Why do papillomas occur in children?
Once inside the body, the virus peacefully coexists with other microorganisms and does not manifest itself in any way until a certain point - when the child’s immunity weakens, benign growths may appear. The reasons for the appearance of papillomas in children are due to a decrease in natural protection in the case of:
- previous bacterial, viral and fungal infections;
- frequent colds;
- allergies;
- autoimmune pathologies;
- gastrointestinal diseases;
- immunodeficiency;
- long-term drug therapy;
- injuries, surgeries and burns;
- vitamin deficiency
Any attack on children's immunity can provoke virus activity. Sometimes the starting point is mental and physical overexertion, stress, and nervous shock.
HPV is highly contagious and can be transmitted even through short-term contact with a carrier. In children, 3 routes of infection with the human papillomavirus are most relevant.
- Perinatal. Passing through the vaginal canal during childbirth, the baby comes into contact with the physiological secretions of the mother, receiving a viral load. Another option for this method of infection is the transmission of HPV from the expectant mother to the fetus through the placental bloodstream during pregnancy.
- Domestic. This method is the most common reason for the appearance of papillomas on a child’s body. The virus is transmitted through surfaces and objects touched by an infected person. Common sources are towels, combs, general hygiene products, and clothing, from which HPV enters the child’s body through abrasions and small wounds.
- Contact. Transmission of the virus occurs when a healthy person comes into contact with the skin, hair or other parts of the carrier’s body. The simplest example of such an infection is playing and interacting with children who have rashes.
The incubation period lasts from 2–4 weeks to 3–6 months, less often up to 2–4 years. The optimal conditions for the development of HPV are a humid and warm environment. In the fresh air without contact with human skin, the virus quickly dies.
How are papillomas treated?
Complex therapy for HPV includes removal of existing tumors by surgical methods, destruction of the causative agent of the disease and increasing the body's protective abilities.
Surgical methods
Popular methods of surgical treatment of papillomas include:
- Electrocoagulation (electrodestruction). It is considered one of the “delicate” methods for removing pedunculated polyps. The growth tissue is excised with an electric knife, and the damaged vessels are “sealed” due to the thermal effects of the current. Wounds after electrocoagulation heal quickly without forming rough scars. This method is often used in cases where special care is needed - if papillomas are located on the face, eyelids, and in the corners of the eyes.
- Cryodestruction. The procedure for destroying selective areas of tissue with cold is minimally invasive, eliminates the risk of infection, and does not require anesthesia. Cryodestruction is carried out by applying liquid nitrogen to the affected area. The formation of ice crystals in papilloma cells causes irreversible damage.
- Laser removal . The technique is based on ablation (evaporation) of tissue with a light pulse. This is an effective and safe method for removing skin tumors, allowing you to work in the most delicate areas - on the face, lips, tongue, eyelids. Coagulation of small vessels, which occurs during the “burning” process, prevents the development of bleeding. The procedure is performed under local anesthesia.
- Radio wave surgery is a non-contact method of destroying tumors using high-frequency radio waves. The procedure is performed using the Surgitron device. It is bloodless and painless, does not leave scars and eliminates relapses, since radio waves have a sterilizing effect.
Important! Do not try to cut or pick out the growth yourself - such actions can lead to suppuration or malignant degeneration of the tumor, and the virus becomes more active when the papilloma is damaged.
Therapy methods
Therapy for papillomavirus is aimed at inhibiting HPV activity and increasing immunity. The most frequently used antiviral and immunomodulatory drugs in medical practice are Acyclovir, Isoprinosine, Viferon, Condimin, Panavir, Aldora and Bonafton ointments. They cause the death of a significant part of the virus, and reduce the risk of re-growth of papillomas after their removal.
Consultations with a doctor online Taking care of your health is a life priority for everyone.
Communicate with doctors online and receive qualified assistance without leaving your home. Try it Please note! The information on this page is provided for informational purposes only. To prescribe treatment, you must consult a doctor.
HPV symptoms
The papilloma virus infects the skin and mucous membranes, causing the proliferation of the epidermis and the appearance of pathological neoplasms:
- papillomas;
- warts;
- condylomas.
They look like small skin growths ranging in size from 1 to 5–8 mm, sometimes there are growths reaching 1–2 cm. Basically, such formations imitate healthy skin in color, but there are elements of dark brown and white shades.
The main places of distribution of papillomas:
- face and neck;
- external genitalia and groin area;
- the inner surface of the elbow and knee bends;
- soles of feet;
- fingers and skin around nails.
On the mucous membranes, elements can appear in the larynx, nasal passages; in girls, sometimes there are formations localized on the cervix.
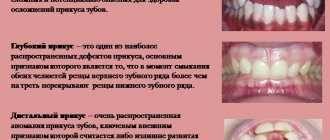
Types of formations
There are several types of papillomas.
- Vulgar (common) warts. They are the most common type of neoplasm. They have a “leg”, rise noticeably above the surface of healthy skin, reaching a diameter of up to 1–2 cm. Sometimes hair grows from the central part of the wart. Such formations do not bother the child with pain or itching and appear on the arms, back or legs.
- Flat or juvenile papillomas. They look like small pigmented plaques of a fuzzy round shape, do not extend beyond the skin and form in groups. Such elements are characterized by a smooth surface and selectivity: they appear on the face, neck, legs, sometimes hands, but never in the armpits, genitals or skin folds. Occurs in children older than 5–6 years.
- Condylomas or genital papillomas. These elements resemble small papillae. They are pink in color and form in areas with thin skin: in the genital area, on the mucous membranes.
- Plantar warts. They affect the feet, occur under the big toes and visually resemble small round calluses.
Another variant of formations is filamentous warts or acrochords. They are similar to regular ones, but differ in elasticity and more compact sizes up to 5–6 mm. They prefer to appear under the mammary glands, in the groin, armpits, and are found on the neck and face.
The dangers of human papillomavirus
Some of the representatives of these microorganisms are harmless to humans, while others can provoke the growth of cancer cells. HPV is classified into two main types:
- Strains with high oncogenic risk. Such variants of the virus provoke the development of condylomas on the mucous membranes and in the genital area. Under unfavorable circumstances, they can cause an oncogenic mutation.
- Strains with low oncogenic risk. Viruses of this type cause warts, plantar lesions and juvenile papillomas. The risk of cell degeneration is minimal.
The greatest danger lies in girls: studies conducted in the USA have proven that 98% of cases of cervical cancer are associated with this virus. There is also a risk of developing cancer of the vagina, ovaries, anal canal, larynx, pharynx, and in boys, the genitals. Papillomas located in the anus and genital area require special attention.
Types of benign tumors of the tongue
Papilloma
Focal skin growth caused by activation of the human papillomavirus in the body. The virus is transmitted when the tongue comes into contact with the mucous membrane or skin of an infected person. In the rarest cases, transmission of the virus occurs through household contact. The virus can remain dormant for a long time and appear when the immune system is weakened.
Externally, papillomas look like small pink, flesh-colored or white papillae of various shapes. Their size usually does not exceed two centimeters. You can detect these tumors yourself. They are usually localized on the back, surface and tip of the tongue. These small tumors pose a serious threat to human health because they are very often damaged and susceptible to malignancy.
Adenoma
The occurrence of this tumor is caused by the proliferation of glandular epithelium. As a rule, neoplasms are single. The following types of tongue adenoma are distinguished:
- polymorphic;
- basal cell;
- canalicular;
- sebaceous;
- adenolymphomas;
- monoform.
The pathology is usually accompanied by the formation of polyps on the tip of the tongue.
Botriomyxoma
A benign tumor of the tongue, the occurrence of which is caused by traumatic injuries - burns, cuts, injections. A couple of months after the injury, a red tumor-like formation with a lobulated or smooth surface may appear in its place. Botriomyxoma has a dense elastic consistency, sits on a stalk, and with minor damage begins to bleed.
Fibroma
A neoplasm that is formed from connective tissues covered with mucous membrane. Usually appears as small nodules, but can also look like branched polyps. The main causes of the disease are traumatic and inflammatory processes in the oral cavity. Most often, a tumor forms against the background of advanced inflammatory dental diseases - stomatitis, glossitis, periodontitis, gingivitis.
Retention cyst
The tumor occurs due to problems with the outflow of secretion from the gland, which causes blockage of the duct. Because of this, the secretion gradually accumulates in the gland, stretches it and fills it with new contents. This type of tumor is removed surgically.
Lipoma
A tumor that is predominantly localized in the back of the tongue. A lipoma forms in the submucosal layer of the tongue and has a soft and elastic consistency. Often the process of lipoma formation occurs without symptoms, so diagnosing it at an early stage is extremely difficult.
Myoma
A tumor in the tongue that occurs due to the growth of muscle tissue. Myoma has a fairly dense consistency, is covered with a mucous membrane, and small papillary outgrowths can form on it. This tumor usually reaches a centimeter in size.
Neurofibroma
A tumor develops from the sheaths of peripheral nerves. Doctors associate its formation with a defect of the facial or trigeminal nerve. This tumor is extremely rare.
Hemangioma
This is a vascular neoplasm that occurs in the tissues of blood vessels. The tumor is benign - it grows quite slowly and does not penetrate other organs. However, hemangioma is completely unpredictable, as it can suddenly increase in size and begin to interfere with the functioning of the tongue. Depending on the structure of the tumor, it can be of two types: simple (looks like a tangle of capillaries located on the mucous membrane of the tongue) and cavernous (a tangle of large vessels under the mucous membrane of the tongue).
Lymphangioma
The tumor usually grows in the walls of the lymphatic vessels, which then leads to a significant increase in the size of the tongue. Tumors often form on the tip of the tongue and its surface.
Struma of the tongue
A congenital pathology that occurs due to a violation of the location of fragments of the thyroid gland. It looks like a small organic node. After surgical removal of the tumor, the prognosis for the patient is favorable.
Diagnosis of HPV
The main clinical sign of papillomatous infection is formation on the skin. Therefore, in most cases, an examination by a doctor is sufficient to make a correct diagnosis. Additional examination methods are:
- biopsy or scraping - taking biological material for further research;
- PCR (polymerase chain reaction);
- General and biochemical blood test.
These laboratory diagnostic methods help:
- detect the presence of papilloma virus in the child’s body (if there are no growths on the skin);
- accurately determine the HPV strain;
- understand the form of the infection (acute or chronic).
These data are necessary for assessing oncogenic risk and timely further examination.
Treatment of HPV in children
Unfortunately, there are no effective medications for the treatment of papillomavirus in children, as well as in adults.
In most cases, the body copes on its own, and action is only necessary in situations where there is a risk of oncological processes or tumors interfere with the child’s daily life. What do they do if children develop papillomas?
- Do not panic. In the vast majority of cases, warts and other growths go away on their own within 2–3 years. The human papillomavirus is not only easily transmitted, but also quickly “leaves” the child’s body without any consequences or external help.
- Do not try to remove the growths at home, do not tear off or cut off under any circumstances. This is fraught with infection and the extensive appearance of new rashes.
- Contact a dermatologist if any suspicious elements appear on your child’s skin. During the consultation, the doctor will examine and give recommendations, and, if necessary, prescribe removal.
Medical care for manifestations of HPV is limited to the removal of formations that affect the quality of life or are located in places where they are often injured and cause discomfort (on the eyelid, in the genital area, in the larynx).
An extraordinary inspection is needed if:
- the color of the papilloma changes;
- the wart begins to grow or change shape;
- blood or other fluid is released from the formation;
- papilloma is subject to constant friction due to clothing;
- the rashes are on the face or mucous membranes.
It is advisable not to delay a visit to a dermatologist if the formation itches, hurts, causes other physical discomfort, or has been injured. In other cases, it is recommended to observe the “behavior” of the papilloma virus and control the elements on the child’s body.
Options for removing papillomas
There are 5 modern and proven methods, each of which has its own limitations, features and advantages.
- Electrocoagulation. The method is based on the influence of high-frequency electric current. It literally “burns out” the neoplasm, leaving in its place only a dry crust, which eventually falls off on its own.
- Radio wave surgery. This method allows you to remove warts and other elements without contact with the skin, which eliminates the risk of thermal damage to tissue.
- Laser therapy. It involves treating the affected area with light waves of a certain length.
- Cryodestruction. It involves “freezing” new growths with liquid nitrogen.
- Surgical excision. It is performed under local anesthesia using a scalpel.
It is strictly not recommended in childhood to resort to traditional methods of removing warts and to use medications from the pharmacy on your own without the supervision of a doctor. After removal of papillomas, children should not:
- tear off the crust;
- sunbathe;
- visit the baths;
- cover the treatment area with a plaster;
- scratch and rub the removal site.
You should not use creams and ointments without a dermatologist's prescription. In the first 1–4 days, it is advisable to refrain from walking in direct sunlight, swimming in public bodies of water and activities that can injure the treated area of skin.
Which doctors treat
As a rule, HPV treatment is a long process. It takes up to six months to completely get rid of the infection. Depending on the type of virus and the location of the tumors, in addition to a dermatologist, treatment may require the participation of several specialists.
- Surgeon. Deals with the removal of papillomas located on the torso, arms, legs or face.
- Urologist. Men with growths on the genitals should contact this specialist. If it turns out that HPV has oncogenic characteristics, a consultation with a urological oncologist will be required.
- Gynecologist. He is contacted if growths of epithelial tissue are found on the external female genitalia or the cervix.
- Proctologist. She treats papillomas localized in the anus and perineum.
- Otolaryngologist, dentist, ophthalmologist. They are directly involved in the treatment of HPV if the tumors are located in the mouth, on the tongue or on the eyelids.
- Immunologist. This doctor is referred to if large areas of the skin are affected by the virus, which means that the immune system is clearly unable to cope with the infection.
HPV prevention
The most effective method of preventing infections and complications caused by the human papillomavirus is vaccination. It is carried out before the onset of full puberty and before the start of sexual relations. The optimal age is from 9 to 11 years.
Other preventive measures are:
- maintaining a healthy lifestyle;
- balanced healthy diet;
- timely treatment of abrasions, scratches and other skin damage;
- informing children and adolescents about the dangers of smoking, since tobacco use increases the risk of oncogenic mutations of the virus;
- regular preventive examinations.
It is very important to monitor the child’s health and support immunity in accessible ways. Active physical activity, hardening, and outdoor games are encouraged, allowing the formation of an adequate immune response to environmental factors. It is advisable to abandon home self-medication and uncontrolled use of medications, since incorrect actions can reduce the natural defenses of the child’s body and lead to the activation of HPV.