Caries is a common dental disease that destroys the hard tissues of teeth. According to statistics, it affects about 95-98% of the population of economically developed countries. In the treatment of caries, medicinal pads can be used. In what cases and for what they are used, we will tell you in this article.
In this article
- What is a therapeutic pad in dentistry?
- In what cases is a lining used for caries?
- Why are medicinal pads used in the treatment of deep caries?
- How is a therapeutic napkin installed for deep caries?
- Materials of therapeutic pads
- How do combined pastes work?
- Pros and cons of using medicinal pads in dentistry
In what cases is a lining used for caries?
Caries is a slowly progressive pathological process that goes through several stages. At an early stage, a carious lesion looks like a light spot on the enamel, while there is still no hole or pain in the tooth. As the disease progresses, the spot turns into a carious cavity. At the stage of superficial caries, this cavity is located within the tooth enamel; with medium and deep caries, it affects dentin tissue.
For caries in the spot stage and the superficial form of the disease, pads with a therapeutic effect are not needed; for average caries, they can be used according to indications. Most often, medicinal dental pads are used for deep caries. The peculiarity of deep caries is that the carious cavity is located as close as possible to the pulp - the neurovascular bundle, or dental nerve. At this stage, treatment is quite painful and there is a high risk of complications in the form of pulpitis and periodontitis.
Dental linings help increase the effectiveness of treatment of deep caries.
Why are medicinal pads used in the treatment of deep caries?
The purpose of a healing pad is to protect the pulp. After the dentist has removed the tissue affected by caries, cleaned and prepared the carious cavity for filling, a very thin layer of dentin, the bone tissue of the tooth, remains between it and the dental pulp. This creates a high risk of microbes entering the dental nerve and developing pulpitis. To prevent the spread of infection into the pulp, stop the inflammatory process and stimulate the production of a new layer of dentin, a special gasket is applied.
When a gasket is temporarily applied, the entire carious cavity is covered with it and a temporary filling is installed for a period of two weeks to several months. Permanent linings for deep caries are applied pointwise in the area of the tubercles of the neurovascular bundle. In the second case, along with the therapeutic one, an insulating gasket is installed.
Treatment of deep caries
The treatment method for deep caries will be determined by how deep the destruction process has spread and whether it has affected the pulp. However, the first stages of treatment are the same:
- Carrying out anesthesia - infiltration anesthesia is most often used, less often conduction anesthesia.
- Preparation of a carious cavity and removal of all pathologically changed tissues.
- Application of medicinal preparations to the bottom of the cavity. Calcium hydroxide-based preparations are usually used in the form of pads, paste, suspension or varnish. The therapeutic pad for deep caries has a powerful bactericidal effect, preventing infection of the pulp. In addition, it stimulates proliferation due to which its thickness increases. We successfully use these drugs even for the treatment of deep caries with an open pulp chamber. In this case, we apply a gasket to the area of the exposed pulp.
- Installation of insulating gasket. An insulating lining for deep caries will, firstly, fix calcium hydroxide preparations, and secondly, protect the tooth cavity from the toxic effects of the filling material.
- Installation of a seal. This may be a temporary or permanent filling, depending on the clinical situation. A temporary filling is installed in the following cases:
- During the preparation of the carious cavity, the pulp was exposed.
- A thin layer of dentin between the pulp and caries.
- The patient had pain syndrome.
A temporary filling lasts 3-4 days, and if no pathological symptoms (pain) occur during this time, it is replaced with a permanent one. If there are complications in the form of increasing pain, the filling is removed and endodontic treatment is performed. The pulp is opened, removed and the canals are filled. In the case of acute pulpitis, you can try to remove only the coronal part of the pulp, and leave the part in the canals alive.
Light-curing polymers (or, as they are also called, “photofills”) are most often used as filling materials. If the damage is extensive, but at the same time there is reason to expect stabilization of the pathological process, we recommend using ceramic inlays. If the damage is particularly extensive, the question of using an artificial crown arises.
How is a therapeutic napkin installed for deep caries?
Depending on the form and complexity of the disease, as well as the chosen method of caries treatment, the dentist can install the lining by direct or indirect application. The first option assumes that it is applied directly to the pulp area, ensuring direct contact between the gasket and the dental nerve. The method is used for tooth injuries with exposure of the nerve, for fibrous pulpitis. The second method is to apply a lining using dentinal tubules without direct contact with the pulp. It is often chosen for the treatment of deep stage caries and acute pulpitis.
Materials of therapeutic pads
Several types of dental dams are used in the treatment of deep caries:
- varnishes, solutions, light-curing cements and polymers based on calcium hydroxide;
- zinc-eugenol and combined pastes.
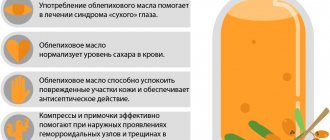
Preparations based on calcium hydroxide have a powerful bactericidal effect. The application of these compounds to the bottom of the carious cavity prevents the penetration of microbes into the dental pulp and the development of the inflammatory process. Calcium hydroxide also promotes the production of new bone tissue in the area between the cavity and the nerve of the tooth.
Aqueous suspensions based on calcium hydroxide are usually applied in a thin layer to the bottom of the carious cavity, dried and a temporary filling is placed on top. They are replaced after 30-45 days. Also, in the treatment of dental caries, chemically cured cements are often used. They are pastes containing ether and hydroxide in a 1:1 ratio. These pastes harden directly in the patient's mouth and have excellent insulating properties in relation to fillings. Light-curing polymers must be used very carefully, because there is a risk of burning the dental nerve. At the same time, they have very high strength and, in the hands of a professional dentist, can be an effective means of treating caries. Zinc-eugenol pastes are widely used as an antiseptic for temporary fillings.
Therapeutic and insulating pads
Therapeutic pads . In cases where the bottom of the carious cavity is close to the pulp, even the most gentle preparation has an adverse effect on the dental pulp. In these cases, the bottom of the cavity is covered with a medical pad before applying an insulating pad and before filling the teeth. Therapeutic pads are preparations based on calcium hydroxide. It is believed that due to the pronounced alkaline reaction of the drug, the blood circulation of the pulp is normalized and intensive deposition of replacement dentin occurs.
Recent studies have shown that not all problems with therapeutic pads have been solved. The use of medicinal dams in small cavities weakens the adhesion of the filling to the dental tissues (therapeutic dams do not have adhesion to dentin). If the medical lining remains not only on the bottom, but also on the walls of the cavity, then it can become a path for the penetration of microbes and the development of secondary caries. The material of the treatment pad may gradually dissolve and open the way for infection. Particularly problematic is the need to use therapeutic and insulating pads under composite materials. Manufacturers of bonding systems often propose to abandon spacers and replace them with modern adhesive systems. However, it is not denied that the use of calcium hydroxide-based preparations reduces the potential danger of infection under the filling. Examples of materials for therapeutic pads include the following:
Deikal
(Dycal). Durable self-curing material, “paste-catalyst” system. Contains 25% calcium hydroxide. Compatible with all filling materials.
Life
(Life). Therapeutic pad based on calcium hydroxide.
Calcipulp
(Calcipulpe). Paste based on calcium hydroxide. At the bottom of the cavity, it neutralizes acids released during the hardening of the filling material. It is used as a therapeutic lining for deep caries, and also eliminates the increased sensitivity of teeth treated for an orthopedic crown.
Insulating gaskets . It is believed that almost all permanent filling materials can have an irritating effect on the dental pulp (for example, composites due to the toxicity of the organic matrix). There is, however, evidence of the absence of chemical irritation of the pulp by widely used filling materials. Isolating gaskets are used not only to protect the pulp from the irritating effect of the permanent filling material, but also to isolate the dental pulp from toxins, reversely isolate the filling material from the influence of dental lymph, improve the adhesion of the filling (reducing the likelihood of the formation of microcracks and marginal gaps due to shrinkage of the permanent filling material ). Isolating pads are used to cover medicated pads and root fillers. As with therapeutic pads, the need to use isolating pads when adhesive systems are available is widely debated. The materials of insulating gaskets are subject to very stringent requirements: lack of chemical toxicity, mechanical strength, impermeability to acids and monomers (released components of permanent fillings), low thermal conductivity, good adhesion, coefficient of thermal expansion close to the hard tissues of the tooth. Examples of modern materials for insulating gaskets include the following.
Ionosil
(Ionoseal) – light-curing glass ionomer cement. It is resistant to acids, has good adhesion to dentin and composite materials, is tensile and resistant to compression, prevents the development of secondary caries due to the prolonged release of fluoride ions.
Fuji Line
(Fuji Lining) – light-curing glass ionomer cement. Has low shrinkage during curing.
Fuji IX
(Fuji 9, Fuji IX) – classic chemically cured glass ionomer cement.
Ionosit Baseline
(Ionosit Baseliner) is a light-curing hybrid glass ionomer cement (more often referred to as compomers). Dual-curing material (light polymerization, classic ionomer reaction). During curing, it expands slightly (by 1-2%), which compensates for the polymerization shrinkage of the composites. Physical properties are approximately 3 times stronger than traditional glass ionomer cements.
Baseline
(BaseLine) – glass ionomer cement. In addition to being used as a cushioning material, it is used for cementing crowns and temporary filling.
Time Line
(Time Line). Light-curing glass ionomer material.
Our clinics use only advanced methods of treating and diagnosing oral problems. We are waiting for you!
How do combined pastes work?
The composition of combined pastes includes oils, fillers (zinc oxide or white clay), as well as medications. The therapeutic effect of a particular pad directly depends on the latter:
- Stimulating dentin growth and promoting enamel remineralization. These drugs are called odontotropic, they are based on fluorides, collagen, calcium glycerophosphate and other substances. They are used when it is necessary to increase the layer of bone tissue between the pulp and a deep carious cavity.
- Possessing anti-edematous and anti-inflammatory effects. They help stop the inflammatory process in the dental pulp; they are based on prednisolone and hydrocortisone. Typically, such preparations are temporarily placed at the bottom of the cavity and covered with a bandage on top. If the dentin layer next to the neurovascular bundle grows too slowly, then a spacer with an odontotropic effect is applied.
- Pads with an antiseptic effect based on metronidazole or chlorhexidine disinfect and prevent the growth of bacteria.
- Proteolytic enzymes contained in the drug are needed in the treatment of acute focal pulpitis, as well as in the treatment of deep caries.
Most combined pastes harden poorly and have low strength, so they are used as a temporary therapeutic material. After their removal, a different type of therapeutic pad is usually used.
When filling cavities, various gaskets are widely used. They can be divided into 2 groups. 1. Therapeutic pads. 2. Insulating gaskets. Therapeutic pads. The purpose of the therapeutic lining is to stimulate the formation of secondary dentin, protect the pulp from external influences and create conditions for stopping the reversible inflammatory process in it. Therapeutic pads are used to stimulate the formation of secondary dentin:
When filling cavities, various gaskets are widely used. They can be divided into 2 groups. 1. Therapeutic pads. 2. Insulating gaskets.
Therapeutic pads. The purpose of the therapeutic lining is to stimulate the formation of secondary dentin, protect the pulp from external influences and create conditions for stopping the reversible inflammatory process in it.
Therapeutic pads are used to stimulate the formation of secondary dentin: • in the presence of a deep cavity; • in case of tooth trauma, when the crown fracture line passes close to the pulp.
If it is impossible to remove all damaged dentin without the risk of opening the pulp, then stimulate the formation of secondary dentin using a pad with calcium hydroxide. A prerequisite is the absence of symptoms of pulpitis at the time of treatment and in the medical history, as well as close to normal electroodontodiagnosis (EDD) numbers.
Stages of applying a therapeutic pad. 1. Anesthesia is performed, after which the defect is prepared, removing the maximum possible amount of necrotic tissue without the risk of opening the pulp. 3. Apply a medical pad. 4. A temporary filling made of glass ionomer cement is applied for a period of 10 weeks. A dressing made of water-based or oil-based dentin does not provide long-term insulation and protection from irritants. 5. After 10 weeks, the viability of the pulp is checked according to EDI data, reactions to a temperature stimulus are studied, and, if necessary, an X-ray is taken. 6. Under anesthesia, the temporary filling, medical lining and layer of affected dentin are removed under the control of a caries detector and probing. 7. If necessary, a therapeutic pad is applied pointwise to the area of projection of the pulp horn and a permanent filling is applied.
Dental restoration after injury, especially in adolescents, is accompanied by mandatory etching of tooth tissue. In this case, the acid does not act on the sclerotically changed one (as in the case of working with a carious cavity), but on a thin layer of intact dentin with wide dentinal tubules. In such cases, it is necessary to use therapeutic pads that stimulate the activity of odontoblasts, and insulating pads that cover the thinnest layer of dentin.
In case of a deep cavity or in case of accidental opening of the tooth pulp without symptoms of pulpitis, a medical lining is applied, since in case of a deep carious cavity, even the most gentle preparation can lead to injury to the processes of odontoblasts. We cannot exclude the direct influence of waste products of microorganisms and a decrease in pH in the peripulpal dentin. To provide an anti-inflammatory effect on the pulp and stimulate the function of odontoblasts to enhance mineralization and deposition of replacement dentin, preparations with calcium hydroxide are used: “Dycal” (“Dentsply”), “Alkalainer” (“Espe-3M”), “Laif” (“ Kerr"), etc.
Insulating gaskets. The purpose of the insulating spacer is to protect dentin from possible exposure to the etching gel or composite; connection of dentin to the composite in the absence of a primer. Isolating linings are applied to the enamel-dentin border. Currently, insulating gaskets are not used as widely as before, thanks to the creation of new adhesive systems.
Insulating spacers are necessary when working with those materials that do not include a dentin sealant primer. To reliably seal dentinal tubules, glass ionomer cements should be used as spacers, which have the ability to form a strong bond with dentin, cement and composite. According to the curing mechanism, spacer glass ionomers are divided into light-curing and self-hardening.
Pros and cons of using medicinal pads in dentistry
The use of medicinal pads in dental practice has a number of advantages:
- They relieve inflammation, promote tissue regeneration, and help prepare the tooth for filling.
- Many drugs contain anesthetics that provide an analgesic effect, which is important when treating tissues near the sensitive dental nerve.
- Most materials are highly plastic, harden quickly and prevent the formation of microscopic cracks in the tooth.
In addition to the advantages, therapeutic pads have a number of disadvantages:
- They impair the adhesion of the filling to the walls and bottom of the cavity, which can shorten the service life of the restored tooth.
- If the technology for installing a medical pad is violated, the risk of tissue infection increases.
- Most materials dissolve when exposed to liquids, so they must be replaced frequently.
Despite the disadvantages, medicinal pads are still widely used in dentistry, as they have a wide spectrum of action and help solve many therapeutic problems.