liquid.
When answering the question of what is better to do for sinusitis - CT or MRI, you need to definitely make a choice in favor of computed tomography. This examination can be carried out even in the presence of crowns and implants, which is not possible with magnetic resonance imaging. In addition, MRI has the greatest diagnostic value when examining soft rather than bone tissue.
Is it possible to determine sinusitis without a picture?
If there are significant symptoms, the doctor collects an oral history and conducts an examination. The forehead area and around the nose are palpated for pain. The nasal passages are also examined, the purpose of which is to assess the condition of the mucous membrane.
Based on the manipulations performed, an experienced doctor can diagnose sinusitis without x-rays. But a visual examination does not give a clear picture of the disease, so in order to draw up a competent treatment regimen, it is necessary to take a picture.
X-ray - have been conducting X-ray examinations since 2015. Modern equipment allows you to obtain images of high accuracy and detail. We clearly understand how important diagnosis is for further therapy, therefore we are strict in fulfilling our professional duties.
You can make an appointment with us using the contact phone number listed on the website. Contact us for more detailed advice.
Sign up for a study by phone
+7 (812) 332-52-54
Treatment
The choice of treatment for maxillary sinus perforation depends on the changes that occur as a result of the rupture. Non-surgical treatment seems possible in case of violation of the integrity of the tissues during tooth extraction, when the pathology was detected immediately, and according to the results of the radiographic examination it is clear that there is no infection of the sinus cavity and there are no foreign bodies in it. With such a clinical picture, the doctor, as a rule, tries to preserve the blood clot formed in the hole as much as possible. In addition, preventative measures are taken to prevent wound infection.
For this purpose, a small gauze swab soaked in an iodine solution is inserted into the hole. As a rule, the tampon is self-fixed in the wound cavity. However, sometimes it may be necessary to place a stitch in the gum. Treatment with an iodide solution should be carried out for 6-7 days until the defect disappears and full-fledged granulations are formed. It is not recommended to remove the tampon from the socket during treatment, as this can damage the clot and lead to infection of the wound.
When a tooth root is found in the maxillary sinus, everyone should know what to do. In some cases, the doctor decides to close the defect with a special plastic plate, which is secured to adjacent teeth with clasps. Thus, it is possible to achieve separation of the sinus and oral cavity.
Therapy for perforation of the maxillary sinus during treatment or tooth extraction
If a hole has formed in the sinus after tooth extraction, the doctor will stop the bleeding if possible by forming a blood clot in the hole. To do this, a tampon soaked in medications is inserted into the wound. The patient is advised to rest completely until the perforation heals.
If, during tooth extraction, the maxillary sinus opened, but the doctor did nothing, then inflammation may develop. In this case, if detected, an operation to restore integrity using special plates or artificial bone material is indicated.
Preventing inflammation
In addition to preserving the wound, preventive therapy is carried out aimed at preventing the development of the inflammatory process. Most often, antibacterial drugs and anti-inflammatory drugs are prescribed. In addition, drops are prescribed for instillation into the nasal passages, which have a vasoconstrictor effect. Treatment can be carried out both on an outpatient basis and while staying at home.
If the examination reveals the presence of a foreign body in the maxillary sinus, then treatment is carried out only in a hospital setting. Therapy consists of surgical intervention to open the cavity and remove the tooth root from the maxillary sinus.
Treatment methods for acute sinusitis
The mildest disease does not require the use of any special measures or antibacterial agents for treatment. It is enough to take anti-inflammatory drugs to relieve general symptoms and use vasoconstrictor drops to relieve swelling and facilitate the release of mucus.
Sinusitis with a purulent form is treated with the help of antibiotics (for example, Amoxiclav).
Therapy for the acute form of the disease is best supplemented by rinsing the nasal cavity and paranasal sinuses. The most effective method of treating sinusitis is Proetz lavage, better known as the “cuckoo” method.
Physiotherapeutic procedures and irrigation of the nasal cavity with antiseptic agents will help to consolidate the effect of treating sinusitis.
Complications
Rupture of the maxillary sinus is a serious consequence of dental procedures, the treatment of which most often occurs in an inpatient setting. What is the risk if the tooth root has grown into the maxillary sinus?
Self-treatment of the problem using traditional medicine methods can lead to even more serious complications, including:
- Severe inflammatory process in the sinus cavity with further infection of adjacent tissues. Then osteomyelitis develops in the upper jaw.
- Transition of the inflammatory process to other cranial sinuses, including the sphenoid, frontal and ethmoid.
- Loss of healthy teeth located in the perforation area.
- Formation of foci of pus, phlegmon and abscesses.
Due to the immediate proximity of the brain, and the fact that the tooth root has gone into the maxillary sinus and the latter has ruptured, the occurrence of an infectious lesion of the meninges cannot be ruled out. The next stage of serious complications may be meningitis or meningoencephalitis, which are life-threatening for the patient.
Features of the structure of the maxillary sinus on CT
The shape of the maxillary sinuses resembles a truncated tetrahedral pyramid. On average, the volume of each cavity is 10-13 cm³. The dimensions are not constant and change with the development of the facial skeleton. In a healthy person, the thickness of the mucous membrane of the maxillary sinuses is approximately 1.0–1.5 mm. During inflammatory processes, allergies, and colds, tissues swell and hypertrophy, which contributes to thickening of the walls and a decrease in the volume of cavities. The pathology is clearly visible on CT images of the upper jaw and maxillary sinuses.
The left and right bone cavities are usually symmetrical. But in some patients, examination reveals anomalies, such as the division of the cavity by partitions into several chambers. This structure of the sinus creates certain difficulties in the treatment of sinusitis.
In the CT photo you can see that the maxillary sinuses communicate with the nasal cavity. Mucus is constantly discharged through these anastomosis. In infectious diseases, polyps, tumors and some congenital abnormalities, narrowing of the passages is observed. As a result, the passage of secretion is hampered, and it begins to accumulate in the sinuses, which leads to increased proliferation of microbes and the development of sinusitis.
CT scanning of the upper jaw is valuable not only for studying the structure of the maxillary sinuses. Diagnostics using a computed tomograph makes it possible to study in detail the structure of the alveolar process (the area of the maxillary bone where the teeth are located) and the anatomical and topographic relationship of the roots of the teeth with the bottom of the sinus cavities.
Prevention
As for preventive measures regarding perforation of the maxillary sinus, they consist of following the following rules:
- A thorough and comprehensive examination of the patient before undergoing serious dental procedures, including tooth resection or implantation.
- Correct assessment of the anatomical features of the jaw structure of each patient.
- Strict compliance with all technological requirements for complex dental procedures.
CT scan of the upper jaw with contrast
Native CT examination of the upper jaw accurately diagnoses pathologies in the sinuses, lacrimal ducts and anastomoses with the nasal cavity. With the addition of contrast to the procedure, adjacent soft tissues are clearly visualized.
Most often, contrast is prescribed when malignant processes are suspected. Intravenous administration of iodine-based drugs improves the visibility of the circulatory system: tumors have their own network of vessels, which is clearly visible after contrast. By identifying additional foci of blood supply, computed tomography can detect tumors at an early stage.
Examination of sinuses without enhancement does not require special preparation. It is enough to bring with you a referral from your attending physician, an extract from the outpatient card and the results of previous diagnostic measures. Before a CT scan of the upper jaw and maxillary sinuses with contrast, it is necessary to do a blood test for creatinine. If creatinine levels increase, the use of contrast is prohibited, since there is a high risk of problems with removing the medication from the body.
Other contraindications:
- Individual intolerance to the components of the drug.
The patient may develop reactions to iodine - dermatological (skin redness, rash, itching) or systemic (facial swelling, difficulty breathing, bronchospasm, Quincke's edema, anaphylactic shock). Similar phenomena during CT scanning of the upper jaw with contrast cannot be excluded in people with any serious allergies.
- Taking metformin in patients with diabetes mellitus.
This medication reduces the glomerular filtration rate of the kidneys, which increases the damaging effect of the contrast agent. In combination with iodine-containing drugs, metformin can provoke the accumulation of lactic acid in the body (lactic acidosis). This condition is life-threatening. For patients taking metformin, it is important that two days before a CT scan of the upper jaw with contrast, the endocrinologist either discontinues the drug or replaces it with another medicine.
- Hyperfunction of the thyroid gland.
Iodine-based substances accumulate in the tissues of the thyroid gland, which can significantly worsen the patient’s condition. In this situation, the possibility of examination with contrast appears only after preventive preparatory treatment. In any case, CT scanning of the upper jaw and maxillary sinuses using iodine-containing preparations should not be done without consultation with an endocrinologist.
- Age up to 12 years.
It is difficult for young children to get into a vein, and it is also difficult for children to explain the need and sequence of the manipulations performed.
Lactation is not a contraindication to CT scanning of the maxilla with contrast. But since the dye used partially penetrates into breast milk, a woman should take care of the baby’s nutrition in advance. After the procedure, you must skip two feedings in a row, expressing and pouring out the milk.
How can a complication be identified?
External signs of dental materials getting into the maxillary cavities and patient interview data may not be enough to make a correct diagnosis, and additional studies are carried out to confirm complications of the dental procedure:
- x-ray of the maxillary sinus;
- MRI;
- CT;
- puncture.
The diagnostic plan may include several procedures. Their number is determined by each doctor individually.
How is the treatment carried out?
We respect the patient’s personal time and strive to carry out all activities comprehensively, in one day :
- Professional hygiene Preparation of the oral cavity to ensure sterility during surgery to avoid secondary sinus infection
- Surgery to eliminate inflammation Performed while you sleep; the method of access to the sinus is selected depending on the location of the foreign body and the presence of tumors
- Temporary prosthetics If the causative tooth had to be removed, a temporary crown or immediate prosthesis is installed to mask the defect
Surgical operations in our Center are performed under sedation. The patient does not feel anything, fears and worries are excluded. Sedatives put you into a controlled drug-induced sleep without falling into unconsciousness - this is not general anesthesia! They do not contain toxic components, act gently, preserving reflexes. The artificial lung ventilation device is not connected, hospitalization is not required.
The surgical intervention is completed by a mandatory CT examination , which is necessary to assess the quality of the work performed.
After 10-14 days, the patient is invited to the clinic for suture removal and a control CT image. A schedule of professional inspections is drawn up.
How is a foreign body removed from the maxillary sinus?
To prevent the development of complications in the presence of foreign objects in the maxillary sinus, minimally invasive surgical intervention is performed. Its main purpose is to remove filling material. The operation can be performed using optical instruments such as an endoscope or laparoscope. When carrying out such interventions, significant trauma to bone tissue and incisions is not required. These minimally invasive operations are pain-relieved with local anesthesia and take no more than half an hour. Traditionally, endoscopic techniques are used to remove foreign bodies from the maxillary sinuses. To perform the operation, a small incision is made above the upper lip through which an endoscope is inserted. This optical device helps the surgeon detect a foreign body. The dental material is then removed. When performing laparoscopic surgery, tissue puncture is performed in the place where the bone tissue is thinnest. A special instrument is inserted into the laparoscope, which captures and removes the foreign particle. This technique is used in cases where endoscopic intervention cannot be performed for some reason. Sometimes operations are supplemented by such manipulation as curettage. This method is necessary in cases where, due to the filling material, a granuloma has formed on the tissues of the cavity. After surgical removal of a foreign particle, the patient is prescribed anti-inflammatory drugs to prevent inflammatory and purulent processes. To achieve the desired result, antibiotics, immunostimulants and other drugs may be prescribed. In addition, the affected sinus is washed with antibacterial, antiseptic and anti-inflammatory solutions. To increase the protective functions of the body, the patient is prescribed vitamin and mineral complexes. The best prevention of such complications is regular visits to the dentist. In addition, it is necessary to exclude facial injuries, try to avoid stress, eat right and lead an active lifestyle.
Chronic sinusitis and sinus lifting
The chronic form of the inflammatory process is a relative contraindication for sinus lifting. In some situations, when it is not possible to use alternative methods, the operation is still performed. There is a risk of exacerbation of the infectious process after a sinus lift, but such a complication is rare.
If a patient has chronic inflammation in the maxillary sinus area, the dentist must carefully weigh the benefits and possible risks before setting a date for surgery. During the rehabilitation period, the patient must take strong antibacterial drugs to minimize the risk of exacerbation.
Exacerbation of sinusitis in the postoperative period can lead to implant rejection (if a closed sinus lift was performed). This complication is considered very unfavorable, since the deficiency of bone tissue worsens after removal of the structure. Doctors are not always able to restore bone volume after implant failure, so it is better not to risk the patient’s health again.
Diagnosis of perforation
Having an accurate understanding of the situation in the sinus, the maxillofacial surgeon chooses the correct tactics and method of eliminating the problem
As part of diagnostic activities, our Center carries out:
- X-ray allows you to assess the condition of the causative tooth and the quality of canal treatment
- Computed tomography in ENT mode allows you to get a complete picture of the condition of the maxillary sinuses
The modern Sirona Gallileos CT scanner guarantees high quality images , in which you can determine the location and size of the perforation, identify the presence and localization of foreign bodies, cysts and polyps (if they form), and assess the size of the inflammatory process.
Catarrhal manifestations in the frontal sinuses (frontitis)
Alexey, Ekaterinburg
September 29, 2021
Hello!
Let me start with some background: In February 2022, after ARVI, for the first time in my life I had sinusitis (my upper tooth hurt, my head hurt, my temperature rose to 37.1). I started rinsing with dolphin and furatsilin - then at night the pus came out (yellow snot) and it became easier. the next day I had an appointment with an ENT specialist - he prescribed me Polydex and Sinupret. I drank this and my sinuses no longer bothered me. At the beginning of August 2022, I caught ARVI again, and sinusitis appeared (my cheekbones hurt, I was blowing yellow snot). I didn’t go to the doctor and started treatment as before (washing with Dolphin, Polydex, Sinupret). Again he blew out the yellow snot. Just when I felt good and thought I was cured, the symptoms of ARVI came upon me again. And again signs of sinusitis appeared (cheekbones and upper teeth hurt), plus unpleasant sensations in the frontal sinuses (mild pain, pain in the eyes) were added. This time, instead of Polydex, I used Isofra, plus Sinupret and rinsing with salt water and furatsilin. I couldn’t go to the doctor because on September 7 I was flying to Turkey for 20 days. On the trip, just in case, I took Augmentin and Sinuforte. Upon arrival in Turkey, I used Sinuforte for 6 days - I did not have any yellow (purulent) snot. There I completed the course of isophore, which I started at home (7 days). And I began to feel good, plus every day I washed my nose with sea water from the sea (I swam to the buoys where the water was clean and splashed water into my nose). 5 days before departure, I began to experience symptoms of sinusitis and frontal sinusitis again - my cheekbones and teeth + temples began to hurt, then my forehead and eyes, plus a feeling of malaise appeared. At the same time, I did not feel any manifestations of the virus - my throat did not scratch, I did not sneeze, my eyes did not water, and there was not much snot flowing from my nose. Of course, my nose was periodically stuffy; in general, it seems to me that throughout the entire illness I had swelling in my nose, but breathing was more or less normal. On the day of departure, my temperature rose to 36.9. As a result, I came home and went to the ENT clinic. On the day of admission, I still had the following symptoms - malaise, nasal congestion, discomfort in the frontal sinuses, slight pain in the eyes, mucus running down the throat, the temperature rose to 36.8 (my normal temperature is 36.4). The doctor sent me for an x-ray. X-ray results: Thickening of the mucous membrane of both frontal sinuses. Veiling of lattice cells on both sides. Pneumatization of the maxillary and sphenoid sinuses is not reduced. There are no fluid levels. The nasal septum has a hollow curvature to the right. The mucous membrane of the nasal concha is thickened. Conclusion - Catarrhal manifestations in the frontal sinuses, ethmoid cells. Signs of rhinitis. Diagnosis and doctor's prescription: The doctor said that this is a manifestation of a viral infection. She says she looked at the X-ray and the nose - the surfaces there are pink. She did not prescribe antibiotics, since there was no pus. And she prescribed the following: 1. xylometazoline 0.1 twice a day for 5-7 days; 2. Rinse your nose twice a day with a shower of sea water; 3. Zyrtec 1 time per day; 4. Mometasone furoate 50 mcg, 2 sprays in each nostril once a day for 1 month. The treatment was prescribed on the day I am writing this question. I can’t evaluate the effectiveness. Question for you, dear ENT specialists: Is the treatment prescribed correctly? I myself am against antibiotics and I don’t remember the last time I took them. But it confuses me that the doctor believes that inflammation in the frontal sinuses is a manifestation of viruses, but I have not experienced symptoms of the virus before. What if these are bacteria and the inflammation turns from the catarrhal stage to purulent? How do you think you should take antibiotics? I still have a doctor’s prescription when I contacted him about sinusitis - Augmentin 875 2 times a day for 7 days. Or should I be treated according to the doctor’s instructions and monitor the condition? When should improvement occur? And at what point with this treatment, if there is no improvement, should I start taking antibiotics (for what reason)? Chronic diseases:
Pancreatitis
The question is closed
frontal sinusitis sinusitis