General information
Primary tumors of the skeletal system are rare. They are observed between the ages of 15 and 40 years, that is, children, adolescents and young people are more often affected. In 10% of cases, the disease is detected in people over 60 years of age - in them the tumor may be associated with radiation or develop against the background of benign diseases of the skeletal system. The term “bone cancer” is applied to various types of oncopathology of the skeletal system. Among malignant tumors of this system, the most common are osteogenic sarcoma (synonymous with osteosarcoma in 50-60% of cases), Ewing's sarcoma (the second most common type of tumor), chondrosarcoma , giant cell tumor , fibrosarcoma .
Secondary bone tumors (bone metastases) are much more common. The source of metastatic tumors are primary tumors of the lung, prostate, breast and thyroid gland. Bone sarcomas are a group of tumors of nonepithelial origin. In 80-90% of sarcomas, they are highly malignant tumors that are localized in different bones of the skeleton. However, the tubular bones most often affected are the femur and tibia. The tumor develops in the metaphyses (growth part) of long bones, especially in the area of the knee joint. Men get sick more often than women. An increased risk of the disease is observed with genetic abnormalities: hereditary retinoblastoma and Li–Fraumeni syndrome .
Clinical manifestations of osteosarcoma of the jaw
An early sign of the development of osteogenic sarcoma of the jaw:
pain in a healthy tooth;- itching in the gum area;
- loosening of some teeth.
Jaw pain occurs in the later stages. Sometimes the onset of pain is preceded by a sensory disturbance in the area where the infraorbital and mental nerves diverge. In the place where osteosarcoma develops, a swelling is formed, the density and size of which may vary. Palpation of the tumor is accompanied by slight pain.
If a large tumor forms, the soft tissues swell, the surface above the tumor becomes thinner, and dilated veins become visible under the skin. If a tumor develops in the area of the masticatory muscles of the temporomandibular joint, then at an early stage a contraction of the jaws can be observed. Sometimes osteosarcoma of the jaw in the later stages is accompanied by a pathological fracture.
The onset of the disease is asymptomatic. When the tumor grows to a large size and the process of decay begins, the patient’s body temperature rises to 40˚C. Osteogenic sarcoma of the jaw first penetrates the lungs, then the skeleton is affected.
Pathogenesis
Carcinogenesis is triggered under the influence of many factors, which include:
- radiation treatment for other cancers;
- suppression of tumor suppressor genes;
- prosthetics performed;
- hereditary diseases;
- complex chromosomal aberrations.
Frequent deletion, as well as loss of heterozygosity of 3q13, are specific aberrations for osteosarcomas. One of the tumor suppressor genes is localized in this region, which regulates cell proliferation and plays a major role in tumor pathogenesis. 3q12 deletion is associated with progression and poor prognosis.
An important morphological feature of bone tumors is the infiltrative nature of growth, or circular (encompasses the entire area of the bone around the circumference). The tumor spreads through the bone marrow spaces and replaces them, destroys and surrounds the bone beams. Neoplastic cells are characterized by severe cellular atypia. The architecture of the newly formed bone determines the tumor potential.
Classification
The most common malignant bone tumors are:
- osteogenic sarcoma;
- Ewing's sarcoma;
- chondrosarcoma;
- fibrosarcoma;
- parosteal sarcoma;
- fibrous histiocytoma;
- lymphosarcoma.
Bone sarcoma
The most common tumor develops from osteoblasts and in the process of neoplasm develops altered, atypical bone. This tumor is called differently - synonyms are osteogenic sarcoma, osteosarcoma, osteoidsarcoma, osteoblastosarcoma. Chondrosarcoma and fibrosarcoma are distinguished as independent forms.
Classic osteosarcoma is a highly malignant intraosseous tumor. If a tumor appears in an unchanged bone, it is a primary sarcoma; if it develops after irradiation or against the background of Paget’s disease , it is a secondary sarcoma. The tumor affects the metaphysis (growth zone) of the tubular bone of the arm or leg. Active growth processes occur in the metaphyses, so they are associated with a high risk of tumor transformation. The appearance of a tumor is associated with the rapid growth of bone tissue.
The peak incidence is observed in children aged 10-14 years. They are more likely to affect the tubular bones of the leg - osteosarcoma of the femur in the hip joint, as well as the bones of the knee joint (femur and tibia). When the femur is affected, a large lesion zone of 5-10 cm is revealed. Hemorrhages , necrosis and cystic cavities are found in the newly formed bone. The tumor gradually destroys the periosteum. Sarcoma of the hip occurs at any age, but is more common in young men.
It is characterized by aggressive growth and metastasizes early. Malignant formation of the knee joint in most cases is a secondary metastatic process and less often - as a primary process. In adults, osteosarcoma affects the spine and maxillofacial bones. This type of tumor rarely develops in the area of the coccyx, shoulder girdle, ulna and humerus. Primary osteosarcoma of the ribs is less common, but secondary (metastatic) tumors predominantly affect the ribs, vertebrae and pelvic bones. Malignant transformation of Paget's disease to sarcoma occurs in 1% of cases and the peak incidence occurs at 60 years of age and older. Of all the bones, the jaw is the most commonly affected. Jaw cancer is a tumor with rapid aggressive growth and early metastases to the lungs (most often). There are isolated cases of metastases to the stomach and soft tissues. Damage to the lower jaw is somewhat more common than to the upper jaw (corresponding to 58% and 42%).
Hand bone cancer in most cases is metastatic. In the bones of the skull there are various types of primary sarcomas, as well as secondary metastatic tumors from the primary focus (uterus and prostate). Skull bone tumors cause headaches due to compression of the brain. Spinal cancer is characterized by active growth and rapid progression. Patients develop movement disorders: when the lumbar region is affected, the lower limbs and the functions of the pelvic and genital organs are affected. Cervical spine cancer is very dangerous and requires immediate treatment. When the cervical vertebrae are damaged, the functions of the arms and legs are affected.
Ewing's sarcoma
This type of tumor occurs in children and adolescents. Develops in bone tissue and soft tissues. It is aggressive and metastasizes quickly. There is a high mortality rate in the first year of diagnosis. If we consider damage to the inert system, then in 70% this type of tumor occurs in tubular bones, flat bones (scapula, ribs) and pelvic bones. Compared to osteosarcoma, the diaphyses of bones are more often affected. Many patients have genetic mutations that cause disruption of cell differentiation processes.
Chondrosarcoma
The neoplasm develops from cartilage tissue. Occurs in people over 40 years of age. The course of this type of cancer is difficult to predict. In some, chondrosarcoma develops slowly, while in others it develops very quickly and metastasizes . This type of tumor affects any bone, but the femur and pelvic bones are predominant. The tumor can also develop in flat bones (scapula, skull, ribs). Most often, the course of chondrosarcomas is slow and metastases appear late. The appearance of pain is characteristic, and when the pelvis is damaged, the nerve roots are involved, therefore, in addition to pain, the function of the pelvic organs will be impaired.
Fibrosarcoma
A rare tumor that develops from connective tissue. Tumor cells are located between the collagen of the connective tissue and look like a spindle. In most cases, fibrosarcoma appears after radiation treatment.
Classification of osteosarcomas according to the TNM system
- T0 - no data on the tumor process.
- T1 - formation no more than 8 cm.
- T2 - neoplasm larger than 8 cm.
- T3—tumor continuity is disrupted.
Involvement of lymph nodes (“N”) is rare, since bones do not have a lymphatic system. But if there are metastases to the nodes, this is a poor prognostic sign. Regional lymph nodes are nodes that correspond to the location of the primary tumor.
- N0 - no metastases in the lymph nodes.
- N1 - metastases are present.
Osteosarcoma is characterized by the development of hematogenous metastases, which in the diagnosis of o. By the time of diagnosis, 20% of patients already have small metastases in the lungs. Metastases can also be in the pleura, pericardium, bones, kidneys, and central nervous system.
- M0 - no distant metastases.
- M1 - distant metastases are present (“a” - to the lungs, “b” - to organs and tissues).
An important point is histological examination, which confirms the diagnosis, determines the type of tumor and its malignancy. There are five forms of osteosarcomas, with different degrees of differentiation.
Metastatic bone lesions
The course of metastatic bone lesions is not asymptomatic - pain is the first manifestation of bone metastases. Most patients describe it as unbearable. Patients with metastases also experience:
- pathological fractures of tubular bones;
- vertebral compression fractures;
- spinal cord compression;
- hypercalcemia.
A quarter of breast cancer have fractures of long bones associated with destruction of the cortical layer. radiation therapy or surgery is required .
Benign bone formations
Bones are affected by benign tumors ( chondroblastoma , fibrous dysplasia , osteoclastoma , aneurysmal cyst and others), with which a malignant formation must be differentiated.
Aneurysmal bone cyst
A benign tumor-like bone lesion, which is characterized by the proliferation of connective tissue. It contains cavities filled with blood. A distinctive feature of this cyst is its spread through the epiphyseal plate, as well as to adjacent bones. The cyst appears at any age, but more often in adolescents and children. Its most common location is the bones of the spine, the distal part of the femur, the proximal part of the humerus and tibia, and the pelvic bones. A secondary cyst is formed after damage to benign chondroblastoma , fibrous dysplasia , giant cell tumor and malignant neoplasms - osteogenic sarcoma .
Chondroblastoma
A benign tumor that forms at the articular ends of a bone. It develops from chondroblasts and resembles mature cartilage tissue. It is characterized by slow growth and a favorable course, but there is information about cases of a malignant course or malignancy by chondroblastoma. Like all bone tumors, it affects children and adolescents, and in rare cases, older people. Clinical manifestations are pain and swelling of the joint. Treatment is surgical. The prognosis is favorable.
Aggressive osteoblastoma of the mandible: diagnostic difficulties
Osteoblastoma is a benign tumor that accounts for less than 1% of all bone tumors and most often affects the spine and sacrum of patients at a young age. Less than 10% of all osteoblastomas are located on the skull, and approximately half of them involve the mandible, especially its posterior segments. The very first detailed description of a case of osteoblastoma of the jaw bones was carried out by Borello and Sedano in 1967.
Since the discovery of the tumor by Jaffe and Mayer in 1932, the nomenclature of osteoblastoma has changed dramatically. Names proposed include osteoblastic osteoid-forming tumor, giant osteogenic fibroma, and giant osteoid osteoma. In 1956, this neoplasm was clearly distinguished from osteoid osteoma and identified by Jaffe and Lichtenstein as a separate nosological form: benign osteoblastoma. This name has been approved by the World Health Organization and the Institute of Pathology.
This bone tumor occurs at a young age (on average 20 years) in men and women in a ratio of 2:1. Clinically, the disease is characterized by severe pain lasting from several weeks to a year or more. Radiologically, the tumor may begin to appear as a radiolucent area with poorly or well-defined edges and varying degrees of mineralization. Although the use of radiological examination is very important, the final diagnosis is made only after a histopathological report.
This article describes a case of aggressive osteoblastoma in the posterior segment of the mandible in a 26-year-old woman.
Description of a clinical case.
A 26-year-old woman came to the clinic with complaints of a slowly growing painful swelling in the right posterior part of the lower jaw, which had been developing over the past 3 years. The pain is moderate and intermittent. An external examination revealed a swelling with a smooth surface measuring 3 x 3 cm, affecting the right part of the body of the lower jaw approximately from the symphysis of the chin to the second lower molar on the right side and causing pronounced facial asymmetry. Intraoral examination is unremarkable, the mucous membrane over the swelling is not changed. No lymphadenopathy was detected by palpation.
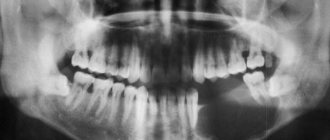
An orthopantomogram reveals a large radiolucent zone affecting the second lower molar on the right side. The formation contains calcified masses approaching the distal root of the second molar, as well as several radiopaque areas located against the background of the clearing zone. This formation was well defined and caused bulging and thinning of the bone tissue of the lower edge of the lower jaw. (Photo 1).
Photo 1: Orthopantomogram. Large single-cavity radiolucent lesion involving the right mandibular second molar, with areas of mineralization
Differential diagnosis included cementoblastoma, osteoid osteoma, ossifying fibroma, and focal cemento-osseous dysplasia.
Subsequently, the tumor was scraped out. The removed tissue, as well as the second molar, was sent for histopathological examination (Figure 2).
Photo 2: Photograph of tissue sample: material obtained after curettage and lower second molar
Light microscopy of the hematoxylin-eosin-stained specimen revealed an irregular bone structure with many cells and loose fibrovascular connective tissue stroma. A large number of areas of osteoid and cementoid formations were also found. The bone was composed of large osteocytes surrounded by a clear rim of osteoblasts (Figure 3a and b). Along the edge of the neoplasm, mature trabeculae are visible, clearly delimited from the rest of the tissue by a demarcation line. The specimen contained giant cells with several nuclei. No atypical mitotic activity was detected.
Figure 3a: Photomicrograph of specimen showing irregular bone, rims of osteoblasts and fibrovascular connective tissue stroma (hematoxylin-eosin, x100)
Figure 3b: Photomicrograph of a specimen showing large osteocytes, modified osteoblast-like cells, surrounded by osteoid substance. (hematoxylin-eosin, x400)
Histopathological examination allowed a diagnosis of aggressive osteoblastoma.
Discussion.
Osteoblastoma is a fairly rare bone tumor for which damage to the jaw bones is not typical. However, cases of its occurrence in the posterior part of the lower jaw have been described. Differential diagnosis is often particularly difficult due to the unclear radiological and clinical appearance, as well as the histological features of this tumor, which sometimes resemble osteosarcoma.
Typical osteoblastomas are biologically benign and limited in growth, typically no more than 4 cm in diameter. But there is also a small group of borderline, more aggressive osteoblastomas. Such tumors cannot be classified as “typical” and are therefore classified as a separate class of lesions with the names: osteoblastoma-like osteosarcoma, malignant osteoblastoma, or aggressive osteoblastoma.
Aggressive osteoblastomas occur at a later age than tumors with a benign course. Clinically, these neoplasms exhibit more aggressive behavior. They can grow into neighboring tissues, and after treatment they recur in 10-21% of cases, but never metastasize. The histological picture is more reminiscent of osteosarcoma than a benign neoplasm. Some authors have stated that the disease called aggressive osteoblastoma is actually a high-grade osteosarcoma that resembles the course of osteoblastoma. Diagnosis is based on the histological features and clinical picture of the lesion.
Differential diagnosis is carried out with a wide variety of diseases, such as cementoblastoma, osteoid osteoma, fibrous dysplasia, ossifying fibroma, focal cemento-osseous dysplasia, as well as borderline malignant forms of the above pathologies and slowly progressing osteosarcoma.
Benign cementoblastoma is included in the differential diagnosis due to similar radiographic findings with osteoblastoma. The main distinctive features of cementoblastoma are revealed by careful examination of the surface of the tooth root on an x-ray, and it is also believed that the affected area by cementoblastoma looks more uniform in shadow. In this clinical case, the tumor masses did not affect the tooth, despite its very close location to it. Microscopically, these two diseases look the same, so the final diagnosis of cementoblastoma cannot be made until the fact of tooth damage is confirmed.
Another difficulty is confusing osteoblastoma with osteoid osteoma. Clinically, benign osteoblastoma does not usually cause the pain that is characteristic of osteoid osteoma. Also, osteoblastoma is a fairly large neoplasm, usually about 1 cm in diameter, and does not cause sclerosis of bone tissue, which is again characteristic of osteoid osteoma. Microscopically, the bone trabeculae of osteoblastoma are slightly wider than those of osteoid osteoma and also have a more regular orientation. Osteoblastoma has a huge number of osteoblasts, while osteoid osteoma has few giant cells and poor vascularity.
Histopathologically, ossifying fibroma and fibrous dysplasia of bone may resemble osteoblastoma, but they are typically less mineralized and mildly calcified in contrast to the large mineralized fragments of osteoblastoma. In addition, fibrous dysplasia does not appear as demarcated radiographically as osteoblastoma and may also be multifocal, which is uncommon in osteoblastoma.
Focal cemento-osseous dysplasia is a fibro-osseous lesion that may appear very similar to osteoblastoma on radiographs. However, the former is typically asymptomatic and does not damage the cortex. Most of these formations are less than 1.5 cm in diameter. Although, upon microscopic examination, both pathologies damage bone tissue in a similar way. In focal cemento-osseous dysplasia, a small number of large and actively proliferating osteoblasts are determined.
Histological examination is of paramount importance in making a final diagnosis and excluding osteosarcoma, especially the osteoblastic variant. The difficulty in distinguishing arises from the presence in osteoblastoma of modified osteoblast-like cells, similar to atypical osteosarcoma cells. In such cases, diagnosis is based on accurate interpretation of histological and radiological studies, the findings of which exclude aggressive characteristics of osteosarcoma. Bertoni and other scientists believe that the main microscopic feature that distinguishes osteosarcoma from osteoblastoma is the small number of mature trabeculae at the edge of osteosarcoma and the high penetration of this tumor into surrounding tissues.
Due to the benign nature of osteoblastoma, the main treatment is conservative excision, since recurrence is rare (13.6%) and is usually associated with a complicated course. It should also be noted that there is no uniform description of the biological behavior of this tumor. Looking at the various study reports, it becomes clear that the course of this disease varies greatly depending on the specific clinical case.
Conclusion.
The importance of the clinician understanding the tumor process and its individual course should be especially emphasized. To make a final diagnosis, it is necessary to take into account clinical and radiological data in strict conjunction with the results of histological examination. At the same time, the entire pathology must be qualitatively classified and segmented to facilitate diagnosis and prescribe appropriate, strictly specific treatment.
Authors: Harshaminder Kaur, Sonika Verma, Manveen K. Jawanda, Atul Sharma Department of Oral and Maxillofacial Pathology, College of Dental Research, Mullana, Haryana, India
Causes
The causes of bone tumors are not well understood. To a certain extent, bone cancer is caused by:
- Chronic diseases of the skeletal system ( osteomyelitis , Paget's disease , benign tumors ).
- Smoking.
- Injuries.
- Foreign body in the bone (orthopedic implants). Tumors of the skeletal system are more often detected in patients who have had implants used for osteosynthesis or have undergone joint replacement. Dentures use hexavalent chromium, which is a carcinogen.
- Previous radiation therapy , which induces the development of osteosarcoma. Radiation-induced sarcomas develop 3 years after irradiation.
- State of immunodeficiency .
- Skeletal abnormalities ( Olier disease ).
- Mutations of the p53 gene and the retinoblastoma Rb1 gene.
- Hereditary diseases ( retinoblastoma , Li-Fraumeni syndrome , Rothmund-Thompson syndrome , Werner syndrome , absent thumb).
- Benign bone tumors that can become malignant.
- Taking the drug Natpara (a drug for the treatment of hypoparathyroidism ). This drug increases the risk of osteosarcoma.
There is evidence of an increased risk of osteosarcoma in children born weighing more than 4500 g and above average height. However, in most patients no specific factors are identified.
Symptoms and manifestations of bone cancer
A characteristic manifestation of malignant bone formation of any location is constant, aching pain, disturbing for several weeks or months, not eliminated by analgesics and increasing over time.
For a long time, patients associate the appearance of pain with a former injury, so they do not consult a doctor and this becomes the reason for a late diagnosis. Pain from bone tumors does not depend on physical activity and bothers patients even at rest. Sarcoma is characterized by pain that worsens at night and relief does not occur in any position of the limb. Symptoms of osteosarcoma also include swelling of the tissue in the area of the tumor. But local swelling appears later - at first it is a deeply located tumor in the soft tissues, and then the swelling area increases, the affected area swells, and a venous network appears on the skin, sometimes the skin turns red.
When joints are affected, swelling appears in their area. Cancer of the knee joint or any other joint disrupts the function of the joints - they bend poorly and movement is limited. Movements are impaired not only when there is a tumor in the joint, but also in the nearest joint when the bone is damaged. A tumor of the joints changes their shape. In some cases, effusion appears in the joint cavity.
Photo of osteosarcoma of the knee joint
Bone cancer is accompanied by fragility, so patients often experience spontaneous fractures due to minor trauma. When the tumor process affects the spine, difficulties appear when walking, weakness in the limbs, and paretic phenomena. A tumor of the leg bones is accompanied by numbness of the limb and lameness. Symptoms of advanced bone sarcoma include abdominal pain, nausea and vomiting, which is associated with increased levels of calcium in the blood ( hypercalcemia ) due to bone breakdown. In the advanced stage, general symptoms are also noted - fatigue and weight loss. The appearance of general symptoms indicates a process with metastasis.
Symptoms of jaw cancer
Osteosarcoma that occurs in the thickness of the jaw is called central, and that developing in the peripheral parts is called peripheral. For a long time, signs of bone cancer do not appear. Then pain appears that is not associated with tooth pathology. Long-lasting pain should alert the patient. The tumor process can be recognized using radiography and MRI. With a tumor formation in the lower or upper jaw, pain in the teeth occurs for no reason and radiates to the ear and eye. It gets worse at night and becomes unbearable, forcing patients to wake up and take painkillers.
Palpation of a tumor in any part of the jaw is painful. In addition, osteogenic sarcoma of the jaw changes the sensitivity of the trigeminal nerve and causes changes in tooth position. The teeth within the tumor become mobile. paresthesia and anesthesia occurs (Vincent's symptom).
Photo of sarcoma of the lower jaw
As the jaw grows, it becomes deformed. The tumor quickly grows, spreads to the surrounding tissues and compresses them, causing exophthalmos and congestion in the soft tissues. Lymph nodes are often not enlarged. The mucous membrane of the alveolar process at the site of the tumor is red and swollen, and when the mucous membrane is injured, ulcers appear on the gums. In some cases, osteosarcoma festeres (the temperature rises, weakness and malaise appear).
Symptoms and course
Patients with malignant tumors of the jaws, of course, belong to the contingent of the most severe patients due to the difficulty and danger of surgical intervention, often great difficulties in choosing a prosthetic method, and finally, due to little hope for a favorable outcome, not only long-term, but also immediate.
The presence of a malignant neoplasm in the oral cavity often leads to disruption of eating and speech functions quite early on. A number of special conditions under which tumors of the oral cavity and jaws develop undoubtedly influence the early formation of ulcers and tumor disintegration. The temperature of the oral cavity, a humid environment, constant exposure to mechanical insults (eating) and the inability to thoroughly cleanse are the factors that make tumors prone to early ulceration if the oral mucosa is also affected by the tumor. The emerging ulcer quickly increases both in surface and in depth, due to necrosis of the bottom and walls. From this moment on, the clinical picture changes sharply for the worse, inflammatory phenomena appear to varying degrees, intoxication intensifies, and the body's resistance sharply decreases.
Intense bad breath, difficulty eating, and difficulty swallowing create especially difficult living conditions for the patient. Difficulties in eating with sarcoma of the jaw seem to play the greatest role, reducing the body's resistance. The most common cause of death in these patients is aspiration pneumonia.
The rate of tumor growth and the progression of general exhaustion of the body depends on the type of tumor and its location. Intraosseous giant cell tumors develop slowly over years. Often, squamous epithelial cancer has a long, slow course. The most intense malignant growth appears to be found in pigmented tumors, which generalize very far in a short period of time, and some sarcomas. A sharp acceleration of growth and germination into surrounding tissues can occur after mechanical trauma to the tumor. If until this moment the tumor did not give any signs, then it is sometimes extremely difficult to recognize the presence of blastomatous growth against the background of clinical phenomena after injury.
Pathological fractures of the lower jaw, due to infiltration of the entire thickness of the bone by tumor elements, are observed much more often with cancer than with sarcomas.
Enlargement of regional lymph nodes in malignant tumors of the jaws for the most part has a dual origin. On the one hand, according to anatomical conditions, there is the possibility of early and extensive damage to nodes through metastatic transfer of tumor elements. Their damage is especially pronounced in cancer of the lower jaw. On the other hand, the tendency of jaw tumors to early decay with severe inflammatory phenomena entails a reactive enlargement of the lymph nodes (of an inflammatory nature).
Lymph nodes affected by a cancerous tumor, in advanced cases, are soldered together into huge conglomerates and grow together with the surrounding tissues. When metastases break through the skin, deep, crater-shaped ulcers with purulent-ichorous discharge are formed. In slow-growing forms of sarcomas (for example, intraosseous giant cell tumor), inflammatory processes prevail in the lymph nodes.
Tests and diagnostics
- X-ray of the affected area in two projections. X-ray examination covers the entire affected bone and joints nearby. This is necessary in order not to lose sight of the “step-by-step” metastases. With osteosarcoma, the x-ray picture may be different. A large tumor node with unclear outlines. The cortex and medulla of the bone are affected. The tumor destroys the periosteum, often revealing a “cloud-shaped” component, which is associated with uneven ossification of the tumor. In the newly formed bone, osteosclerotic and osteolytic (sparse) areas alternate. However, areas of bone change become visible on x-ray when the tumor grows to a certain size. Therefore, to avoid diagnostic errors, you need to use MRI and CT.
- MRI and CT provide layer-by-layer visualization of bone, bone marrow, soft tissue and connective tissue. They are carried out with contrast. These methods clarify the size of the lesion, the exact location and spread of the tumor beyond the bone.
- To detect distant metastases, a CT scan of the chest and abdominal pelvis is performed. Chest X-ray also reveals metastases in the lungs.
- To identify lesions in other bones, skeletal scintigraphy (radionuclide scanning) is prescribed.
- The main method to confirm the disease is a biopsy and histological examination of the obtained material. The patient's bone tissue is collected and the type of tumor is determined. Tissue collection is carried out by excision of the bone, which makes it possible to obtain sufficient material. If the lymph nodes are enlarged, a biopsy (puncture) is also performed.
- Histological examination. To make a diagnosis, detection of neoplastic tissue (osteoid) is mandatory. The amount of osteoid is not important because it is different in different fields of view. Osteoid is produced by tumor cells and may be found adjacent to or surrounding the cells.
- Angiography. Detects vascular damage.
- Molecular genetic diagnostics. It determines the presence of mutations in the genome. This is necessary to determine the need for targeted therapy (biological).
Specific markers for osteosarcoma are currently unknown. Sometimes patients are prescribed a CEA test. Let's find out how necessary this is. Carcinoembryonic antigen , what is it? This is a tissue marker of cancer. What does this marker show? This type of protein is detected in minute quantities in a healthy person, but during the oncological process its level increases.
Determination of this antigen is used to diagnose the following tumors:
- colon and rectum;
- stomach;
- mammary gland;
- pancreas;
- lungs;
- metastases to the liver and bones (the sensitivity of the method in the metastatic process is much lower).
This test is not specific for malignant tumors, since an increase in antigen is observed in inflammatory and autoimmune diseases, benign tumors (intestines, liver, pancreas), liver cirrhosis , hepatitis , Crohn's disease , tuberculosis , pneumonia , cystic fibrosis . During a malignant process, the level increases throughout the entire period of the disease. CEA analysis is used to monitor the effectiveness of treatment of malignant neoplasms. A decrease in its level during the course of treatment indicates a positive result. The norm of carcinoembryonic antigen for non-smokers: 0-3.8 ng/ml, the norm for women who smoke is slightly higher than 0-5.5. A negative result does not exclude cancer.
Diagnostics
Pathological examination of a piece of tumor is very widely used in clinical practice. The general principles of the technique for taking a piece of a tumor are entirely applicable when examining tumors of the jaws. If possible, without anesthesia, a piece of tissue is cut out at the border of the healthy and tumor-invaded area. The material is processed according to certain rules of histological technique.
Puncture of the tumor with a syringe with a wide needle often (for small tumors) makes it possible to obtain a cylindrical piece of tissue suitable for making sections.
The presence of tumor infiltration, the nature of the inflammatory infiltration, the degree of differentiation of the formed elements, the number of dividing cells, the presence of special formations (pearls, giant cells, foci of necrosis, hemorrhages) are the main signs that serve as criteria for making a pathological-histological diagnosis for suspected sarcoma of the jaw .
Blood and urine testing should be performed in all cases; these studies are auxiliary diagnostic techniques that make it possible to find out, for example, the degree of anemia, the intensity of inflammatory processes, and side diseases.
X-ray examination provides a very important service in diagnosing sarcoma of the jaw. The main importance of radiographs is in determining the boundaries of the tumor. When reading a radiograph, it is necessary to find out, if possible, the area of primary localization of the tumor, its shape, relationship to neighboring organs and the degree of bone damage. Malignant tumors are characterized by vagueness (“blurring”) of the tumor boundaries. It is necessary to pay attention to the loss of bone structure, the condition of the cortical layer, and whether there is a pathological fracture. It is imperative to find out the relationship of the root tips to the tumor, which is important in differential diagnostic terms.
Diagnosis of sarcoma of the jaw is relatively simple when it is localized in accessible parts of the mucosa. Considerations regarding the age of the patient and the detection of factors causing irritation of certain parts of the oral cavity and jaws should also be taken into account in the clinical recognition of tumors.
It is much more difficult to recognize deeper tumors. In terms of symptomatology, there is a fundamental difference in the localization of sarcoma on the lower or upper jaw. In the lower jaw, the presence of a tumor can be established quite early, deformation of the dental arch, displacement of organs and formations of the floor of the oral cavity can be detected, especially with periosteal sarcomas.
If periosteal sarcomas are recognized early due to the certain availability of external examination, then central tumors developing in the thickness of the lower jaw may not show any external signs for a long time. Quite strong pain, but uncertain in localization, causeless local loosening of teeth, and often spontaneous loss of teeth - these are the most characteristic signs of a tumor developing in the central parts of the lower jaw.
With sarcomas of the upper jaw emanating from the wall of the maxillary cavity, sometimes only indirect signs can sometimes be stated, for example, neuralgic pain, darkening of the maxillary cavity, serous-purulent exudation from the nose, repeated bleeding, etc. However, these symptoms, without directly indicating the development of a tumor can give rise to diagnostic errors over a long period of time, and the true nature of the disease becomes clear only after the tumor, having occupied the entire maxillary cavity, begins to either infiltrate the nasal wall, or spread towards the alveolar process, causing loosening of the teeth, or grows outer wall of the jaw; in this case, a noticeable deformation of the face is formed with successive ulcerations through the skin.
Removal of loose teeth soon entails infiltration and germination of the walls of the free socket with tumor elements.
With cysts, the mucous membrane covering the protrusion has a normal appearance and is not inflamed; with sarcoma, the mucous membrane is often changed - swollen and hyperemic. With sarcoma, the bone wall is softened and gives in when pressed, even with a large thickness of the bone; with a cyst, the bone springs due to its thinning (softening of the cyst).
Tendency to bleeding, causeless loosening of teeth and symptoms of bone rarification are the main clinical signs that must be used to guide the differential diagnosis. Data from X-ray diagnostics and histological examination allow us to finally understand the essence and distribution of the process.
Difficult in diagnostic terms should be considered cases of development of sarcoma of the jaw from the wall of a periodontal cyst: but even here there are signs that suggest a malignant tumor: the absence of clear boundaries of the cyst, the softened spongy part of the bone and a strong tendency to bleeding during surgery and during dressings.
In conclusion, it is necessary to touch upon the differential diagnosis between a periodontal cyst and a central sarcoma of the mandible. Radiographs, physical examination and mechanical examination findings may sometimes be very similar. Anamnesis and objective data regarding the connection with the dental system do not always clarify the matter. In any case, a mixture of these completely different forms of diseases is observed.
Recognition in doubtful cases is most accurately determined by a test puncture and suction of the contents: with a cyst, a light yellow transparent liquid with cholesterol crystals (or pus) is obtained, with a tumor - blood. In cases of cysts and sarcomas, puncture sometimes fails due to the strength and thickness of the outer bone wall. It must be borne in mind that the lingual wall may also be thinned, making it difficult to touch and puncture. If the suspicion of a cyst cannot be completely eliminated, then an operative test trepanation of the bone wall is necessary.
In children
Among all tumors in children, 5% are bone sarcomas : 3% osteosarcoma and 2% Ewing sarcoma . The lack of alertness among doctors and the atypical nature of the course greatly complicate early diagnosis. Osteosarcoma in children in half of the cases is localized in the knee joint (the femur and tibia are affected). In second place is damage to the metadiaphysis of the humerus. The most common symptom of osteosarcoma is constant, dull pain with a gradual increase. Most children have a soft tissue component - swelling and an increase in the volume of the limb. Weight loss and fever at the onset of the disease are rare.
Ewing's sarcoma occurs before the age of 17 years, but the peak incidence occurs between 12 and 15 years of age. Boys are most often affected. Ewing's sarcoma, unlike osteosarcoma, does not synthesize osteoid . Often this tumor is located in the scapula, ribs, vertebrae, pelvic bones, as well as the femur, fibula, and humerus. Unlike osteosarcoma, flat bones are affected. Signs of Ewing's sarcoma are increasing pain, tissue swelling, dysfunction, and fever. The soft tissue component is more pronounced than bone destruction. An increase in local temperature due to the appearance of hemorrhages and necrosis in the tumor complicates diagnosis, since osteomyelitis is suspected. Neurological symptoms are associated with nerve damage.
Combined treatment for Ewing's sarcoma:
- Chemotherapy courses (standard drugs for this pathology).
- Surgery (similar to osteosarcoma).
- Radiation therapy. It is carried out on the area of the primary tumor and on distant metastases.
Diet
Dietary table No. 1a
- Efficacy: therapeutic effect after a week
- Terms: 3-10 days
- Cost of food: 900-1100 rubles per week
Diet table No. 5a
- Efficacy: therapeutic effect after 5-7 days
- Time frame: 2-6 weeks
- Cost of products: 1300 - 1400 rubles per week
Diet 11 table
- Efficacy: therapeutic effect after a month
- Terms: 2 months or more
- Cost of products: 1800-1900 rubles. in Week
of diarrhea while undergoing chemotherapy . In this regard, a diet excluding spicy, fatty foods containing fiber (vegetables, nuts, seeds, bran bread) is recommended.
Fried foods and simple carbohydrates, which increase intestinal motility, are also excluded. A balanced diet during this period should contain a sufficient amount of protein (boiled meat, fish, steamed cutlets, meat soufflé). Dishes must be pureed - soups, cereals, meat. During this period, you can use Diet No. 1B and No. 5P . When diarrhea disappears and the patient’s condition improves, the patient is transferred to Table No. 11 . The diet of this diet is suitable for the recovery period. The patient’s diet is complete, containing the necessary vitamins, nutrients and minerals. Daily calorie content is increased (3000 kcal). Food is taken in 5 divided doses. The goal of the diet is to normalize weight while reducing it and improve the function of all body systems.
All foods and cooking methods are allowed, but nevertheless, it is better to adhere to a healthy diet, in which preference is given to stewed, boiled or baked dishes, vegetable and cereal soups that are not fried. To replenish vitamins, the diet should contain fresh seasonal vegetables, fruits and berries. It is important to choose healthy and natural products that do not contain dyes, flavor enhancers or preservatives. The diet must contain dairy products: natural milk, kefir, cottage cheese, cheeses, yogurt. Dairy products are important for replenishing calcium, which is constantly lost from bones. The calorie content of the diet should not be increased by fatty foods, cakes, cream pies, semi-finished products, beef and lamb fat, fatty sausages, ready-made sauces, pastes, mayonnaise, and sweet carbonated water.
Prevention
There is no specific prevention. However, you can perform non-specific activities:
- Observation and treatment of precancerous diseases of the skeletal system. Processes that tend to become malignant include chondroma, fibrous degeneration, Paget's disease, and osteochondral exostoses. The malignancy rate of these benign formations reaches 15%. It is important to undergo follow-up examinations annually to detect malignancy at an early stage. Healthy lifestyle. Balanced diet. Avoiding injuries and occupational hazards.
Secondary relapse prevention includes:
- The use of drugs that restore the immune system after chemotherapy and radiation therapy .
- Complete nutrition, rich in vitamins, antioxidants, proteins.
- Rejection of bad habits.
- Prevention of viral infections.
- Preventive examinations with an oncologist. Local relapses can be detected visually. It is important to have examinations during the first 4 years. After this, local relapses are rare.
- Carrying out diagnostic procedures according to the protocol. Metastases develop in 95% of cases within the first 5 years and most often affect the lungs. Bone metastases present with pain, and they appear simultaneously with pulmonary metastases.
Diagnosis of the disease
Dental instructions for oncological diagnostics require the following activities:
- collecting a medical history and identifying the patient’s main complaints;
- visual and instrumental examination of the maxillofacial area;
- radiography of the bone tissue of the jaws;
- palpation of regional lymph nodes;
- general and detailed blood test;
- biopsy or histological analysis.
The key way to evaluate patients with osteosarcoma is radiography. On X-ray photographs, the doctor determines individual areas of bone dissolution or replacement with connective tissue.
Recently, dental oncologists have begun to actively use computed tomography, which makes it possible to detect areas of atypical ossification outside the jaw. Using this technique, the specialist also assesses the size, shape and exact location of the malignant neoplasm.
X-ray of osteosarcoma of the mandible
The final diagnosis is established only by the results of histological and cytological analysis. To do this, the surgeon removes a small area of abnormal tissue and sends it to the laboratory for microscopic analysis. Based on the results of the biopsy, a treatment and rehabilitation plan for the cancer patient is formed.
Consequences and complications
The course of the disease itself is complicated by fractures and infection of soft tissues. All bone cancers after treatment have consequences:
- Secondary cancer , which develops as a result of exposure to radiation.
- Chronic heart failure (exposure to doxorubicin ).
- Osteoporosis.
- Hearing and vision impairments.
- Renal dysfunction and renal failure .
- Endocrinopathies.
- Impaired fertility ( infertility ). Reproductive functions suffer after chemotherapy with alkylating drugs ( Ifosfamide , Carboplatin , Cyclophosphamide ) and after the use of radiotherapy in the pelvis, abdomen, and spine. Menstrual irregularities are always observed after high-dose chemotherapy and stem cell transplantation.
- The consequences of the operation are significant - after amputation, limb prosthetics and long-term rehabilitation are necessary.
Forecast
The prognosis of osteosarcoma is determined by many factors: age, size, localization, stage, “purity” of the resection margin, histological conclusion.
How long do people live with bone cancer? With complex treatment of osteosarcoma, 70% of patients live 5 years or more, with Ewing's sarcoma - 60% of patients.
Some authors give a higher survival rate. If there is a localized distal lesion, radical resection is performed and the result of chemotherapy treatment is more than 90% tumor necrosis, then 5-year survival is observed in 80% of cases.
The prognosis is worse in case of proximal localization, large tumor size, poor response to chemotherapy before surgery and metastases. Poor prognosis for tumors in the pelvic bones and weight loss at diagnosis. It is known that the intensity of tumor cell apoptosis also affects prognosis. Also unfavorable factors are early relapse, multiple lesions in the lungs and pleural involvement. If patients have stage 4, how long do they live in this case? When removing metastases in the lungs, 12-20% occur; if metastasectomy is not performed, 2.5% of patients survive. Life spans are calculated in months.
Diagnostic methods
Based on the symptoms, one can only suspect bone cancer or another disease. In order to get an accurate diagnosis, the doctor will prescribe an examination, which may include:
- Radiography . A quick and simple diagnostic method, in some cases it helps to immediately identify a tumor. If there is a suspicion of metastases in the lungs, a chest x-ray is performed.
- Magnetic resonance imaging (MRI) and computed tomography (CT) help to examine the tumor in more detail and detect growth into neighboring tissues.
- Positron emission tomography . A weak radioactive substance is injected into the body in safe doses, which accumulates most strongly in tumor cells. Then photographs are taken. This allows not only to examine the main tumor, but also to detect metastases in different parts of the body.
- General and biochemical blood tests. It is used as an additional diagnostic method to assess the general condition of a person. They can also indirectly indicate the degree of tumor aggressiveness.
- Biopsy. The most accurate diagnostic method. It is always used, even if other studies already conclusively show that the patient has bone cancer. A biopsy helps establish a final diagnosis, distinguish osteosarcoma from other tumors, and determine the degree of malignancy. The doctor may take a tissue sample with a needle or through an incision.
List of sources
- Clinical guidelines for bone sarcomas, 2022, 51 p.
- Practical recommendations for the treatment of primary malignant bone tumors (osteosarcoma, Ewing's sarcoma) / Malignant tumors. Russian Society of Clinical Oncology. 2022, pp. 283-295.
- Clinical guidelines for the diagnosis and treatment of patients with primary malignant bone tumors. 2014, 25 p.
- Clinical protocol for diagnosis and treatment. Bone sarcoma, 2015, 19 p.
- Belokon O.V., Nechval V.N. Surgical treatment of children with osteogenic sarcoma with metastases to the lungs/Health of Ukraine, 2012, pp. 34-35.