Symptoms of advanced oral cancer
You may have any of the following symptoms:
- persistent pain in the lips, mouth, or both;
- a lump on the lips, neck, or mouth that does not go away;
- white or red spots on the gums, tongue, or cheeks;
- persistent bleeding, pain, or numbness in the mouth;
- persistent sore throat;
- feeling as if something is stuck in the throat;
- problems chewing or swallowing;
- pain while chewing food or swallowing;
- swelling, which causes dentures to fit poorly or cause discomfort;
- voice change;
- ear pain;
- inability to open mouth.
to come back to the beginning
Complications
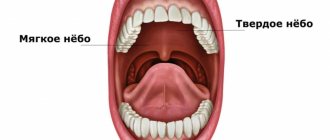
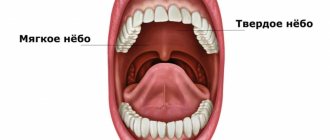
Complications of surgical resection of the soft palate may include:
- velopharyngeal insufficiency (most often);
- hypernasal speech;
- dysphagia (impaired swallowing);
- effusion in the middle ear due to scarring at the opening of the eustachian tube.
The extent and likelihood of these complications depend on the extent of the resection, the size of the defect, and the method of reconstruction. The larger the resection and defect, the greater the likelihood of these complications occurring.
With soft tissue resection preserving only the bony palate and soft palate, the resulting defect heals with granulation and epithelialization, and no complications are expected. If patients have previously had radiation therapy in this area, healing may be delayed.
Palate cancer and its treatment can sometimes cause problems such as loss or changes in taste, dry mouth, or even tooth loss. This can make it difficult to eat, leading to weight loss and weakness due to poor nutrition.
Radiation therapy may also cause long-term or permanent side effects.
- Damage to the salivary glands. It may cause dry mouth. This leads to problems with eating and swallowing. Lack of saliva can also lead to tooth decay (cavities).
- Damage to the jaw bone. This problem, known as osteoradionecrosis of the jaw, can be a serious side effect of radiation therapy. This condition is difficult to treat. Osteoradionecrosis is manifested by pain in the jaw, and sometimes by fractures, which require surgical treatment.
Newer radiation treatments such as IMRT may help reduce this side effect. The drug amifostine (Ethyol®) may also help reduce this side effect by limiting radiation damage to normal tissue. It is injected into a vein over 15 minutes before each radiation treatment.
Diagnosis of advanced oral cancer
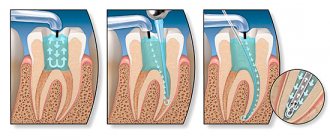
To check if you have oral cancer, you will need to have a biopsy (a procedure that takes small samples of tissue). During a biopsy, your healthcare provider will remove a small piece of tissue from the area where the cancer may be located. This tissue is examined for the presence of abnormal or cancerous cells. It will take at least 5 business days to receive biopsy results. The healthcare professional will then explain the diagnosis to you.
Your healthcare provider may also order other tests, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), to help you Find out if the cancer has spread to other areas.
to come back to the beginning
Causes
Oral cancer
The mechanism of development of oral cancer is generally similar to the stages of formation of any malignant tumor. Healthy epithelial cells, after dividing, perform their functions and are gradually destroyed.
Cell division is regulated by genetic information and special intracellular mechanisms. Under certain conditions, the division process can be disrupted, resulting in the formation of an abnormal cell mass called a malignant tumor.
Information about surgery to treat advanced oral cancer
Surgery is the most common treatment for advanced oral cancer. Its goal is to remove all cancerous tissue. Depending on the surgery, you may need tissue, muscle, or bone reconstruction. In this case, a plastic surgeon will work with a surgeon who specializes in the head and neck.
A surgeon who specializes in the head and neck may refer you to an oral and maxillofacial surgeon. If necessary, they will examine your teeth and make a denture. A prosthesis is a device that replaces a removed body part.
The extent of the operation depends on how the head and neck surgeon removes the cancerous tumor.
- Some tumors are removed through an incision (surgical cut) in the jaw. An incision is made between the 2 lower front teeth. Once the incision is made and the tumor is removed, the jaw is reattached using a metal plate and screws.
- If the cancer is close to the jaw or only affects a small part of it, only that part of the bone is removed.
- If the cancer affects a large part of the bone, that part of the jaw is removed completely.
- Sometimes tissue, muscle, bone, arteries and veins may be taken from another part of the body to replace those that were removed. This is called a free flap.
- You may also need to have lymph nodes in your neck removed. The tumor and lymph nodes will be sent to the Pathology Department for examination. It will take at least 1 week to see results.
to come back to the beginning
Diagnostics
The basis for diagnosing RPR is biopsy. A small piece of tissue is separated from the tumor and further examined under a microscope. Biopsy is an accurate and reliable diagnostic method. But sometimes additional studies may be required to determine the extent of the malignant tumor.
Your doctor may order one or more of the following tests:
- CT scan to detect tumors in the throat, neck, lungs;
- PET scan to determine if there are metastases to lymph nodes or other organs
- MRI to get detailed images of the head and neck and determine the stage of cancer;
- endoscopy to examine the nasal passages, sinuses, larynx and trachea.
Tracheostomy
Sometimes surgery to treat advanced oral cancer can cause swelling in the throat. In this case, your surgeon may perform a tracheostomy to make sure you can breathe normally. A tracheostomy is an operation to create a surgical opening in the windpipe to make breathing easier and protect your airway. Before your surgery, your healthcare provider will discuss with you whether you will need a tracheostomy.
During a tracheostomy, your surgeon will make a hole in your neck and insert a tracheostomy tube into your trachea (windpipe). This will allow you to breathe easier. If you are having a tracheostomy, your nurse will give you the resource Care after a tracheostomy.
You will also have a tracheostomy if your surgery involves certain types of reconstruction or free flaps.
A nurse will care for your tracheostomy while you are in the hospital. Any mucus that forms will be removed using a suction tube. Keeping your airways clear will make breathing easier and reduce the risk of pneumonia.
The tracheostomy tube will be removed when the swelling in your airway has subsided and you can breathe normally. If you still have a tracheostomy after discharge, your nurse will teach you how to care for it.
to come back to the beginning
After operation
Communication after tracheostomy
If you have had a tracheostomy, you may not be able to speak when you first wake up after surgery, but you will be able to communicate in writing. The nurse will give you a pencil and paper. You can also answer yes or no questions by nodding or shaking your head. You may also be given a tablet to facilitate communication. The tablet comes with an app to help you communicate your needs. Your nurse will teach you how to use the tablet.
Compression boots
You will be wearing compression boots while you are in bed. These boots put gentle pressure on your calves, which prevents blood clots. They will be removed when you are able to get out of bed and walk. If you have surgery without a free flap, you will be able to get out of bed and walk the day after surgery. If a free flap was used during surgery, this will occur somewhat later, depending on the location of the free flap. Every day your physical activity will increase.
Nutritional tube
If you find it too difficult to eat and drink, you may have a feeding tube placed after surgery. Depending on the surgery, you may be unable to eat for a week after surgery. Your healthcare provider will provide you with more information.
Anesthesia
You will experience pain after surgery. Be sure to ask your nurse for painkillers. You may initially receive it through an intravenous (IV) drip. Later, you may take medications by mouth (by mouth) or through a feeding tube if you have one. As you heal, you will need less pain medication.
Drainage tubes
If lymph nodes in the neck are removed, drainage tubes will be placed in the neck. You may also have them installed in the area of the free flap, if one was used. Drainage tubes are usually removed when the amount of discharge decreases. Most likely, all of these tubes will be removed before you are discharged from the hospital. If you are discharged from the hospital with tubes in place, your nurse will teach you how to care for them. For more information, read the pre-surgery guide About Neck Dissection Surgery.
Oral hygiene
Your nurse will teach you how to use the oral irrigation and care kit. This kit will help keep your mouth clean and speed up healing. After you leave the hospital, you will need to rinse your mouth with an irrigation kit. It is especially important to rinse your mouth after eating. After you eat, there should be no food particles left in your mouth. For more information, see Oral Irrigation
How to prevent spasms of the masticatory muscles
Spasm of the masticatory muscles is the inability to open the mouth. During recovery after surgery, it is very important to prevent spasm of the masticatory muscles. Your nurse will teach you exercises to help prevent this side effect, which are described in How to Prevent Masseter Muscle Spasms.
to come back to the beginning
Stages of the disease
Stage I is characterized by the presence of a tumor up to 1-2 cm in diameter, not extending beyond the affected area (cheek, gums, palate, floor of the mouth), limited to the mucous membrane. Metastases are not detected in regional lymph nodes.
Stage II - a lesion of the same or larger diameter, which does not extend beyond any one part of the oral cavity, but extends into the submucosal layer. There are single metastases in regional lymph nodes.
Stage III - the tumor grows into the underlying tissues, but not deeper than the periosteum of the jaw, or has spread to adjacent parts of the oral cavity. In regional lymph nodes there are multiple metastases measuring up to 2 cm in diameter.
Stage IV - the lesion spreads to several parts of the oral cavity and deeply infiltrates the underlying tissues, in the regional lymph nodes there are immobile or disintegrating metastases, and the presence of distant metastases is also characteristic.
Classification by stages is periodically subject to revision; you can find a division of stages into subtypes - A and B. Currently, classification by stages is used less and less, the TNM classification is more relevant. Its principle is that this coding indicates the characteristics of the tumor itself, the condition of the closest (regional) lymph nodes, and the presence or absence of distant metastases.
In the diagnosis, the oncologist indicates the histological type of cancer, since different types of cells differ in growth rates, tendency to metastasize, and sensitivity to treatment. All types of classifications serve one purpose - to correctly assess the extent of the spread of the disease, the degree of damage and develop the right tactics of assistance.
Book a consultation 24 hours a day
+7+7+78
Discharge after surgery
Your surgeon will tell you when you can return to work and normal activities. It depends on the surgery you underwent and the speed of recovery.
In most cases, patients can cope with daily activities at home without additional help, but the nurse will discuss this with you before leaving the hospital. If you need help, your nurse or case manager can help arrange visits from a visiting nurse or home health professional.
Call your healthcare provider if you have any of these signs or symptoms of infection:
- temperature 101°F (38.3°C) or higher;
- increased redness around the incisions;
- increased discharge from the incisions;
- discharge that has an unpleasant odor;
- increased pain that does not go away after taking a prescribed pain reliever or acetaminophen (Tylenol®).
to come back to the beginning
Follow-up
You will need to see your head and neck surgeon 7-10 days after discharge. If a plastic surgeon was involved in the operation, you will also need to see this specialist. Call each doctor's office to make an appointment. Depending on the rate of healing, you may have some stitches removed at your first follow-up appointment. You will also have a complete examination of your head and neck.
If your lab results are ready, your head and neck surgeon will review the results with you during your first follow-up appointment. He will also give you details about the cancerous tumor that was removed during surgery.
Your healthcare provider will discuss the need for additional treatment with you. In most cases, patients with advanced oral cancer need to undergo radiation therapy, chemotherapy, or both after surgery to ensure that all cancer cells are removed. If you would like to have these procedures done at Memorial Sloan Kettering (MSK), an appointment will be made for you. If you would like to take them elsewhere, we can help you choose a healthcare professional. Your medical record will be sent to the health care provider who will treat you.
It is very important not to miss any follow-up appointments. These techniques can help detect relapse (recurrence of cancer) or new cancers at an early stage. As time goes on, visits will be scheduled less frequently.
to come back to the beginning
Risk factors
Among the main factors predisposing to the development of palate cancer are the following:
- bad habits: smoking, especially in combination with drinking strong alcohol, chewing various mixtures (for example, betel);
- precancerous conditions that can develop into a malignant tumor,
- chronic inflammation of the oral mucosa;
- factors of chronic mechanical trauma to the oral mucosa (destroyed teeth and their roots, poorly manufactured dentures);
- work in hazardous industries (contact with carcinogens, work in high temperatures);
- lack of vitamin A;
- eating too hot and too spicy food.
Separately, I would like to dwell on diseases that are obligate, that is, with a high frequency of malignancy, and facultative, with a low frequency of malignancy, precancerous conditions.
An obligate condition for palate cancer is Bowen's disease - single or multiple neoplasms of the mucosa, localized in its surface layer. In the early stages of its development, the neoplasm looks like a reddish spot with jagged edges. The spots grow slowly, and when several spots are located close to each other, they can merge. With further growth, the spots may peel off, and depressions or growths may appear on them.
Throughout its progression, Bowen's disease does not manifest itself as pain or itching. The degeneration of Bowen's disease into cancer is indicated by the appearance of ulcers on the plaque.
Bowen's disease is often considered a cancer in situ and requires immediate surgical treatment when diagnosed.
Optional precancerous diseases include:
- Leukoplakia - flat, whitish areas of the mucous membrane, smooth to the touch and with a soft consistency. Flat leukoplakias may remain unchanged for many months, without thickening or ulcerating. The incidence of cancer due to leukoplakia varies according to different authors and ranges from 15-75%.
- Erythroplakia is a red area of the mucous membrane raised above the surface, which is easily injured and bleeds. In 70% of cases it leads to the development of cancer (and according to a number of authors, with long-term existence of erythroplakia, this probability increases to 80-100%).
- Leukokeratosis is the proliferation of squamous epithelium. Upon examination, it looks like whitish spots of various shapes, slightly rising above the mucous membrane of the soft palate. When palpating the area of leukokeratosis, a dense consistency and rough surface are determined.
- Papillomatosis is a papillary growth of connective tissue caused by infection with the human papillomavirus. In most cases, papillomas develop against the background of progression of leukokeratosis.
Due to the risk of malignancy of the above formations, surgical treatment is necessary - either conventional excision of the affected areas of the mucosa, or cryodestruction or electrocoagulation can be performed.
Recovery
Being diagnosed and treated for cancer can leave you feeling stressed and overwhelmed. Each person deals with this differently. Many people say that it is helpful to focus on small improvements that you will see with each new day and each new week, for example:
- swelling will gradually subside;
- the face will begin to look more natural, and the scars will become less noticeable;
- It will become easier for you to speak and you will be able to eat many of your favorite foods; A dietitian can help you choose the best way to prepare your favorite foods until your ability to chew and swallow is restored;
- you'll have more energy to do the things you love.
Support Resources
Numerous resources are available to help you and your loved ones through the recovery process. Some of them are offered by MSK, while others can be found locally. Ask your health care provider or social worker about available resources.
You may find it helpful to talk to a head and neck cancer survivor or someone who has cared for someone who has undergone similar treatment. Through our Patient and Caregiver Support Program, you can connect with former patients and caregivers. To learn more about this program, call 212-639-5007.
MSK's Resources for Life After Cancer (RLAC) Program provides support and education for patients who have completed treatment. For more information about this group and the programs offered, call 646-888-8106 or visit our Cancer Survivor Program page at
Emotional Health
It is normal if you feel depressed during or after treatment. Programs are available to help you cope with these feelings. It is important to recognize the signs of depression, such as:
- feelings of helplessness and sadness;
- inability to concentrate or do usual activities;
- mood swings;
- changes in sleep patterns (increasing or decreasing usual sleep duration);
- increase or loss of appetite.
Call your healthcare provider if you have these symptoms and they do not go away for more than 2 weeks. To speak with a counselor, call the MSK Counseling Center at 646-888-0200. For more information, see Coping with Depression During Cancer Treatment.
Smoking and drinking alcohol
Using tobacco or alcohol increases your risk of developing oral cancer. Quitting these bad habits will help reduce the risk of recurrence or formation of a new tumor. If you want to quit smoking, we can refer you to a Tobacco Treatment Program at our center or in your community. For more information, contact MSK's Tobacco Treatment Program at 212-610-0507 or visit: . Tips on how to quit smoking are given in our material Recommendations for the treatment of tobacco addiction for patients and their family members.
If you want to stop drinking alcohol, there are programs that can help you.
For more information, call MSK's Counseling Center at 646-888-0200. to come back to the beginning
Radiation therapy: how is treatment carried out?
Choosing a treatment regimen using radiation therapy
Typically the course of treatment lasts 4-7 weeks. In some cases, when radiation therapy is carried out before surgery to reduce the size of the tumor or to alleviate the patient's condition, the course duration is 2-3 weeks.
Typically, radiation therapy sessions are carried out 5 times a week. Sometimes, in order to protect normal tissues in the irradiation zone, the daily dose is divided into 2-3 sessions. A two-day break at the end of the week allows healthy tissue to recover.
The decision on the total radiation dose and the number of sessions is made by the radiologist based on the size of the tumor and the location of the tumor, its type, your general condition and other types of treatment being performed.
How does a treatment session work?
You will be asked to lie on a treatment table or sit in a special chair. Based on the fields previously marked on the skin, the irradiation zones will be accurately determined. Therefore, you should not move during irradiation. You need to lie calmly, without much tension, breathing should be natural and uniform. You will be in the office for 15-30 minutes.
Before turning on the unit, the medical staff goes to another room and watches you on TV or through a window. You can communicate with him through the loudspeaker.
Some parts of radiotherapy machines may move and make noise during operation. Don't worry - the whole process is controlled.
The irradiation itself is painless. If you feel unwell during radiation exposure, tell your doctor immediately without taking any action on your own. The installation can be turned off at any time.
It is possible that already at the beginning of treatment you will feel a decrease in pain (if any). However, as a rule, the greatest therapeutic effect of radiation therapy occurs after completion of the course of treatment.
To obtain a good therapeutic effect, it is very important that you complete all prescribed treatment sessions.
How to behave during radiation therapy
The body's response to radiation therapy varies from person to person. However, in any case, the radiation therapy process represents a significant burden on the body. Therefore, you may develop a feeling of fatigue during treatment. In this regard, you should rest more. Go to bed when you feel the need.
The sensation usually goes away within 4-6 weeks after completing treatment. However, you should not completely avoid physical activity, which increases the body's defenses and resistance to harmful influences. You can get recommendations on the selection and dosage of physical activity from your doctor and a physical therapy specialist.
During treatment you should follow some rules
- Eat well. Try to stick to a balanced diet (ratio of proteins, fats and carbohydrates 1:1:4). Along with food, you need to take 2.5-3 liters of liquid per day (fruit juices, mineral water, tea with milk).
- Give up bad habits (smoking, drinking alcohol), at least for the period of treatment.
- Do not wear clothing that is tight to the areas of your body being irradiated. Items made from synthetic fabrics and wool are extremely undesirable. Loose, old cotton clothing is preferred. If possible, the areas of skin to be irradiated should be kept open.
- Get outdoors more often.
- Carefully monitor the condition of your skin. Irradiated skin sometimes appears tanned or darkened. By the end of treatment, in some cases, the irradiated areas of the body may become excessively moist (especially in the folds). This largely depends on your individual sensitivity to radiation. Tell your doctor or nurse about any changes you notice. They will give appropriate recommendations.
- Do not use soap, lotions, deodorants, ointments, cosmetics, perfumes, talc or other similar products on the exposed area of your body without consulting your doctor.
- Do not rub or scratch the area of skin being treated. Do not place warm or cold objects (heating pad, ice) on it.
- When going outside, protect the exposed part of the skin from the sun (light clothing, a wide-brimmed hat).
What awaits the patient after radiation?
Side effects of radiation
Radiation therapy, like any other type of treatment, can be accompanied by general and local (in the area of irradiation on tissue) side effects. These phenomena can be acute (short-term, occurring during treatment) and chronic (developing several weeks or even years after the end of treatment).
Side effects of radiotherapy most often occur in tissues and organs directly exposed to radiation. Most side effects that develop during treatment are relatively mild and can be treated with medication or proper nutrition. They usually disappear within three weeks after the end of radiation therapy. Many patients experience no side effects at all.
During treatment, the doctor monitors your condition and the effect of radiation on body functions. If you experience any unusual symptoms during treatment (cough, sweating, fever, unusual pain), be sure to tell your doctor or nurse.
Common side effects of radiation therapy
Emotional condition
Almost all patients undergoing cancer treatment experience some degree of emotional stress. The most common feelings are depression, fear, melancholy, loneliness, and sometimes aggression. As the general condition improves, these emotional disturbances become dull. Communicate more often with family members and close friends. Don't isolate yourself. Try to take part in the lives of the people around you, help them and do not refuse their help. Talk to a therapist. Perhaps he will recommend some acceptable methods of relieving tension.
Fatigue
Feelings of fatigue usually begin within a few weeks of starting treatment. It is associated with significant physical stress on the body during radiation therapy and stress. Therefore, during the period of radiation therapy, you should slightly reduce your overall activity, especially if you are used to working at a strenuous pace. However, do not completely avoid housework; take part in family life. Do things that you enjoy more often, read more, watch TV, listen to music. But only until you feel tired.
If you do not want others to know about your treatment, you can take a vacation during the treatment period. If you continue to work, talk to your manager - he may change your work schedule. Don't be afraid to ask your family and friends for help. They will certainly understand your condition and provide the necessary support. After completing the treatment, the feeling of fatigue gradually disappears.
Blood changes
When large areas of the body are irradiated, the number of leukocytes, platelets and red blood cells in the blood may temporarily decrease. The doctor monitors hematopoietic function using blood tests. Sometimes, with pronounced changes, a break in treatment is taken for one week. In rare cases, medications are prescribed.
Decreased appetite
Radiation therapy usually does not cause nausea or vomiting. However, there may be a decrease in appetite. You must understand that in order to repair damaged tissues, you must eat enough food. Even if you don't feel hungry, you need to make an effort to eat a high-calorie, high-protein diet. It will make it possible to better cope with side effects and improve the results of cancer treatment.
Some nutritional tips during radiation therapy:
- Eat a variety of foods often, but in small portions. Eat when you want, regardless of your daily routine.
- Increase the calorie content of food - add more butter if you like its smell and taste.
- To increase your appetite, use a variety of sauces.
- Between meals, consume kefir, a mixture of milk with butter and sugar, and yogurt.
- Drink more fluids, preferably juices.
- Always have a small supply of foods you like (approved for storage in the clinic where treatment is carried out) and eat them when you feel like eating something.
- While eating, try to create conditions that improve your mood (turn on the TV, radio, or listen to your favorite music while eating).
- Talk to your doctor about drinking a glass of beer with meals to increase your appetite.
- If you have any medical conditions that require you to follow a specific diet, talk to your doctor about ways to vary your diet.
Side effects on the skin
The skin's reaction to radiation is manifested by redness in the area of exposure. In many ways, the development of this phenomenon is determined by your individual sensitivity to radiation. Redness usually appears at 2-3 weeks of treatment. After radiation therapy is completed, the skin in these areas becomes slightly dark, as if tanned.
To prevent an overly pronounced skin reaction, you can use vegetable and animal oils ("Children's", "Velvet" cream, aloe emulsion), which should be applied to the skin after a radiation therapy session.
Before the session, you need to wash off the remaining cream with warm water. However, the skin should be lubricated with appropriate ointments and creams not from the first days of irradiation, but later, when the skin begins to redden. Sometimes, if there is a severe radiation reaction of the skin, a short break in treatment is taken.
For more information about skin care, consult your healthcare professional.
Side effects on the mouth and throat
If you are receiving radiation to the maxillofacial area or neck, in some cases the mucous membrane of the gums, mouth and throat may become red and inflamed, and you may experience dry mouth and pain when swallowing. Usually these phenomena develop in the 2-3rd week of treatment.
In most cases, they go away on their own within a month after completion of radiation therapy.
You can alleviate your condition if you follow the recommendations below:
- Avoid smoking and alcohol during treatment as they also cause irritation and dryness of the oral mucosa.
- Rinse your mouth at least 6 times a day (after sleep, after each meal, at night). The solution used must be at room temperature or refrigerated. What solutions are best for rinsing the mouth can be found out from your doctor.
- Twice a day, gently, without pressing hard, brush your teeth with a soft toothbrush or cotton swab (after use, rinse the brush thoroughly and store dry).
- Consult your dentist for the right toothpaste. It should not be harsh and irritate the mucous membranes.
- If you use dentures, remove them before your radiation therapy session. If dentures rub your gums, it is better to temporarily stop using them.
- Do not eat sour, spicy foods.
- Try to eat soft foods (baby food, purees, cereals, puddings, jellies, etc.). Soak hard and dry foods in water.
Side effects on the mammary gland
When undergoing radiation therapy for a breast tumor, the most common side effect is skin changes (see section "Side effects on the skin"). In addition to following the above skin care recommendations, you should avoid wearing a bra during the treatment period. If you feel uncomfortable without it, use a soft bra.
Radiation therapy may cause pain and swelling in the breast area, which will disappear or gradually decrease after treatment is completed. The irradiated mammary gland can sometimes become larger (due to fluid accumulation) or smaller (due to tissue fibrosis).
In some cases, these deformations of the shape of the gland can persist for the rest of life. You can find out more about the nature of changes in the shape and size of the mammary gland from your attending physician.
Radiation therapy may impair shoulder motion. Consult a physical therapy specialist about what exercises you should do to prevent this complication.
In some patients, radiation therapy may cause swelling of the arm on the side of the irradiated gland. This swelling may develop even 10 years or more after completion of treatment. Therefore, it is necessary to carefully monitor the condition of your hand and adhere to certain rules of behavior:
- Avoid heavy lifting (no more than 6-7 kg), vigorous movements requiring excessive effort (pushing, pulling), or carrying a bag over your shoulder on the side of the irradiated breast.
- Do not allow blood pressure to be taken or injections (blood drawn) into the arm on the side being treated.
- Do not wear tight-fitting jewelry or clothing on this arm. If you accidentally damage the skin of your hand, treat the wound with alcohol (but not alcohol tincture of iodine!) and cover the wound with a bactericidal plaster or apply a bandage.
- Protect your hand from direct sunlight.
- Maintain your optimal weight through a balanced, low-salt, high-fiber diet.
- If you experience even occasional hand swelling that goes away after a night's sleep, contact your doctor immediately.
Side effects on the chest organs
During radiation therapy, you may have difficulty swallowing due to radiation inflammation of the esophageal mucosa. You can make eating easier by eating small meals more often, thinning thick foods, and cutting solid foods into pieces. Before eating, you can swallow a small piece of butter to make it easier to swallow.
You may develop a dry cough, fever, change in sputum color, and shortness of breath. If you notice these symptoms, tell your doctor immediately. He will prescribe special drug treatment.
Side effects on the rectum
This may occur during radiation therapy for cancer of the rectum or other pelvic organs. With radiation damage to the intestinal mucosa, pain and bleeding may appear, especially with difficult stool.
In order to prevent or reduce the severity of these phenomena, it is necessary to prevent constipation from the first days of treatment. This can be easily achieved by organizing an appropriate diet. It is necessary to additionally include kefir, fruits, raw carrots, stewed cabbage, prune infusion, tomato and grape juice in the diet.
If, despite following the recommendations, you experience stool retention for more than 1-2 days, be sure to inform your doctor about this.
Side effects on the bladder
Radiation therapy sometimes causes inflammation of the lining of the bladder. This can lead to frequent painful urination and increased body temperature. Occasionally, the urine becomes reddish in color. If you notice these symptoms, tell your doctor. These complications require special drug treatment.
How to behave after completion of radiation therapy (post-radiation period)
After completing a course of radiotherapy, it is very important to periodically check the results of your treatment. You should have regular follow-up examinations with a radiologist or the doctor who referred you for treatment. The time of the first follow-up examination will be determined by the attending physician upon discharge.
The schedule for further observation will be drawn up by the doctor at the clinic or dispensary. These same specialists will, if necessary, prescribe further treatment or rehabilitation for you.
Symptoms for which you should consult a doctor without waiting for the next follow-up examination:
- the occurrence of pain that does not go away on its own within several days;
- nausea, diarrhea, loss of appetite;
- increased body temperature, cough;
- the appearance of a tumor, swelling, unusual rashes on the skin;
- development of limb edema on the irradiated side.
Care for irradiated skin
After completion of treatment, it is necessary to protect the irradiated skin from injury and sunlight for at least a year. Be sure to lubricate the irradiated areas of the skin with a nourishing cream 2-3 times a day, even when it has healed after treatment. Do not treat your skin with irritating products.
Ask your doctor which cream is best to use. Do not try to erase the marks left after irradiation; they will gradually disappear on their own. Give preference to showering over bathing. Do not use cold or hot water. When taking a shower, do not rub the irradiated areas of the skin with a washcloth. If irritation of irradiated skin persists for a long time, consult a doctor. He will prescribe appropriate treatment for you.
Remember: mild pain in the irradiated area is common and quite common. If it occurs, you can take mild painkillers. If pain is severe, consult a doctor.
Relationships with relatives and friends
Radiation therapy does not make your body radioactive. It should also be clearly understood that cancer is not contagious. Therefore, do not be afraid to communicate with other people, friends and relatives during and after treatment.
If necessary, you can invite those closest to you to have a joint conversation with your doctor.
Intimate relationships
In most cases, radiation therapy does not have a significant effect on sexual activity. The decrease in interest in intimate relationships is caused mainly by the general physical weakness that occurs during this treatment and stress. Therefore, do not avoid intimate relationships, which are an important part of a fulfilling life.
Professional activity
When radiation therapy is performed on an outpatient basis, some patients do not stop working at all during the course of treatment. If you did not work during treatment, you can return to your professional activity as soon as you feel that your condition allows it.
If your job involves strenuous physical activity or occupational hazards, you should consider changing your working conditions or profession.
Leisure
Pay more attention to rest. You will regain your strength over time, so do not return to full physical activity right away. Visit theaters and exhibitions. This will allow you to take your mind off unpleasant thoughts.
Make it a rule to take daily walks in the fresh air (walks in the park, in the forest). Communicate more with friends and family. With the knowledge of your attending physician, consult with a physical therapist and psychotherapist. They will help you choose adequate physical activity (health-improving gymnastics) and suggest ways to overcome stress.
Conclusion
We hope that this information will help you get rid of unnecessary nervous tension, make it easier to undergo radiation therapy, and understand what awaits you after it. All this contributes to your recovery.
For more detailed information on issues related to your health, please contact your physician.