When do molars erupt?
Molars are the last teeth that erupt in the child’s lower and upper dentition. As a rule, the first units appear on the lower jaw at the age of 12-18 months, a month later molars erupt on the upper row. The second molars appear in a child between 24 and 30 months of age.
Replacement of primary molars of the lower jaw occurs at the age of 6-8 years. In place of the upper units, molars grow only by the age of 9-12 years. However, these are average indicators and may vary depending on individual characteristics.
The timing of eruption depends on the following factors :
- hereditary predisposition;
- the general health of the child;
- congenital features;
- climatic living conditions;
- nature of nutrition;
- gender of the child.
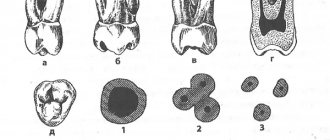
Features of molars
Large molars differ from other groups not only in external characteristics, but also have other features :
- these are the largest units in each dental arch;
- have the largest chewing surface;
- have a powerful root system;
- the upper molars are slightly larger than those on the lower jaw;
- have a stronger surface coating;
- able to withstand weight up to 75 kg;
- upper molars have 4-6 canals, while lower units generally have only 3 canals;
- maxillary molars have 3 roots (palatal, buccal-medial, buccal-distal), less often 4;
- the chewing teeth of the lower jaw have only 2 roots;
- wisdom teeth are the very last molars, which may appear by the age of 50 or not appear at all;
- the last molars are very often located not in the chewing arch, that is, they can grow horizontally or with a slight slope, located buccally or towards the tongue or palate;
- wisdom teeth have from 1 to 5 chewing cusps;
- the last molars often have a complex root configuration (curvature, fusion).
All this entails the peculiarities of treatment of such teeth. The presence of a large number of complex root canals, as well as difficult access compared to other groups of teeth, requires highly qualified doctors and modern equipment for high-quality therapy.
In dental practice, molars are considered the heaviest units, especially wisdom teeth. Proper care and regular preventive examinations will help keep them healthy. When the first signs of damage to the molars appear, we recommend that you immediately sign up for a consultation at our KAS+ dentistry. Timely detection of dental problems guarantees their high-quality treatment with minimal risk and long service life.
Endodontic treatment of lower second molar with four roots
To achieve success in endodontic treatment, it is important not only to know the basics of the anatomical structure of teeth, but also their possible variations, which often require special skills and abilities from the doctor. The anatomical variations of the second molar are among the most varied and interesting of any of the mandibular teeth. During treatment planning, the clinician must consider not only the number of tooth roots, but also the number of canals, their length and orientation, as well as the complexity of the existing bends of the endodontic space, which can be anticipated from the visualized root contour. In particularly complex cases, the targeted radiography method alone may not be enough to take into account all the above-mentioned details; therefore, in such situations, the use of cone beam computed tomography (CBCT) is indicated, which allows one to visualize all the specifics of the endodontist structure without any graphic distortions. Based on CBCT data, the doctor can modify the treatment approach, avoiding the development of a number of iatrogenic errors. As a rule, the number of roots of the second molar ranges from one to three, but the presence of four roots is noted in no more than 1% of cases. In this article we will describe the treatment algorithm for just such a molar, the structure of which can be classified as a developmental anomaly.
The following cases of anatomical configurations of the second molar have been described in the literature: with three separate mesial roots and one distal; with two medial roots and two distal roots; with two medial roots and one distal with an additional radix entomolaris. Despite the presence of a significant number of studies, the prevalence of second molars with four roots in the structure of different populations has not yet been established, with the exception of residents of Israel, in whose environment a four-rooted molar was observed in 0.55% of cases. In this article we will describe a case of treatment of a second molar with four roots and four canals. Obviously, the formation of just such a structure occurred due to the fusion of roots during the process of tooth formation.
Clinical case
An 18-year-old patient sought dental care for sensitivity in the area of the distal tooth of the lower jaw, which responded to cold and temperature stimuli for 15-20 days. In addition, the patient was also concerned about the fact that the tooth was discolored. Her medical history was clear, and clinical examination revealed the presence of a deep carious cavity in the area of the mandibular second molar. A study of electrical odontosensitivity (Digitest II, Parkell) established the presence of a premature reaction to the stimulus, and a cold test (Roeko Endo-Frost, Coltene) provoked the development of severe, prolonged pain. Slight sensitivity was also noted during percussion. During the analysis of the radiograph, the presence of an area of radiolucency (carious cavity) was identified, the bottom of which bordered the pulp chamber (photo 1).
Photo 1. Sight radiograph with visualization of a carious lesion on the second molar of the mandible.
The radiographic contour of the apical region was characterized by the presence of a double shadow from the periodontal ligament, which made it possible to suspect the presence of additional roots. The patient was recommended to undergo CBCT. Axial, coronal and sagittal CBCT slices (CS 9300, Carestream Dental) (internal software version 3.5.15.0 at 5 cm x 5 cm, 85 kV, 8 mA, 20 s, 985 mGy cm2) revealed the presence of type 1 canals in each of the four roots (photo 2-3).
Figure 2: Axial CBCT slice showing four roots.
Photo 3. Three-dimensional image with visualization of four roots.
Taking into account the radiological and clinical data, a diagnosis of irreversible pulpitis with symptomatic apical periodontitis was made. After anesthesia with a 2% solution of lignocaine with a concentration of adrenaline 1:200000 (Xylocaine, AstraZeneca Pharma India Ltd.), the intervention area was isolated with a rubber dam (Hygenic Dental Dam Kit, Coltene). The effectiveness of anesthesia was confirmed by performing a cold test. The access cavity was formed using ESE-014 Endo Safe End burs (SS White). The access cavity was formed in a trapezoidal shape to provide better opportunities for identification of all orifices. During the revision of the bottom of the pulp chamber using an endodontic probe (DG16 Endo Explorer, EXDF166, Hu-Friedy), the presence of two mesial and two distal canals was verified (photo 4).
Photo 4. Visualization of the four orifices during the formation of the access cavity.
Each of the canals was filled with pulp tissue, as evidenced by bleeding from the orifice area. The working length of the canals was determined using a size 10 K-file (NiTiFlex, Dentsply Sirona) and an apex locator (Root ZX mini, Morita) and confirmed using radiographs (Figure 5).
Photo 5. Determination of working length.
Instrumental processing of the canals was carried out using the crown-down technique using nickel-titanium files (HyFlex CM File System, Coltene). Irrigation was provided with 5.25% sodium hypochlorite, 17% ethylenediaminetetraacetic acid (EDTA) solution (EndoPrep solution, Dentsply Sirona) and saline. Obturation was performed with gutta-percha pins (Dentsply Sirona) with a taper of 30/4 for the mesiobuccal (MB), mesiolingual (ML) and distallingual (DL) canals, and 25/04 for the distal buccal (DB) canal (Figure 6).
Photo 6. X-ray with master pins.
The canals were obturated by cold lateral condensation using AH Plus endodontic sealer (Dentsply Sirona). Modified glass ionomer cement (Ketac Nano, 3M Oral Care,) was used to seal the pulp chamber. The coronal part of the tooth was restored with composite material (Tetric N-Ceram, Ivoclar Vivadent) (photo 7). During clinical monitoring, it was confirmed that there were no symptoms that bothered the patient before visiting the dentist. An x-ray obtained 1 year after treatment is shown in photo 8.
Photo 7. X-ray after obturation.
Photo 8. X-ray one year after treatment.
Discussion
Root development begins at the so-called bell stage in the Hertwig epithelial region (HERS), which is located between two mesenchymal structures: the dental papilla and the dental follicle. The apical extension of the root sheath (sheath) curves to form a collar-like structure that grows apically around the dental pulp. With the development of multi-rooted teeth, there is an expansion of many of these collar-shaped formations, which grow from the periphery of the pulp chamber to its center, uniting at a certain moment into a single whole. Thus, in a four-rooted tooth at a certain stage of development, four such collar-like structures should have formed through the invagination of epithelial cells. Variations in the internal and external anatomical structure of teeth are observed with different frequencies among representatives of different ethnic groups and even among individuals of the same nationality. Two-dimensional radiography is an important fundamental tool for diagnosing and assessing the condition of a tooth, however, in cases of identifying unusual changes, it is recommended to resort to CBCT examination, which is characterized by a higher level of accuracy and diagnostic efficiency. In this clinical case, the primary diagnosis of a tooth with four roots was carried out on the basis of targeted radiography data obtained in the medial and distal projections. However, for a detailed assessment of possible anatomical variations and structural features of the endodont, the patient also underwent a CBCT scanning procedure. Data from preliminary studies indicate that mandibular second molars require special attention in terms of diagnosing their endodontic system. Under certain conditions, the doctor cannot identify all the canals and roots, therefore, some of them remain untreated, which leads to the development of corresponding consequences. The number of roots in the second molar of the mandible ranges from one to three. The presence of a third root was noted in 2.8% of representatives of the Mongoloid race, 1.8% of the Negroid race and 1.7% of Caucasians. For these teeth, the most characteristic distribution patterns of canals in the mesial root are type III, IV and II, in the distal root - type I, types II and IV are rarely observed. The prevalence of three-rooted mandibular second molar among the Indian population reaches 8.98%, among the Thai population - 1.2%, among the inhabitants of Burma - 0%. Among Koreans, the presence of c-shaped canals in the second molar of the lower jaw was often noted, and quite rarely, the presence of these teeth with three roots. In some populations, such as Indian and Jordanian populations, two roots and three canals are more common, and c-shaped canals are less common. The incidence of four-rooted first molars in the Japanese population is 0.04%. In the structure of the studies, the presence of four-rooted second molars was noted in 1 clinical case in the study by Zhang et al (2011) and in 8 clinical cases in the study by Shemesh and colleagues (2015). Much more often, the presence of C-shaped roots (up to 293 clinical cases), two roots (up to 387 clinical cases) and three roots (up to 74 clinical cases) was noted. It should be noted that the findings varied significantly among the different ethnic groups of the studies. Clinical cases of identification of a mandibular second molar with four roots have been described by Peiris (2009), Purra (2012), Martins (2014), Rajasekhara (2014), Idris (2014) and Shinde (2016). In most clinical cases, CBCT or spiral CT were used to confirm the presence of four roots.
In the clinical case we described, the patient had two medial and two distal roots, each of which had one full root canal. The lines of formation of the pulp chamber in this situation resemble an “x” figure. Kottoor et al described this form of developmental fusion as a diagnostic criterion for the identification of a four-rooted molar, which was confirmed in our study.
conclusions
Successful endodontic treatment begins with a proper clinical and radiological examination of the patient. Clinicians should be sufficiently informed about the complexities of the anatomical structure of the mandibular second molar and the possible variations in the morphology of the endodontic system. In the clinical case described above, the presence of four roots was suspected based on clinical examination and targeted radiography. CBCT is the main method for detailing anatomical variations, especially in cases of endodontic treatment. After all, the success of this, in fact, depends on the knowledge the clinician has about the potential features of the morphology of the second molar of the mandible, which determine further tactics of iatrogenic intervention.
Authors: Tanvi Paliwal, BDS Rhitu Shekhar, MDS Manoj Kumar Hans, MDS Rohit Paul, MDS Suresh Pandey, MDS