Maxillary sinus surgery is a surgical treatment of the maxillary sinus.
Author:
- Oganesyan Tigran Sergeevich
ENT pathology expert
5.00 (Votes: 2)
Chronic sinus diseases are widespread. Of these, the most common is chronic inflammation of the maxillary sinus - sinusitis.
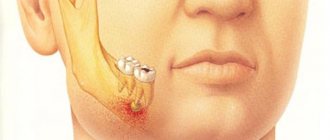
When the disease lasts for a long time - for years, the effectiveness of conservative treatment (punctures, nasal lavage and even antibacterial therapy) becomes less and less effective, and the number of exacerbations increases. The presence of a chronic focus of purulent infection in the upper respiratory tract can provoke complications. Along with exacerbations of sinusitis, a person begins to suffer from bronchitis, tracheitis and even pneumonia. This is called "descending" complications - when the infection spreads to the lower respiratory tract. A general decrease in immunity also plays a major role in this, since any chronic infection forces the immune system to work in an enhanced mode, and frequent antibacterial therapy leads to an increase in forms of bacteria with resistance to drugs. In such cases, when all means have been tried, but it is not possible to eliminate the disease or even reduce its symptoms, surgical treatment is indicated - maxillary sinusotomy .
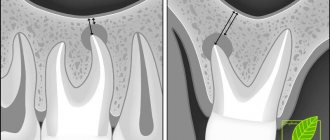
The goal of the operation is to completely remove all affected tissue from the sinus. Since with chronic inflammation the mucous membrane inside the sinus grows rapidly and exceeds the thickness of healthy tissue several times, cysts and polyps can form. An important point of the operation is the revision of the sinus anastomosis. Normally, the maxillary sinus communicates with the nasal cavity through an opening (ostium), which opens into the middle nasal passage. If it works correctly, i.e. is passable for air flow, then when breathing, oxygen enters the sinuses and maintains there an optimal environment for the functioning of the mucosal epithelium and prevents the proliferation of bacteria. Chronically inflamed mucosa can close the anastomosis, thereby maintaining an infection in the sinus cavity. Another reason for the narrowing of the anastomosis can be anatomical features - curvature of the nasal septum, narrowing of the middle nasal meatus due to congenital or acquired enlargement of its structures, for example, the middle concha or the uncinate process.
Indications for maxillary sinusotomy:
- parietal hyperplastic form of sinusitis;
- polyposis-purulent form of sinusitis;
- irreversible changes in the sinus, up to destruction of the bone wall;
- a foreign body in the sinus (for example, filling material that enters the sinus during dental treatment);
- frequent exacerbations of chronic sinusitis (more than 2-3 times a year);
- fungal body in the sinus (occurs as a complication due to long-term antibacterial therapy or the presence of a foreign body).
Brief anatomical summary
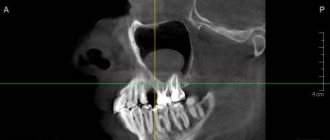
The upper jaw contains the maxillary sinus (maxillary sinus), the alveolar process located under the sinus and a number of other anatomical formations. In the absence of pathology, the roots of the teeth of the upper jaw are tightly fixed in the alveolar process. Normally, between the tips of the roots of the teeth and the sinus cavity there is from 3 to 15 mm of bone tissue.
A fistula is a pathological course formed as a result of an infectious-inflammatory process. Due to the fact that during sinus lifting the amount of bone tissue is reduced, when an infection enters the surgical wound, the soft and hard tissues of the alveolar process and the bottom of the maxillary sinus melt. An oroantral fistula is formed, a fistula connecting the sinus cavity with the oral cavity.
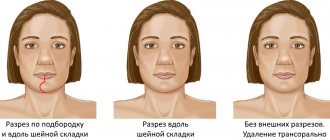
Methods of maxillary sinusotomy
1. Radical surgery on the maxillary sinus according to Caldwell-Luc.
The surgical technique was developed and used by GW Caldwell and N. Luc at the beginning of the last century. To access the sinus, an incision is made under the upper lip, then a fragment of bone is removed from approximately the second to the fifth tooth, resulting in a fairly large entrance to the sinus. This, on the one hand, allows you to freely examine and remove pathologically altered tissues, on the other hand, such an intervention is traumatic - the wound takes a long time to heal, the anterior wall of the sinus remains without a bone wall and the symptoms of inflammation may resume, since the operation does not restore the natural drainage of the sinus. This technique is not currently used.
2. Microsinusrotomy.
A modern and gentle version of the operation. Access to the sinus is also through the front wall (under the upper lip). The hole is formed with a small diameter - about 5-7 mm. A trocar is used for this. This is a funnel with a sharp base that passes through the mucous and bony walls, forming a neat and smooth entrance into the sinus through which an endoscopic camera can be inserted to examine the cavity and endoscopic instruments for removal. This operation is less traumatic due to the ability to use an endoscopic instrument. Therefore, the postoperative period is easy - the patient does not feel pain or discomfort, and the wound heals quickly.
Microsinusrotomy is often performed to remove local sinus formations - cysts, foreign bodies, i.e. when the anastomosis functions well enough and does not need to be expanded.
3. Endoscopic maxillary sinusotomy with access through the nasal cavity.
This operation is indicated for chronic purulent or hyperplastic sinusitis, when the sinus mucosa is changed throughout its entire length. Such conditions are often the result of improper functioning of the sinus anastomosis, to the point that it can be completely blocked. Access to the sinus can be gained through the middle or lower nasal passages, which are located on the lateral (outer side) wall of the nose. Inspection and expansion of the anastomosis is possible only with access through the middle nasal meatus; such an operation will be the most functional and effective. It is worth noting that endoscopic operations require highly qualified operating otolaryngologist and knowledge of the endoscopic anatomy of the nose. At the moment, such operations are the most advanced and modern.
| Methods of maxillary sinusotomy | Complications |
| Radical surgery on the maxillary sinus according to Caldwell-Luc | Damage to the second branch of the trigeminal nerve with subsequent neuropathy |
| Microsinusrotomy | |
| Endoscopic maxillary sinusotomy with access through the nasal cavity | Postoperative bleeding |
Maxillary sinusotomy: how and where it is performed
See also Treatment of ENT diseases Sinusitis Treatment of chronic sinusitis Sinusitis in a child
Sinusotomy is the most effective operation for the treatment of chronic sinusitis. It can be performed using classical surgical instruments, but currently preference is given to minimally invasive endoscopic techniques.
The use of an endoscope allows you to visually control all manipulations, increases the accuracy of the procedure, and significantly reduces its trauma and the level of blood loss. Recovery after endoscopic maxillary sinus surgery is faster and easier than after classical sinus surgery. Patients do not require prolonged hospitalization and can leave the clinic after 2–3 hours.
In the specialized ENT Clinic of Dr. Korenchenko, endoscopy is a key therapeutic and diagnostic procedure. This practice increases the information content of the examination of each patient, minimizes the traumatic nature of manipulations, and increases the effectiveness of treatment even for chronic and complicated forms of sinusitis.
Preparation
Before prescribing a maxillary sinusotomy, the patient is advised to undergo a thorough examination. It includes:
- examinations by a therapist, otolaryngologist, dentist;
- general blood and urine tests;
- coagulogram;
- bacteriological culture of maxillary sinus discharge;
- fluorography;
- ECG;
- radiography of the sinuses;
- CT or MRI of the skull.
Such surgical interventions are usually carried out as planned and are scheduled for the morning. The patient should not eat for 8-12 hours before surgery.
The problems of replacing bone defects in the walls of the paranasal sinuses (NS) and nearby structures of the facial skeleton, increasing the effectiveness of treatment of rhinosinusitis are among the most significant in rhinosurgery.
For a long time, this direction has been one of the priorities in the scientific and practical activities of the Department of Ear, Nose and Throat Diseases and the ENT Clinic of Rostov State Medical University, which was started by the founders of the Rostov School of Otorhinolaryngology - Professors A.R. Khanamirov and A.N. Pomukhina. Preservation, comprehension and enhancement of their creative heritage is the main component of the scientific, clinical and educational work of their students and associates. In this article, we presented a generalized view of the main stages in the development of methods of surgical treatment of various diseases of the urinary tract, previously used and developed at the Department of Ear, Throat, Nose Diseases of Rostov State Medical University at the present time.
The most ancient plastic surgical techniques in otorhinolaryngology were attempts to treat atrophic rhinitis and ozena by changing the laminar movement of air in the nasal cavity to turbulent one by transforming the sizes of various anatomical formations of the nasal cavity [1]. To do this, surgeons injected a variety of materials under the mucous membrane of the inferior turbinates and/or mucoperichondrium of the nasal septum: auto-, homo-, or heterocosity; soft tissue structures: dura mater, peritoneum; natural human adaptogens.
Various methods and techniques of plastic surgery, including rhinosurgery, are used to replace, connect or restore damaged structures and tissues. During operations on the ED, the plastic part of the intervention consists in the formation of pathways for the outflow of pathological and postoperative wound contents from them, the restoration of bone or soft tissue defects and, ultimately, the preservation of the structure and function of the ED.
For a long time, the task of forming the frontonasal anastomosis at the final stage of extranasal opening of the frontal sinus was very relevant. Creating pathways for the outflow of contents from the operated frontal sinus, and often from other SNPs involved in the inflammatory process, as well as the anterior cranial fossa, was a rather complex problem, since the newly created frontonasal anastomosis passes through a number of anatomically and functionally important bone structures of the skull, causing their deformation or destruction. At the same time, an obligatory element of the management of the postoperative period in such patients is to ensure a complete epithelial lining of the newly created frontonasal canal, which takes 28-35 days.
When forming the frontonasal anastomosis, some surgeons displaced flaps of the mucous membrane from the frontal sinus, the lateral wall of the nose, and the oral cavity [2].
Many authors sought to form a persistent anastomosis with the help of tubular drainages, which were introduced into its lumen for the period of complete epithelialization. To achieve this goal, a variety of materials were used: noble varieties of wood, glass, rubber, gold, tantalum, vitalium - an alloy of cobalt, chromium and nickel [3-5].
The creation of polymers made it possible to use their best qualities: biological inertness, plasticity, ease of processing and sterilization. Drains were made from plastics - polyethylene, teflon [6], silastic, silicone, hydroxyapatite, etc. [7] for insertion into the newly formed frontonasal anastomosis. Some authors used tubular endoprostheses made of biocompatible polymer materials containing antimicrobial drugs (dioxidine, quinoxidine) and substances that promote regeneration and epithelialization [5].
Tubes made from all these materials were inserted into the formed anastomosis for various periods: from 7-8 days to 4 years [8].
However, despite a fairly diverse range of materials for tubular drainages, the incidence of disease relapse remained at a fairly high level: up to 20% in the first 3-4 years after the intervention. The development of cicatricial stenosis of the formed frontonasal anastomosis was facilitated by both the extensive wound surface, the retraction of the soft tissues of the lateral wall of the nose and orbit into its lumen, and tissue irritation by the material of the drainage tubes [9].
In the early 70s of the last century, tissue auto-, homo- or heterografts began to be used on a dense basis of tubular drainage in order to fix soft tissue material to the walls of the formed anastomosis. A.G. Likhachev proposed a skin flap as a tissue fragment, N.P. Omelyanenko et al. — collagen, V.T. Zholobov - heterogeneous formalized peritoneum of cattle, V.A. Skorobogaty - the umbilical cord of the fetus [6, 10-12].
A combined drainage was inserted into the anastomosis for 28-35 days, and after the formation of a stable canal, it was removed through the nose. According to a number of authors, the number of relapses of the disease decreased somewhat, but remained quite high. It was found that the growth of granulations occurred from the area of the scar formed at the site of duplication of the leaves of the soft tissue fragment on the wall of the frontonasal anastomosis [13].
We, together with A.N. Pomukhina used a continuous closed homograft, which is a natural conductor of fluid in the human body - the femoral artery, as a tissue component of the combined drainage tube [14].
The preparation of the frontonasal anastomosis was carried out carefully, smoothing out the unevenness of the bone surface for a complete fit of the graft. After the formation of the frontonasal anastomosis, a fragment of the femoral artery equal to the diameter of the tube was placed on a Teflon drainage tube. The artery was stretched due to the elasticity of the vessel wall. On the proximal part of the vascular prosthesis, 3-4 incisions were made with scissors vertically downwards, 5-10 mm long, forming “petals” (Fig. 1). Then a combined drainage tube was inserted through the nose into the formed frontonasal anastomosis. The “petals” of the vascular prosthesis were straightened at the mouth of the formed canal, funnel-shaped, moved to the sides and fixed with tissue glue to the walls of the sinus. After installation of the prosthesis, the upper section of the Teflon tube, 2-3 mm long, protruded into the lumen of the sinus. This fixation of the combined drainage tube ensured its stable position in the anastomosis and good outflow of wound discharge and exudate. After epithelialization of the anastomosis, the Teflon drainage tube was easily removed, and the vascular fragment became part of the wall of the frontonasal canal. The smooth and even endothelium of the vessel, being the wall of the anastomosis, retained the original lumen of the newly formed frontonasal canal for a long time and ensured good drainage and aeration of the sinus. The proportion of disease relapses after intervention with the formation of the frontonasal anastomosis using the described method did not exceed 0.8% [15].
Rice. 1. Combined drainage tube (according to A.G. Volkov and A.N. Pomukhina, 1981), intended for plastic surgery of the frontonasal anastomosis using the human femoral artery.
After the introduction of gentle endonasal surgery techniques and instruments for their implementation into clinical practice, the method of forming an anastomosis in this way is rarely used and only with massive radical interventions. At the same time, the use of endonasal surgery methods makes it possible to reduce the degree of invasiveness of the intervention and involves extranasal stages of the operation to restore the full functioning of the structures of the nasal cavity and the SNP to improve their drainage [16].
For a long time, the ENT clinic dealt with the problem of treating an extremely severe pathology - chronic diffuse osteomyelitis of the walls of the frontal sinus (CDOSLP), which is characterized by the presence of a purulent-necrotic focus in the bone, long-existing and, as a rule, not prone to self-healing. We have already written in detail about this disease earlier [15, 17] and noted that with osteomyelitis, the entire bone structure is involved in the inflammatory process with the formation of panostitis, a significant role in the occurrence of which belongs to thrombophlebitis of the veins of the mucous membrane, and subsequently the veins of the bone marrow, periosteum and dura mater [18, 19]. In contrast to local destruction, most often of the lower wall with the formation of a fistula, CDOSLP is characterized by chronic diffuse inflammation affecting all layers of the bone [15, 19]. We divided the methods of surgical treatment of CDOSLP into two types: the first type - with preservation of the air sinus and the formation of the frontonasal anastomosis; the second type is surgical obliteration of the sinus. Both with the first and second types of operations, a significant number of postoperative relapses of the disease were noted, which, according to W. Bosley [20], account for more than 50% of the total number of patients and are an indication for repeated interventions on the frontal sinuses with an external approach and unfavorable outcomes [19, 21, 22].
There are many reports of failure of frontal sinus obliteration despite careful removal of the mucosa [23].
We have proposed a method for treating patients with CDOSLP, the main element of which is open wound management with filling it with tampons impregnated with an oxygenated protein-antibiotic complex (OPAC), consisting of chicken egg white and a targeted antibiotic solution. This method of treatment is based on the direct effect on the tissues of all components of this natural protein preparation with oxygen dissolved in it. As was shown by A.E. Rauer and other authors [24, 25], when a drug is administered locally, its concentration in inflamed tissues is several orders of magnitude higher than in the same tissues when the same drug is administered intravenously.
Chicken egg white is a 10% aqueous solution of protein substances and contains egg albumin, conalbumin, ovomucoid, globulins, ovomucin, avidin, enzymes: lysozyme, catalase, phosphatase, di- and polypeptidases, tributyrinase, proteinase, diastase, oxidase. It stimulates phagocytosis, having a pronounced bacteriostatic effect [26], interrupts the growth of pathogenic fungi, and enhances the perception of antimicrobial drugs by microorganisms [27].
In the ENT clinic of Rostov State Medical University in the period from 1980 to 1998, we observed 25 patients with CDOSLP aged from 17 to 67 years. There were 24 men, 1 women. In 12 patients, the disease developed as a result of trauma to the frontal region, in the rest - due to inflammation of the frontal sinuses or as a result of surgical intervention on them.
From this point on, we began to talk about chronic diffuse osteomyelitis of the frontal bone (CDOLK), and not about CDOSLP, since the inflammatory process can spread beyond the anatomical boundaries of the frontal sinuses.
Before admission to the clinic, all patients underwent from 2 to 6 operations on the frontal sinuses with an extranasal approach and unsuccessful attempts to maintain their pneumatization. Relapses of the disease occurred within 2 months to 1 year after the intervention. 5 patients had extensive skin defects of the frontal region and scar changes in nearby soft tissues.
To prevent relapses of the disease, we have developed a set of treatment measures, including the following stages:
1) extranasal opening of the frontal sinus;
2) removal of the pathological contents of the frontal sinus, including osteomyelitic foci, within healthy bone tissue;
3) obliteration of the frontal opening of the frontonasal canal;
4) application to the mucous membrane of the nasal mouth of the frontonasal canal of a 10-20% solution of silver nitrate for 10-12 days of the postoperative period;
5) daily loose tamponade of the postoperative cavity with gauze turundas soaked in OBAK.
The sanitizing surgical intervention was completed by monitoring the radicality of bone tissue excision under a microscope. This measure is necessary, since areas of the changed bone are difficult to distinguish from healthy tissue with the naked eye, and in 12 patients, as already noted, the process spread beyond the frontal sinuses. The intersinus septum was examined especially carefully and, if there was the slightest damage, it was resected. If there was any doubt about the completeness of removal of pathologically altered bone tissue, the wound was widened. This approach coincides with the opinion of surgeons who have experience in operations for CDLD and who recommended that limited skin incisions and small burr holes in the walls of the sinus should not be used [28].
In our opinion, in the postoperative period in patients with CDLD, the wound should remain open, since there are blood clots and wound exudate on the surface of the bone, and in a closed cavity it is impossible to ensure full trophism of the bone and soft tissues and to carry out dynamic control over reparative processes. This is why the coronary neurosurgical approach to the wound [29], in our opinion, is not acceptable for the treatment of patients with CDLD.
In our proposed treatment method [30], much attention is paid not only to surgical techniques, but also to the local effect of chicken egg white on the tissue of the frontal sinus and frontal region. Bactericidal and local stimulating effect of chicken egg white, according to A.A. Yarosh [31], is best achieved by introducing it on tampons with the addition of antibiotics. The presence of only one of the components of chicken egg white - native lysozyme - has an active anti-inflammatory effect, improves the growth of granulations, and accelerates healing [32].
We developed a tool and an original method for preparing OBAK, the foamy mass of which was impregnated with wide tampons and loosely placed, filling the lumen of the sinus. The formation of young granulation tissue led to a gradual decrease in the volume of the frontal sinus and, accordingly, the number of inserted tampons with OBAK. A gradual decrease in the lumen of the frontal sinus with its replacement by granulation tissue from the periphery to the center caused its obliteration. This method, which we called secondary obliteration, for small and medium-sized frontal sinuses, as a rule, guaranteed the absence of relapse of the disease. Subsequently, we came to the conclusion about the need for biological tamponade of the sinus lumen [15], since we believe that primary biological obliteration of the frontal sinuses in case of CDLO, orbital and intracranial complications is contraindicated.
We soon became convinced that with large sizes of the frontal sinuses, the time frame for their complete obliteration can be significant, but justified by the reduction in the risk of relapse of the pathological process.
Attempts to reduce the treatment time for this severe group of patients without reducing its quality made it possible to justify the need to use a two-stage method [33]. At the first stage, open wound management was carried out with daily change of tampons with OBAK until the walls of the sinus were evenly covered with granulation tissue. At the second stage, surgical obliteration of the formed cavity was performed with a subcutaneous fat autograft with the application of a secondary suture to the wound of the frontal region.
In the early postoperative period, dressings were performed in the described manner until the walls of the sinus were completely and uniformly covered with granulation tissue. The use of OBAK along with sanitation of the pathological focus and removal of tissues affected by the osteomyelitic process eliminated the accumulation of exudate in the sinus cavity.
To prevent the development of mucocele and purulent inflammation in the operated sinus [22], we constantly monitored the condition of the frontonasal canal (or postoperative anastomosis) so that its obliteration occurred evenly, without the formation of pockets or cavities, removing excess granulations. In 12 patients, upon completion of the extranasal opening of the frontal sinus, a spherical electrode inserted into the lumen of the frontonasal canal (or anastomosis) was used to diathermocoagulate the mucous membrane invaginated from the frontal sinus, which accelerated and improved the process of its obliteration.
The method of the second stage of treatment of patients with CDLD was as follows: after completion of the process of granulation of the walls of the frontal sinus, before the intervention, the surface layer of granulation tissue was scarified with the removal of areas of its excess growth. Then a subcutaneous fat graft was prepared from the anterior abdominal wall or gluteal region of the patient, the size of which was 25-30% larger than the volume of the frontal sinus, which was subjected to obliteration [15]. The edges of the skin wound were carefully refreshed, mobilized and brought together, ending the operation with a secondary suture.
The two-stage combined method of treatment made it possible to reduce the treatment time for patients in a hospital setting by more than 2.5 times compared to the one-stage method.
Our observations of a group of patients with CDLC over a long period of time allowed us to draw the following conclusions:
1) if this category of patients has large frontal sinuses, it is advisable to use a two-stage method of treatment;
2) the absence of relapses of the disease for about 30 years is an important criterion for the effectiveness of treatment and gives grounds to recommend the proposed methods of treatment for patients with CDLD for implementation in clinical practice.
The open method of treating patients with CDLD has set us another important task - to achieve a good cosmetic result when closing soft tissue defects in the frontal region. Cicatricial changes in soft tissues and large bone defects remaining after previous surgical treatment complicated this task. Some patients had skin defects of the frontal region of various sizes (up to 120×40 mm) and scar changes in nearby soft tissues after repeated interventions. Removing such skin defects using the widespread techniques used in facial plastic surgery was not feasible. These methods involved the mobilization of skin flaps by closing the defect [34]. Some of these methods have already been used to close skin defects in patients before admission to the clinic. Special methods of facial skin plastic surgery [35] could not be used due to pronounced scar changes in the area of skin defects.
For these patients, we have developed and performed options for plastic surgery of skin defects of the frontal region in conditions of cicatricial changes in soft tissues.
We give examples of surgical one-stage obliteration of the frontal sinuses with plastic surgery of the skin wound.
Clinical example 1
Sick R.
, 43 years old, was admitted to the clinic with a diagnosis of “chronic bilateral frontal sinusitis, osteomyelitis of the frontal bone.” There were 3 extranasal openings of the frontal sinuses in the anamnesis. On examination: a skin defect in the area of the eyebrow, deformation of the anterior wall of the right frontal sinus. Obliteration of the frontal sinuses was performed: a U-shaped graft was formed from the subcutaneous tissue of the gluteal region, approximately 25-30% larger than the volume of the frontal sinuses. The sinus cavity is washed with warm saline, and excess granulation is removed from the walls. A graft was introduced into the lumen of the frontal sinuses and laid on granulation tissue covering the walls of the sinus and the dura mater. The skin around the edges of the wound is refreshed and mobilized. In the area of the superciliary arches, two incisions were made, each 6 cm long, which is 0.7 cm larger than the skin defect subject to plastic surgery. Then, using a second arcuate incision upward, two flaps are cut out, the base of which is the lower walls of the defect. The skin-subcutaneous fat flaps are separated from the aponeurosis, mobilized, turned towards the wound and sutured in layers. The postoperative period was 12 days. He was discharged on the 14th day after the intervention (Fig. 2).
Rice.
2. Surgical obliteration of the frontal sinuses with simultaneous plastic surgery of the skin wound (first and second stages). In this observation, good results were achieved with a two-stage method of obliteration of the frontal sinuses and plastic surgery of the skin defect using nearby intact areas of soft tissue.
Clinical example 2
Patient A.,
52 years old, was admitted to the clinic with a diagnosis of “CDOLK, a condition after obliteration of the frontal sinuses, a significant soft tissue defect in the left frontal region.” He has a history of 4 surgeries on the frontal sinuses. On examination: a defect in the anterior walls of both frontal sinuses and the intersinus septum. Plastic surgery of the walls of the frontal sinuses was performed. At the first stage, the wound was inspected, surface granulations were removed, and tampons soaked in OBAC were inserted into the wound. Subsequently, tampons soaked with OBAC with chloramphenicol sodium succinate were inserted into the wound daily, according to the antibiogram. After the formation of granulation tissue on the walls of the sinus, the first stage of the intervention was to excise and moderately mobilize the edges of the soft tissue defect (Fig. 3). In the upper part of the left frontal sinus, superficial granulations were removed, the sinus was washed, and a prepared subcutaneous fat autograft taken from the patient’s left gluteal region was inserted into its lumen. The second stage involved cutting out a tongue-shaped skin-subcutaneous fat flap outward from the lateral edge of the defect in the area of unchanged skin of the left superciliary part, with its apex directed towards the middle of the forehead and its base towards the superciliary arch on the left. The skin-subcutaneous fat flap reached the postoperative scar on the patient's forehead without touching it. The flap was separated from the forehead aponeurosis to the base and well mobilized. Then, between the outer edge of the defect and the inner edge of the flap, a subcutaneous canal was formed with a scalpel and scissors so that its lower edge was at the level of the lower edge of the skin defect, and the upper edge was at the level of the upper one (see Fig. 3). After measuring the length and width of the subcutaneous canal, these data were transferred to the middle section of the flap and marked on it with dye. The flap is inserted into the subcutaneous canal with a comparison of its size and marking areas. After the necessary adjustments, the marked area of the flap is decutted (Fig. 4), and the flap itself is deployed downward and medially, inserted into the subcutaneous canal, after which its distal section is brought out into the wound formed by the soft tissue defect. After suturing the edges of the flap and the defect, mobilizing the edges of the wound by cutting out the flap, layer-by-layer sutures are applied [30]. The postoperative period proceeded without complications. He was discharged on the 10th day with a satisfactory result.
Rice. 3. Preparation for plastic surgery of a rounded, scar-modified soft tissue defect (first and second stages). A - mobilization of the wound edge; B - subcutaneous canal; B - tongue-shaped skin-subcutaneous fat flap.
Rice.
4. Plastic surgery of a scar-modified soft tissue defect of the frontal region (third and fourth stages). D — decomposed area of the flap. The advantages of this option for plastic surgery of a soft tissue defect: accessibility, ease of implementation, it does not require a lot of time and multi-stage operations, it does not cause inconvenience to the patient, and the formed skin-subcutaneous fat flap provides complete trophism of the scarred edges of the soft tissue defect, subjected to plastic. The method has been successfully used, in particular, to close gunshot defects in the soft tissues of the head.
Observation of operated patients for more than 25 years allowed us to establish that they had no relapses of the disease.
For many years, the problem of replacing bone defects in the walls of the SNP and nearby structures of the facial skeleton has been relevant. The causes of damage to these bone formations are:
1) injuries or their consequences;
2) defects after surgical interventions;
3) destruction caused by mucocele or benign tumors (osteoma, hemangiomas).
At the end of the last century, the problem of injuries became especially acute due to the emergence of military conflicts, the use of new military means, and the criminalization of peaceful life. In the structure of trauma, damage to the middle zone of the face, including the naso-orbital complex, ranges from 6 to 24% [36] and represents not only a medical, but also a social problem. A characteristic feature of injuries to the facial skeleton is the high frequency of fractures of the walls of the orbit, which occur in 20-80% of cases, among which up to 90% are fractures of the lower and internal walls of the orbit.
Treatment of these injuries is only surgical and includes revision of the fracture area, interposition of soft tissues and reposition of fragments.
For a long time, formalinized homocartilage and homobone were considered the best material for plastic surgery of the walls of the SNP and other structures of the facial skeleton, and experimental studies have shown that the most acceptable material for plastic surgery of the fronto-orbital region is bone and cartilaginous homotissue preserved in 0.5% formalin [ 37]. Such tissues are resistant to infections, quickly fuse with the edges of the bone defect and are subsequently evenly rebuilt, leading to either complete replacement of the bone defect or obliteration of the bone cavity by newly formed bone tissue. In terms of its plastic properties, homogeneous bone was not inferior to freely transplanted autologous bone and was rebuilt more evenly [37].
These materials have been replaced by more advanced ones: demineralized bone grafts (DBT), which are often called bone matrix [12]. They have such necessary qualities as flexibility combined with elasticity, plasticity, the ability to model shape and ease of mechanical processing, lack of antigenic properties, etc. All this allows them to perform operations that are practically impossible with the use of rigid grafts. It was this material that allowed us to return to the proposal of G. Portmann [38]: with extranasal access, open the frontal sinus through the anterior wall and, after removing the pathological contents from it, form an anastomosis with the nasal cavity, removing part of the group of cells of the ethmoid sinus located anterior to the frontonasal sinus channel.
One of the important properties of DCT is the ability to stimulate reparative processes in the bone with subsequent replacement of the shape, size and volume of the transplanted fragment and the possibility of osteogenesis in the wound [39]. As the newly formed bone grows, the size of the DCT decreases, as does the size of the bone defect. This property, according to some authors, allows for objective monitoring of the osteoinductive relationships of both the graft and the tissue bed in the postoperative period [40].
The founder of the research and application of VCT in our country, V.I. Savelyev [39], summarizing the data of his long-term and extensive clinical, laboratory and x-ray observations, wrote in recommendations for the practical use of grafts that the methods used for chemical sterilization of bone tissue do not violate its important biological properties, which ultimately determine the positive outcome of plastic surgery. The author believed that sterilized bone does not cause pathological changes in the recipient's body; after transplantation, it performs a mechanical role, stimulates osteogenesis and undergoes restructuring with its replacement by full-fledged bone structures. At the same time, the protein treated with formaldehyde changes its antigenic properties. The change in the immunological activity of the tissue is explained by specific reactions between protein and formaldehyde, and therefore, according to V.I. Savelyev [39], insignificant doses of formalin not only do not affect the genetic code, but also contribute to the preservation of the biological properties of preserved tissues.
Unlike non-demineralized grafts, DCTs more consistently induce osteogenesis both in the bone bed and outside it; in addition, they also have a stimulating effect, reducing the healing time of bone and soft tissue wounds. DCTs deprived of a mineral basis are more quickly vascularized in the recipient’s body and replaced by newly formed bone tissue.
Yu.V. Zotov et al. [41] noted that the inductive activity of DCTs is due to the presence of a specific inducer protein, called bone morphogenetic protein.
IN AND. Savelyev [28] proved that DCT fragments, due to their porous structure, adsorb many solutions, including antibiotics, gradually releasing them into the surrounding tissues. Saturation of VCT with antibiotics and dimexide does not affect their osteoinductive properties and allows the use of these antiseptic agents to impart antimicrobial properties to grafts [42].
Our clinic was one of the first to use this interesting material. Initially, DCT was used for myringoplasty [43]. In this case, the main evidentiary element was the study of DCT plates implanted under the periosteum of the mastoid process. A.N. Pomukhina et al. [43] proved the following using a significant amount of experimental material:
1) the use of a thin plate of DCT during surgical myringoplasty deprives it of its ability to osteoinduct and causes its replacement with loose fibrous connective tissue, which was not previously determined by other researchers;
2) DCT for total or subtotal perforations ensures a stable position of the neotympanic membrane and preservation of the anterior meato-tympanic angle.
In the ENT clinic of the Rostov State Medical University, methods and techniques for plastic surgery of the structures of the nasal cavity and SNP have been improved for more than 35 years, and fundamental research into the possibilities of VCT has been actively and successfully carried out from 1986 to the present [44].
On the use of VCT in the plastic surgery of the walls of the primary sinus, including the frontal sinuses, the clinic staff have received more than 20 patents by R.F. Our developments are aimed at closing bone defects after interventions on the maxillary and frontal sinuses using corundum ceramics [45], titanium mesh [46] and porous titanium nickelide plates [42], and, from our point of view, the use of these materials for wall plastics SNP turned out to be not effective enough.
Further studies concerned the use of DCT to close postoperative defects in the anterior wall of the maxillary sinus, including after micromaxillary sinus [42]. Successful experience with the use of this material has made it possible to use it in other cases, in particular for fractures of the upper wall of the maxillary sinus with displacement of the eyeball into its cavity.
Many authors tried to stabilize the position of fragments of the bone structures of the upper wall of the maxillary sinus by restoring its integrity in various ways, mainly by introducing into the orbital cavity any materials whose dimensions made it possible to cover the area of the post-traumatic defect. In this case, polymers (silicone, Teflon, homo- and autografts), lyophilized fascia lata, mastoid periosteum, mandibular joint tissue, autogenous bone of the walls of the maxillary sinus, preserved cadaveric costal cartilage, as well as hydroxyapatite, ultra-high molecular weight polyethylene and titanium mesh were used. including those with sprayed biositall, lactosorbide sheets, porous polytetrafluoroethylene, polydioxanone foil [47], autogenous grafts from the patient’s ilium or rib. In addition, various structures made of titanium nickelide with shape memory, as well as perforated mini-plates and mini-brackets with two or three points of fixation are used to treat fractures of the zygomatic-orbital complex [32].
VCT began to be used to treat this traumatic pathology [39, 48].
A frame structure was developed from DCT fragments, which made it possible to fix the eyeball in the orbit for a long time, maintaining its correct position [42] (Fig. 5). In addition, with the help of DCT, a supporting structure was proposed that preserves the anatomical position of the facial and, if necessary, the cerebral walls of the frontal sinuses [49].
Rice. 5. Scheme of creating a support structure for fixing the damaged upper wall of the maxillary sinus and the eyeball.
A.G. Volkov and N.A. Zakharova [49] developed and implemented a scheme for restoring the structures of the frontal sinuses after removal of osteomas, which included original surgical solutions using DCT (Fig. 6). A method was proposed for restoring the anatomical structure of the thinnest (orbital) walls of the frontal sinuses in case of their total destruction, restoring the function of the frontal sinuses and preventing cosmetic defects of the face. After removal of the osteoma, a bed of the frontonasal anastomosis was formed from the remnants of its bone structures, then a cone-shaped drainage tube made of thermoplastic mass, for example, from Portex, which does not cause degenerative-dystrophic changes in the tissues when it remains in the lumen of the formed anastomosis for a long time, was inserted into it. Then, in the lower part of the operated frontal sinus, on both sides of the drainage tube, a hemostatic sponge was installed in the form of bars, which were soaked in blood and treated with DCT, crushed in advance to the consistency of flour. A fragment of the DCT, prepared from a longitudinal section of the tubular bone, was modeled according to the shape and size of the missing orbital wall (Fig. 7) and installed with the convexity of the compact layer outward in the area of the missing orbital wall so that the upper part of the lateral surface of the DCT was located along the edge of the facial wall (approximately in the area of the edge of the brow ridge). The upper section of the DCT, which should be adjacent to the facial wall, was somewhat thinned, and holes were symmetrically placed in it and in the lower sections of the facial wall of the frontal sinus. The DCT was inserted under the periosteum and fixed to the facial wall through the applied holes using vicryl sutures.
Rice. 6. Preparation of VCT for plastic surgery.
Rice. 7. Preparing the drainage tube for surgery.
Two holes were made in the inner edge of the DCT and the lower part of the nasal bone of the corresponding side, through which a vicryl thread was inserted from the nasal cavity into the lumen of the wound in a U-shape. The threads were brought to the surface of the DCT through the holes in it and gradually tightened, bringing them closer in the lower sections to the posterior wall of the sinus, forming a rigid connection, while simultaneously fixing the drainage tube and the hemostatic sponge treated with bone meal from the DCT (Fig. 8). The periosteum was sutured, strengthening the fixation and rigidity of the DCT position. Stitches were placed on the skin.
Rice. 8. Fixation of fragments from VCT.
The advantages of this method of plastic surgery are as follows:
1) the anatomical and functional structure of the operated frontal sinus is preserved, the shape of the orbital wall becomes close in its anatomical parameters to the natural one;
2) there are no cosmetic facial defects;
3) the DCT is rigidly fixed in the place of the missing orbital wall of the frontal sinus;
4) a stationary drainage tube fixed with a graft allows for full function and removal of wound discharge in the early and late postoperative periods;
5) the use of DCT in the form of flour accelerates the processes of osteogenesis at the level of the connection of the orbital and medullary walls of the sinus.
Availability of total times