Anterior rectal resection is a surgical procedure during which the affected part of the intestine is removed. The operation is performed for a small malignant tumor localized in the rectosigmoid or upper ampullary region, 10 cm above the anus. In this case, nearby tissues are also removed: a segment of the intestine, regional lymph nodes, and vessels. In cases where the malignant tumor is located above the anal sphincteran 8 cm, total mesorectumectomy is indicated - low anterior resection of the rectum. During the operation, most of the intestine is removed up to the sphincter, and to replenish the lost reservoir capacity of the rectum, a “reservoir” is formed from the upper part of the intestine during surgery.
Both techniques are sphincter-preserving - there is no need to form a colostomy (excising part of the intestine onto the abdominal wall), although it is possible that it may be necessary to create a temporary stoma - when performing a low intestinal resection, its closure is possible in a couple of months.
With this technique, the remaining part of the rectum will be enough to form an anastomosis - connecting the ends of the intestine, thus ensuring intestinal continuity. As a result, the anal sphincter and the ability to have natural bowel movements are preserved. Moreover, thanks to the availability of modern equipment and instruments with which our clinic is equipped, the nerve fibers located in the pelvis and necessary for controlling urination and maintaining sexual function can also be preserved. At the end of the recovery period, patients quickly return to life without restrictions.
Find out the cost by phone: +7 (495) 782-50-10
Duration 2-3 hours
Time in hospital 4-10 days
Briefly about the treatment method
Bowel resection is an operation to remove part of the small or large intestine. This is a fairly traumatic procedure, so it is not performed without very compelling reasons.
Types of bowel resection
Different types of resections are performed to remove different parts of the intestine. Each type of bowel resection is named based on what it removes: Segmental small bowel resection: A portion of the small bowel is removed. The surgeon may also remove part of the mesentery (the fold of tissue that supports the small intestine) and lymph nodes in the area. This type is used to remove tumors in the lower duodenum (upper part of the small intestine), jejunum (middle part of the small intestine), or ileum (lower part of the small intestine). Right hemicolectomy: removes part of the ileum, cecum (part of the large intestine), ascending colon (part of the large intestine), hepatic flexure (flexure of the colon), first part of the transverse colon (middle of the large intestine), appendix. Transverse colectomy: the transverse colon, hepatic and splenic flexures are removed. This surgery may be used to remove a tumor in the middle of the colon when the cancer has not spread to other parts of the colon. Left hemicolectomy: Part of the transverse and descending colon, the splenic flexure (the curve in the colon near the spleen), and part or all of the sigmoid colon are removed. Sigmoid colectomy: The sigmoid colon is removed. Low anterior resection: the sigmoid colon and part of the rectum are removed. Proctocomectomy with ileoanal anastomosis: the entire rectum and part of the sigmoid colon are removed. An ileoanal anastomosis is a procedure that a surgeon does to attach the lower portion of the small intestine to the anus. Abdominoperineal resection: The rectum, anus, anal sphincter and muscles around the anus are removed. The surgeon makes one cut or incision in the abdomen and another in the perineum (the area between the anus and vulva in women or between the anus and scrotum in men). This procedure requires a permanent colostomy (taking a section of the colon out) because the anal sphincter is removed. Partial and total colectomy: Surgery to remove part or all of the colon (including the cecum).
Types of operations on the small intestine
Surgical interventions on this organ are divided into two types: emergency and planned.
The following pathologies require emergency surgery:
- Meckel's diverticulum. Protrusion of the intestinal wall. The area is excised.
- Intestinal obstruction.
- Operation Whipple. Part of the pancreas, duodenum, gallbladder and lymph nodes is removed.
- Sticking. Adhesiolysis - elimination of intestinal adhesion is carried out in two ways: - laparoscopy - dissection with a laparoscope; - laparotomy - occurs through incisions on the abdominal wall.
In elective surgery, excision is indicated for tumors on the intestine.
Indications and contraindications for the treatment method
Bowel resection is performed to treat the following diseases:
- Cancer in the small intestine, colon, rectum, or anus;
- Cancer that has spread to the intestines (treatment and symptom relief);
- Blockage in the intestines (intestinal obstruction);
- Precancerous polyps before they become cancer (called preventative surgery);
- Inflammatory bowel disease or diverticulitis;
- Ulcerative colitis (characterized by chronic inflammation of the colon and rectum, resulting in bloody diarrhea). Surgery may be indicated when drug therapy does not improve the condition.
- Mesenteric thrombosis or abdominal ischemia;
- Intestinal necrosis.
In addition, surgery is used for intestinal trauma, bleeding, and to close a hole in the intestine (intestinal perforation). The reasons for resection are always carefully assessed by the attending physician. There are a number of contraindications for the operation:
- critical condition of the patient, leading to the inappropriateness of resection,
- coma or unconsciousness of the patient,
- pathology of the heart, kidneys or respiratory system, which can lead to serious complications during or after surgery,
- inoperable tumor.
Preparation and preoperative studies
Before PDR surgery, the patient undergoes extensive preoperative examination. It includes a number of standard procedures:
- clinical and biochemical blood tests;
- general urine analysis;
- blood tests for HIV, hepatitis B and C, syphilis;
- fluorography;
- ECG.
In addition, you need to do:
- CT scan of the abdominal and thoracic cavity with contrast;
- cancer screening - MRI, CT, blood for tumor markers, ultrasound.
With the results, you need to go to a therapist and surgeon, visit an anesthesiologist, because the intervention takes place under general anesthesia.
Preparing for treatment
Before surgery, diagnostic tests are usually performed to check your general health and ensure that the surgery can be performed. This may include blood sampling, chest x-ray, electrocardiogram (ECG), angiography, CT or ultrasound, or endoscopy. You should follow a diet that excludes legumes, baked goods, alcohol, fresh fruits and vegetables. A liquid diet is administered at least the day before surgery, with nothing taken on the day of surgery. Depending on the type of bowel resection, it may be necessary to cleanse the bowel. This usually involves taking a laxative 1-2 days before surgery. Cleansing enemas may also be given in the hospital. Immediately before the procedure, antibiotics are prescribed to help prevent infection. You should also tell your doctor about all the medications, supplements, and herbal products you take.
What can you eat after kidney resection?
Nutrition is structured so as not to overload the kidneys with the work of cleansing the body of toxins and excess water (>1.5 l/day). The main rule is limiting salt. It would be better to completely avoid adding salt to food.
Prohibited:
- Spicy, smoked and fried foods.
- Carbonated drinks.
- Food with preservatives and dyes.
- Alcohol.
Coffee and spices are strictly limited. Mushrooms, radishes, garlic, and raw onions are not recommended. Store-bought sweets are replaced with homemade cakes and dried fruits.
How the treatment method works
The surgeon may use open or laparoscopic techniques. With an open technique (laparotomy), the surgeon makes a large longitudinal incision to reach the intestine. In the laparoscopic technique, small holes are made in the abdomen, and then an endoscope (a thin, tubular instrument with a light and lens) and instruments are inserted to perform the operation. The laparoscopic technique tends to result in shorter hospital stays, faster recovery times, fewer complications, and less pain during incisions. However, not all patients can undergo laparoscopic bowel resection due to the location and stage of the disease or other factors. In addition, surgeons require specialized training, skills, and equipment to use laparoscopic techniques. The surgeon examines the cavity and removes the diseased or damaged part of the intestine within healthy tissue. However, some healthy tissue on either side of the affected part may also be removed.
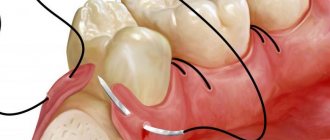
Anastasmosis
When part of the intestine is removed, the surgeon connects the remaining ends of the intestine together using stitches or staples. This procedure is called anastomosis. When the entire large intestine is removed and the anastomosis is between the small intestine and the anus, it is called an ileoanal anastomosis. When it is between the sigmoid colon and the anus, it is called a coloanal anastomosis. For any of these procedures, the surgeon may create a pocket before attaching the intestine to the anus. The pocket creates a place for stool when the rectum is removed. It helps reduce the number of bowel movements a person has and manage incontinence (the inability to control bowel movements).
In some cases, the surgeon does not connect the ends of the intestine together. Instead, it attaches one or both ends of the intestines to an opening in the abdomen. This procedure is called a colostomy or ileostomy (depending on the part of the intestine used) and is an artificial anus. A colostomy can be temporary or permanent.
Rehabilitation after surgery for vaginal cancer
After the intervention, the patient is in the clinic’s hospital under close medical supervision. She is prescribed a course of chemotherapy and/or radiation therapy. To eliminate the risk of relapse of the malignant process, a woman should regularly visit a gynecological oncologist for preventive examinations. The prognosis for vaginal cancer is determined by the stage of the disease, but such a tumor usually grows slowly and does not begin to metastasize immediately. Such an operation entails an early onset of menopause and infertility. If the patient intends to have a child in the future, a good solution would be to cryopreserve her eggs before surgery. Often, removal of the vagina leads to the appearance of psychological problems and depression in a woman, so the help of a psychologist is important here. To maintain a sexual life, you can take advantage of the possibilities of reconstructive plastic surgery and restore the vagina using a section of the intestine.
Possible complications during treatment
The side effects that may occur depend mainly on the type of bowel resection and your overall health. They include:
- obstruction (obstruction) of the intestine,
- paralyzed or inactive bowel
- damage to nearby organs such as the bladder, ureter or spleen, anastomotic leak associated with infectious problems,
- excessive bleeding wound infection,
- hernia,
- thrombophlebitis,
- inability to control urination.
The attending physician should be informed of any of the following problems after surgery: severe pain, swelling, redness, drainage or bleeding in the incision area, muscle pain, dizziness or fever, constipation, nausea or vomiting, rectal bleeding or black, tarry stools.
Restoring work capacity after kidney resection
After a maximum of 1.5–2 months, you can return to work. If the profession involved heavy physical labor or interaction with toxic substances, it is better to find another job. The lifting limit of 3 kg is sometimes extended to one and a half years; subsequently, it is not recommended to lift more than 6–7 kg.
Retirement from disability is rare and is possible in the case of an unfavorable prognosis for oncology, severe renal failure, or severe pyelonephritis.
It is possible to return to sports - fitness, athletics, swimming, skiing. Exercising with weights will cause harm.
Prognosis after treatment method
The period of time required for recovery varies depending on the initial condition, type of resection, the patient's general health prior to surgery, and the length of bowel removed. The prognosis of bowel resection depends on the severity of the disease. For example, in the case of patients with ulcerative colitis, the disease is cured and most people go on to live normal, active lives. Patients with cancer will have a less positive prognosis (due to possible relapses). Alternatives to bowel resection depend on the specific medical condition being treated.
Popular questions
Before surgery
With what weight can this operation be performed?
This operation is based not on weight, but on body mass index (BMI). Body mass index is calculated using the formula “body weight divided by height squared.” We are starting to offer longitudinal gastrectomy to patients with a body mass index of 35 and above.
Body Mass Index (BMI) Calculator
Weight, kg:
Height, cm:
BMI:
What contraindications may there be for longitudinal gastrectomy?
Peptic ulcer disease in the acute stage, mental disorders (schizophrenia) or acute - myocardial infarction and other exacerbations of the condition, for which a decision is made individually.
Is it possible to do another type of surgery at the same time as resection? (for example, remove a gallbladder, cyst, fibroid, etc.)
It is not only possible, but also necessary. If a patient has stones in the gall bladder, then we offer them the so-called “simultaneous surgery,” that is, surgery on two or more organs. This is removal of the gallbladder and longitudinal resection of the stomach. They can be different, for example, uterine fibroids.
Are there any age restrictions for this operation? Is it possible to perform a gastric resection on a child?
In the world, this operation is performed from the age of 8 years, but only for children with enormous weight, approximately 170-180 kilograms. The decision is always made individually. We have had patients in our practice for 14 years or more.
If there are problems with hormonal levels, will it be possible to have a drain?
As a rule, hormonal problems are secondary in such patients; obesity is primary. The exception is Itsenko-Cushing syndrome (adrenal insufficiency) - this is a contraindication to our operations. All other hormonal disorders (pituitary adenoma, etc.) most often disappear after surgery.
Are there any dietary restrictions before surgery?
Sometimes this operation is performed with enormous weight, in which case we prepare our patients for the operation within 2-3 months. The point of this preparation is for the patient to lose at least 10-20 kilograms in order to reduce the size of the liver. Sometimes a huge liver prevents us from performing an operation. 90% of our patients are patients with a body mass index from 35 to 50. The weight is large enough, but special preparation is not required.
What tests will need to be taken before the operation and will it be possible to take them in your clinic?
We do not send our patients to laboratories; all tests are performed in the clinic. Usually, after the day of hospitalization is determined, they come to us on an empty stomach. We conduct an examination in exactly one day and operate on the next day. This is included in the cost of hospitalization.
What additional health benefits does resection provide?
Positive effects include remission of not only weight, but also its accompanying pathology. This may be diabetes mellitus, menstrual irregularities, dysfunction of joints, especially knee and hip joints, hypertension. Curing diabetes, reducing blood pressure in hypertension, or reducing the load on joints is colossal. This sometimes saves the patient from the need for joint replacement in the future.
Are any benefits possible under compulsory medical insurance?
These operations, in principle, are not performed under compulsory medical insurance, unfortunately, so there are no benefits here.
During surgery
What is this operation?
The operation is aimed at reducing the volume of the stomach. We do it laparoscopically, through four small punctures. The essence of this operation is that we reduce the volume of the stomach many times. The volume of the stomach remains only 60-80 ml, the diameter of the stomach is no more than 14 mm. With this volume, the patient does not feel hungry. The functioning part is sufficient to consume the required amount of calories and maintain a normal, full life without any restrictions.
How long does gastrectomy surgery take?
On average about one hour.
What type of anesthesia is used during surgery?
General anesthesia. General anesthesia using modern means.
Observation program after treatment method
After your bowel resection you will need to stay in the hospital for several days. The patient should be given warm, liquid food for 1-2 days after surgery. Solid foods and meals will be introduced gradually. If a colostomy or ileostomy has been performed, a specially trained health care professional will teach the patient how to care for themselves. Temporary ostomies usually remain in place for several months. After the rest of the colon has healed, another operation, an anastomosis, will be performed. The hole in the stomach will be closed. A nasogastric tube is inserted through the nose into the stomach during surgery and may be left in place for 24 to 48 hours after surgery. This eliminates stomach secretions and prevents nausea and vomiting. It will remain until bowel activity resumes. Postoperative patient care also includes monitoring of blood pressure, pulse, respiration and temperature. Fluid intake and output are measured, and the color and amount of drainage from the wound is observed at the incision site. The patient can get out of bed approximately 8-24 hours after surgery. Most patients will stay in the hospital for 5-7 days, although laparoscopic surgery can reduce this stay to 2-3 days. Postoperative weight loss accompanies almost all bowel resections. Weight and strength are slowly restored over several months. You will need to follow a diet prescribed by your doctor. Full recovery from surgery may take two months. Laparoscopic surgery can reduce this time to one to two weeks.
Perform gastric resection
Treatment in the department of thoracoabdominal surgery and oncology of the Russian Scientific Center for Surgery is carried out according to the compulsory medical insurance, voluntary medical insurance, VMP programs, as well as on a commercial basis. Read how to get treatment in the department and have stomach surgery.
To schedule a consultation, call:
+7 (499) 248 13 91 +7 (903) 728 24 52 +7 (499) 248 15 55
Submit a request for a consultation by filling out the form on our website and attaching the necessary documents.