Malignant tumors can form in almost all anatomical areas. Thus, oral cancer, the symptoms of which sometimes appear only in late stages, is not a rare form of oncology.
This disease is found among heavy smokers, chewing tobacco lovers and other categories of patients. Early treatment helps minimize the effects of tumor growth in the mouth.
What is oral cancer
Regular examination by a doctor - prevention
Oncological diseases of the oral cavity are caused by malignant cell growth in various tissues of this anatomical region. Since almost the entire oral cavity is lined with epithelial tissue, the likelihood of developing cancer is quite high.
This does not mean that anyone is susceptible to this disease. For tumor growth to occur, the influence of negative factors is necessary.
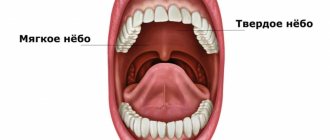
Malignant growth can affect the following parts of the oral cavity:
- Lips.
- Gums.
- Language.
- Buccal mucosa.
- Sky.
- Floor of the mouth.
The most common tumors are the tongue, the inner lining of the cheeks and the floor of the mouth. The clinical picture and the rate of spread of tumor cells depend on the location of the disease. When a tumor grows in the buccal area, the salivary glands may be affected.
Care after surgery for oral cancer
Changes in diet
You will be able to drink fluids immediately after surgery. Your doctor will tell you when you can start taking pureed foods. You can start eating soft foods when your doctor allows, as long as you can tolerate them.
Read the resource Recommendations for Pureeed and Mechanically Gentle Diets for nutritional recommendations. You can also take liquid supplements that are high in protein and calories. For example, Ensure®, Boost® and Carnation Instant Breakfast®. Do not eat regular solid foods until your doctor tells you to.
If you have had surgery on the lining of your mouth or lower gum, chew food on the other side of your mouth until you have your first doctor's appointment after surgery.
Oral care
- Your doctor will tell you whether you can brush your teeth after surgery.
- Keep your mouth clean with rinses or an oral irrigation device. Your nurse will give you an oral irrigation device and teach you how to use it.
- To make a rinse solution, mix 1 quart (250 ml) warm water with 1 teaspoon salt and 1 teaspoon baking soda. You can store it at room temperature. Do not use mouth rinses that contain alcohol. They can cause oral irritation and slow healing.
Caring for the incision
- Do not wet the stitches on your lip or neck for the first 48 hours (2 days). After 48 hours, you can shower as usual. Do not direct the water stream towards the cut itself. Instead, let the water run down the cut and pat it dry with a clean towel.
- Apply bacitracin ointment twice daily if your doctor tells you to do so. Before you leave the hospital, you will be given bacitracin if you need it.
- The absorbable sutures will loosen and fall out 6 to 8 weeks after surgery. When you feel them in your mouth, simply spit them out. As long as they stay in place, they don't require much care other than keeping your mouth clean.
- Non-absorbable sutures will be removed at your first appointment with your doctor after surgery.
- If you have had lip surgery, avoid stretching your lip, such as when smiling, until the area has healed.
Speech changes
- If you have had surgery on your tongue, floor of your mouth, or soft palate, your speech may change. Your tongue may become swollen and numb, and you may not be able to move it freely. This will subside as the area heals. If you have significant changes in your speech, you will be referred to a speech therapist for further help.
Anesthesia
- Most people experience pain or discomfort after surgery. You will be given a prescription for pain medication before you leave the hospital. Take it as prescribed.
- If pain medication doesn't help, call your doctor.
- Painkillers may cause constipation (having bowel movements less frequently than usual). To prevent constipation, take a stool softener such as docusate sodium (Colace®) 3 times daily. If this does not help, take a laxative (eg 2 Senokot® tablets) before bed. Both drugs are available without a prescription. If constipation persists after taking these medications, call your doctor. For more information, read the resource Constipation.
Follow-up appointment
The day after surgery, call your doctor to make a follow-up appointment.
to come back to the beginning
Causes
Oral cancer
The mechanism of development of oral cancer is generally similar to the stages of formation of any malignant tumor. Healthy epithelial cells, after dividing, perform their functions and are gradually destroyed.
Cell division is regulated by genetic information and special intracellular mechanisms. Under certain conditions, the division process can be disrupted, resulting in the formation of an abnormal cell mass called a malignant tumor.
Metastases. Diagnostics
At the Yusupov Hospital, doctors diagnose metastatic cancer using modern research methods:
- tomographic (MRI, CT, PET-CT);
- scintigraphy of skeletal bones;
- Ultrasonography;
- various diagnostic punctures under visual control of a tomograph;
- full laboratory examination, including determination of the level of tumor markers in biological fluids, immunological and molecular genetic;
- endoscopic (gastroscopy, bronchoscopy, colonoscopy) diagnostics with biopsy;
Symptoms and signs
Poorly healing ulcers are a warning sign
Symptoms of any cancer can be variable. Often patients do not have any complaints until the tumor becomes large enough.
Symptoms depend on the location of the malignant growth and the individual body's response to the disease.
The most common symptoms include:
- The appearance of a lump, thickening, rough patch, or slight swelling in any area of the oral mucosa.
- Unexplained bleeding in the mouth.
- Numbness and loss of sensation in the face or neck.
- Constant appearance of sores in the mouth area.
- Painful sensations while eating food.
- Difficulties with chewing and swallowing. Speech dysfunction.
- Partial numbness of the tongue.
- Pain in the ear area.
- Gradual decrease in body weight.
The listed signs are not specific to oncology and may indicate a variety of diseases of the oral cavity. However, if such symptoms are detected, you should consult a doctor for a detailed diagnosis.
Symptoms of gum cancer
- Firstly, any person should be alert to the breakdown of tissue in a certain area. Gum cancer is characterized by the formation of a growth of a certain size. It is imperative to pay attention to the appearance of numerous blood capillaries on this neoplasm.
- Secondly, the appearance of various seals of various configurations is abnormal for gum tissue.
- Thirdly, bleeding increases, accompanied by constant swelling of the gums.
If any suspicious symptom appears, the best option is to contact a specialist. Based on a personal examination, blood tests and other studies using modern equipment (radiography, tomography), the dentist will make a preliminary diagnosis. This disease is hidden behind the symptoms of gingivitis, leukoplaxia, leukoplaxia or ulceration.
Diagnostic methods
If you suspect a disease, you should contact an oncologist. During your appointment, your doctor will ask about your complaints, take a medical history, and examine your mouth to look for signs of malignant growth.
Any abnormality of the epithelial mucosa may be suspected, including areas of irritation, ulcers and white spots. To exclude other diseases and confirm oncology, instrumental and laboratory research methods will be required.
Special research methods:
- Sampling of a section of the oral mucosa followed by histological examination. A biopsy is the most accurate method for diagnosing cancer and identifying the type of malignant tumor. Also, the results of the method may indicate precancerous changes in the epithelium, which increase the risk of cancer.
- Endoscopic examination. During the procedure, a small flexible tube equipped with a camera and a light source is placed down the patient's throat. The nasal cavity is examined in the same way. Endoscopy is necessary to detect the primary area of tumor spread if oral cancer is a secondary formation.
- Visualization. To obtain high-precision images of certain tissues and organs, doctors prescribe radiography, as well as computer or magnetic resonance imaging. These methods are useful for assessing tumor size and finding the primary site of malignant tissue spread.
Screening diagnostic methods aimed at detecting the early stages of oncology are also important. If a patient has certain risk factors, regular examinations are necessary.
Diagnosis and treatment of gum cancer
Gum cancer is quite rare, but is characterized by the aggressiveness of the tumor process. If the disease is diagnosed at an early stage, the five-year survival rate is 80%, in the third stage of cancer - 40%. The diagnosis can be made by examining the oral cavity, but often novice doctors consider bleeding to be a sign of periodontal disease.
Oncologists at the Yusupov Hospital immediately perform a biopsy and send the biological material for cytological examination. If atypical cells are detected in the preparation, surgical intervention is performed - removal of the tumor and surrounding tissues. In advanced stages of gum cancer, additional resection of part of the tongue and jaw is performed. Undesirable consequences of the operation include:
- Difficulty swallowing;
- Impaired sense of taste;
- Smell disorder.
Before surgery, the patient is prescribed radiation therapy, the purpose of which is to destroy cancer cells. In the postoperative period, chemotherapy is administered to prevent relapse of the disease. Treatment of malignant gum tumors at home or using alternative methods of therapy is futile. If you have the first signs of gum cancer, call the Yusupov Hospital.
Forecast
The survival period directly depends on the type of tumor and the stage of spread. During the first stage, when malignant cells remain on the surface of the mucous membrane, surgery helps to completely get rid of the problem.
A poor prognosis is typical for late stages, when tumor cells have spread to the deep cervical lymph nodes. In this case, survival rarely reaches two years.
Thus, oral cancer, whose symptoms may be nonspecific, is best treated in its early stages of growth. Screening diagnostics help detect precancerous changes and prevent tumor growth.
Informative video about oral cancer - in the video:
Neoplasms
Before starting prosthetics, each patient undergoes a thorough examination to identify various diseases and neoplasms in the oral cavity. Sometimes, it makes it possible to identify tumors (including malignant ones) at the moment of their inception, when the patient is not even aware of it. And this is an opportunity to start treatment early, resulting in a complete recovery. Basically, the palpation method is used for this, when the doctor manually checks every centimeter of the patient’s oral cavity.
And although malignant neoplasms are rarely detected, it is recommended to conduct such examinations regularly, since, unlike tumors on other parts of the body, any neoplasms in the oral cavity are better treated and prevented. But to protect yourself, you need to know the main symptoms of this disease. No wonder they say: “Forewarned is protected.”
There are many diseases that are asymptomatic, do not manifest themselves externally and do not cause any trouble to a person. The patient may not realize that everything is not all right with him, while the disease develops more and more. And only in the last stages can the first signs appear, sometimes very unpleasant and painful, along with complications. Such pathologies are not uncommon in dentistry. One of these insidious diseases is a dental cyst.
What is it - a dental cyst?
Generally speaking, a cyst is a formation filled with fluid and having a dense shell. In dentistry, a dental cyst refers to a formation in the bone filled with liquid content (mainly dead epithelial cells and bacteria). The disease occurs due to an untreated infection in the tooth. The cyst has a dense shell (this is a protective reaction of the body so that the inflammatory process does not develop further). But this does not prevent it from growing and reaching sizes of 3-4 cm or more. Many people are dismissive of this type of formation, but a cyst can cause very serious complications - even cancerous tumors, and therefore is a rather dangerous disease.
Reasons for education
A dental cyst can form for a variety of reasons, ranging from an unsuccessful fall, which causes a tooth injury, to a banal unsuccessful root canal treatment. To find out exactly why the cyst formed, the doctor conducts a detailed survey and refers the patient to additional research methods.
The most common causes of dental cysts are the following factors:
- Trauma (tooth displacement provokes infection and rapid proliferation of microorganisms, since dirt and a large number of pathogenic bacteria usually get into the wound)
- Poor treatment of caries (as a result, an infection enters the root canal and provokes a new inflammatory process - a cyst)
- Unsatisfactory endodontic treatment (again, the negative impact of pathogenic microflora and the formation of a focus of inflammation)
- Common diseases in which pathogenic bacteria enter the jaw tissue along with the bloodstream
- Complication of sinusitis (with cysts on the upper jaw)
- Chronic inflammatory processes under the crown
- Chronic periodontitis (if left untreated, the infection progresses and a root cyst occurs
- Diseases of the nasopharynx
- Difficult eruption of wisdom teeth. Typically, this results in the formation of a “hood” - a part of the gum that covers the unerupted part. Bacteria multiply there and penetrate deep into the tooth, causing the formation of a cyst.
Dentists give first place among the causes of cysts to two main ones: dental trauma and root canal infection. Therefore, it is very important to try to avoid infection in the tooth - it is this that triggers the inflammatory process.
Symptoms of a dental cyst
The particular danger of the disease lies in the fact that its first signs appear when the cyst is already of impressive size. The early stages do not manifest themselves at all. Cysts form rather slowly - the process is measured over weeks. Therefore, the patient has time to detect warning signs that may indicate the occurrence of a dental cyst:
A tubercle on the gum near the root of the tooth, increasing in size over time (due to the accumulation of fluid in the cyst cavity)
Unpleasant sensations when eating solid foods (caused by pressure on the gums from pieces of food)
Formation of a fistula (communication between the oral cavity and bone in the form of a hollow tract)
Malaise, fever along with jaw pain
Headaches that do not go away when taking pills (with cysts that form in the maxillary sinus)
It should be especially noted that toothache with cysts is not as severe as caries - it can be called nagging. If the cyst becomes inflamed, the pain becomes stronger.
A person may not associate these signs with any disease, believing that he “rubbed” his gums, scratched his tongue, etc. But in fact, this may be the most real cyst, but, unfortunately, it is really not easy to recognize it.
Diagnostics
As a rule, a dental cyst is discovered completely by accident - during a routine examination or treatment of a neighboring tooth. The disease is detected radiographically.
The picture shows a round dark spot with clear contours, located at the top of the tooth root (surrounding it in the form of a “halo”). If the doctor has doubts about whether it is a tumor or a cyst, he sends the patient for puncture of the cyst. In this case, the cyst is punctured, fluid is taken with a needle, and it undergoes a histological examination to determine if the cells are cancerous.
Cyst treatment
Dental cysts are treated both therapeutically and surgically. Now doctors are trying to save the tooth as much as possible. The “pitfall” in treatment is the fact that some cysts continue to grow even after tooth extraction, and after any method the tooth must be monitored.
The therapeutic method is applicable for early treatment and small cysts (up to 0.8 cm in diameter).
First, the tooth itself is treated and the canals are filled. Even if the tooth has been treated previously, the canals must be unsealed and treated with an antiseptic.
Then the doctor will perform a copper-calcium depophoresis procedure.
A suspension of copper and calcium is injected into the tooth, and then an electric current is applied.
It takes 3-5 sessions, after which the tooth can be filled.
The method is very controversial, it has many opponents and supporters. Doctors who advocate this procedure talk about the possibility of saving the tooth and being gentle on dental tissues. Doctors who do not use this method argue about the possibility of cyst recurrence and loss of time.
Of course, the decision must be made on an individual basis.
The surgical treatment method is divided into the following types:
Cystotomy. Incomplete removal of the cyst. It is carried out for large cysts (more than 1.5 cm), when they cannot be completely removed due to possible damage to neighboring tissues.
Cystectomy. Complete removal of the formation, most often along with the root tip. An incision is made in the gum, the cyst and root tip are removed, the canal is immediately filled and the gum is sutured.
Retromolar cysts must be removed along with the tooth. For large cysts, a bone replacement drug is injected into their cavity (the most popular today are Cerabon, JASON, Maxresorb).
Any surgical method is accompanied by the prescription of antibiotics, anti-inflammatory drugs (usually Tsiprolet), antihistamines (according to indications and individual tolerance).
Possible complications
A cyst that is not diagnosed in a timely manner grows, destroys bone tissue and provokes the formation of connective tissue. Complications can then lead to the tooth being lost.
Most often, doctors record the following complications:
- Purulent inflammation of the cyst (threatens a severe inflammatory process throughout the entire jaw, namely osteomyelitis)
- Melting of the bone tissue of the jaw (occurs due to the growth of a cyst, again leading to osteomyelitis)
- Lymphadenitis (inflammation of the lymph nodes, threatening further spread of infection)
- Chronic sinusitis (when a cyst grows into the maxillary sinus)
- Periostitis (inflammation of the periosteum)
- Abcess on the cheek or gum (occurs due to severe inflammation)
- Fracture of the jaw as a result of thinning of the bone in the place where the cyst formed
- Cellulitis is a severe complication in which soft tissues become inflamed, and general blood poisoning is possible
- Degeneration of cyst cells into malignant ones, then a tumor forms
Some complications can directly threaten a person’s life, so in no case should a dental cyst be treated with disdain and reasoned at the level of “it will resolve on its own.” The cyst can become inflamed, rupture, but not resolve, and treatment is necessary.
Prevention
It is impossible to avoid the occurrence of a cyst, but it is clearly visible at an early stage during an X-ray examination, so get it done every year. This way you will avoid its growth (if detected) and will be protected from many complications.
Visit your dentist regularly and have your teeth and nasopharyngeal diseases treated in a timely manner. If you have any discomfort in your mouth, get it checked by a doctor.
Be sure to brush your teeth properly - this is the prevention of many oral diseases. Simple preventive measures will help you avoid serious problems and provide quality treatment if a cyst is detected, possibly without surgical intervention.
And every tooth saved is a victory.
Possible life expectancy and prognosis
Unfortunately, it is impossible to provide comprehensive information regarding these aspects. The following can affect how long a person will live after diagnosis:
- characteristics of the primary tumor;
- timing of its diagnosis;
- number of metastases in the spine;
- general condition and mood of the patient;
- the patient has other diseases;
- chosen type of treatment.
Prognosis largely depends on the timing of diagnosis
On a note! Only 1/5 of all patients live longer than a year from the moment of diagnosis of spinal metastases. The prognosis is unfavorable.
Metastases usually appear only in the last stages of development of the primary cancer. And this is what significantly affects the overall forecast. Without medical care, a person affected by cancer and having metastases lives for several months. And treatment can increase life expectancy by 1-2 years.
Stomach cancer. Dynamics of patient survival under various chemotherapy regimens
If the tumor grows slowly, its size is small, and there are only a few metastases in the spine, then the person, as a rule, lives longer (with treatment). If the situation is characterized exactly the opposite, then you should not expect a long life expectancy and you need to prepare for the worst.
Diagnostic features
On a note! With a single metastasis in the spine, there is a prognosis that a person will live 5 or more years (the chances are about 49%). Typically, tumor resection and vertebrectomy are performed, that is, vertebral augmentation.
Dental and gum disease linked to increased risk of liver cancer
Doctors have discovered a connection between diseases of the teeth and gums and an increased risk of liver and gallbladder cancer, according to the United European Gastroenterology Journal
. In people with diseases of the teeth and gums, it is on average 30 percent higher than in healthy people. Other factors the researchers named were smoking, being overweight or obese, and not eating enough fruits and vegetables.
Gingivitis (inflammation of the gums), periodontitis (inflammation of the connective tissue between the tooth and the tooth socket) and caries directly indicate poor health of the teeth and gums. It, in turn, is a risk factor for heart disease, diabetes, stroke and various types of cancer, including cancer of various parts of the gastrointestinal tract. A meta-analysis of eight studies found that people with periodontitis and tooth loss had an increased risk of developing pancreatic cancer. And a study of Taiwanese residents who were treated for periodontitis linked the treatment to a reduced risk of various types of cancer. On the other hand, a meta-analysis of six studies examining the relationship between dental disease and colon cancer in residents of the United States and China did not reveal it.
Doctors from Queen's University in Belfast, led by Haydée Jordão, decided to find out whether there is a correlation between poor dental health and the development of gastrointestinal cancer in UK residents. To do this, they took data from the UK Biobank, the largest center for research into health problems in the country. The screening, which was carried out between 2006 and 2010, involved 500,000 Britons aged 40 to 69 years, and monitoring their health continues to this day. At the initial stage, blood, urine and saliva were taken from the participants for tests, and their height and weight were measured. They also participated in a survey and provided comprehensive information about their health. The questionnaire included questions about whether a person’s gums hurt and bleed, and whether their teeth hurt or fall out.
The authors of the new study took information from the Biobank on 469,628 Britons who spoke in detail about the health of their teeth and gums. Subsequently, scientists monitored the health status of the volunteers until September 30, 2014, or until cancer was diagnosed or death. Then, using Cox regression, which predicts the risk of an event, the scientists calculated risk ratios (RR) for developing gastrointestinal cancer depending on dental health for study participants.
It turned out that during the observation period 4,069 people (less than one percent) developed cancer. 13 percent of them had dental problems. As a result, the researchers found no connection between poor dental health and the occurrence of gastrointestinal cancer in general (CR 0.97). However, people with bad teeth had a higher risk of cancer of the liver, gallbladder and bile ducts (HR 1.32), and the risk of hepatocellular carcinoma (the most common type of liver cancer) was even higher (HR 1.75). Among people with bad teeth, the risk of developing cancer was higher in those who ate little vegetables and fruits (CR 1.51), those who smoked (CR 1.51), and were overweight or obese (CR 1.53).
According to the study authors, the oral microbiome may play a role in the development of cancer. It is known that some bacteria, such as Plaut's bacillus ( Fusobacterium nucleatum
) or
Porphyromonas gingivalis
, which contribute to gum disease, also cause liver abscess. Plaut's bacillus, in addition, may influence the development of intestinal cancer. Therefore, researchers believe that they may also be associated with the occurrence of liver cancer, but whether this is true is still unknown.
For proper oral hygiene, it is often recommended to use dental floss in addition to toothbrushes - in the USA, for example, recommendations for the use of dental floss appeared back in 1979.
However, as it turned out several years ago, these recommendations are not scientifically substantiated. Journalists from the Associated Press analyzed 25 papers on this topic over the past 10 years and found that the evidence was unreliable and of low quality. Ekaterina Rusakova
Diagnosis, treatment
Only a doctor can determine the presence of metastases in the spine based on the collected medical history, as well as the results of tests and studies. The patient may be referred for a CT or MRI of the spinal column, radiography, etc. They may also prescribe a blood test for tumor markers, scintigraphy, or osteodensitometry. If the vertebrae are affected, a biopsy, which is usually prescribed in the presence of cancerous tumors, cannot be performed. If it is known which organ became the source of metastases, then additional examination methods such as mammography or ultrasound of internal organs may be prescribed.
Osteodensitometry
Attention! The earlier a primary malignant tumor is detected, the greater the chance of a successful outcome. Very often, timely diagnosis is crucial. Although sometimes it is impossible to identify the root cause of metastases.
Treatment is extremely difficult and often useless. It consists of the use of chemotherapy, hormonal therapy, radiotherapy, certain types of surgical operations, etc. In many ways, therapy will depend on what triggered the formation of metastases, as well as on the condition of the patient as a whole.
Chemotherapy
Hormonal therapy is prescribed for neoplasia, and to combat hypercalcemia, diphosphonates are used. Indications for surgical intervention may include severe pain and excessively rapid compression of the spinal cord, as well as pathological fractures of spinal segments. There are two types of operations.
- Decompressive , which are classified as simple interventions. But they are characterized by a high probability of relapses and deterioration of the condition due to the progression of metastases. Also called laminectomies.
- Decompressive and stabilizing interventions involve the use of implants and fixators and can provide a long-term effect. They can significantly improve the life of a sick person. But such operations are extremely traumatic and cannot be performed in very severe and serious conditions.
Laminectomy
In some cases, the main goal of therapy is to eliminate pain and improve a person’s quality of life. It is also necessary to try to eliminate the cause of spinal cord compression.
Supportive corset for the spine
If you want to learn in more detail whether it is better to perform an ultrasound of the spine or an MRI, as well as familiarize yourself with the possible risks and contraindications, you can read an article about this on our portal.
How likely is the development of a secondary tumor focus?
The likelihood of metastases depends on a number of factors:
- Type of cancer. There are a number of oncological diseases where metastasis is a rare phenomenon (for example, basal cell carcinoma), while in others, on the contrary, they develop rapidly (for example, melanoma).
- Characteristics of the disease are molecular and genetic.
- Stage of cancer. The higher it is, the higher the likelihood of developing a secondary malignant focus.
- Localization.
- Specifics of growth. Tumors that grow infiltratively metastasize more often and faster than malignant neoplasms that grow superficially.