General information
Jaw tumors refer to neoplasms in the cat's tissue. This pathology accounts for 13 to 29% of the total number of dental surgical diseases.
Due to its close location to the teeth, brain and eyes, the pathology is characterized by a special clinical course. Tumor formations in this area lead to functional disorders, aesthetic defects and even death.
Depending on the tissue of which the tumor is composed, it can be osteogenic or non-osteogenic. According to the clinical development of pathologies, there are malignant, benign or locally destructive.
Treatment of jaw tumors is a complex and lengthy task that requires high competence and professionalism from the doctor.
Osteoblastoclastoma - treatment
Treatment for osteoblastoclast of the jaws is surgical. In cystic and cellular forms, careful curettage of the lesion is usually sufficient. If the tumor occupies large areas of the jawbone, it is possible to perform resection of the lower jaw, if necessary, with simultaneous bone grafting. In the lytic form, partial resection of the jaw without breaking the continuity of the mandibular bone (continuum resection) or resection of a fragment of the jaw with simultaneous bone grafting is more often used. Radiation therapy does not provide sufficient therapeutic effect. However, this method of treatment is prescribed to patients for whom any surgical intervention is contraindicated due to their general somatic status. Usually short-focus X-ray therapy, remote gamma therapy, bremsstrahlung and high-energy electron radiation are used. The average radiation dose ranges from 30–50 Gy/kg. The prognosis for treatment is favorable, but the possibility of malignancy and metastasis of the tumor due to the benign nature of the tumor cannot be excluded. Incorrect treatment tactics usually lead to relapses of the tumor process.
Published in Articles
Reasons for development
The exact mechanism of tumor development is unknown. It is generally accepted that odontogenic tumors develop under the influence of malformations of jaw tissue.
Provoking factors:
- chronic inflammatory process of tissues of the jaws and adjacent organs;
- the impact of filling composition and other foreign objects on the maxillary sinus;
- damage to the jaw bones and soft tissues due to bruises and other mechanical impacts;
- the effect of nicotine, alcohol and other chemicals on the oral cavity.
Malignant tumors develop due to the spread of metastases from cancerous tumors in other organs.
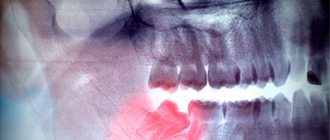
Osteoblastoclastoma - X-ray picture
Radiologically, with a cellular form of a tumor, a shadow from many small and larger cavities or cellular formations, separated from each other by bone partitions of varying thickness, is noted at the site of the lesion. No reaction from the periosteum is observed. The picture is in many ways similar to the X-ray picture of ameloblastoma.
The cystic form on the radiograph resembles an odontogenic jaw cyst and ameloblastoma. The difference between the cystic form of ameloblastoma is that its border with the bone often has fine scalloped outlines in the form of extremely small bays.
In the lytic form of osteoblastoclastoma, the tumor produces a structureless focus of clearing.
Classification and clinical course
Due to the variety of forms and stages, it is difficult to develop a unified classification of jaw tumors. The WHO classification provides for subdivision according to clinical manifestations, histology and anatomical location.
Clinical symptoms, course and prognosis are determined by the type, location and stage of the disease.
- Odontogenic benign
Ameloblastoma is a neoplasm that develops from epithelial cells with inclusions that resemble enamel in structure. Pathology affects people aged 20 to 40 years. As the tumor grows, the patient experiences pain in the jaw and teeth. An external examination reveals a dense structure, fusiform and painless thickening of the jaw bone, causing facial asymmetry. Mobility causes teeth to shift. There is a risk of developing suppuration in case of infection.
Odontomas are pathologies characteristic of children under 15 years of age. The tumor consists of hard tissue, including the pulp and periodontium. It is characterized by its small size and asymptomatic course. When it grows to large dimensions, it deforms the jaw, causing fistulas and pain.
Odontogenic fibroma is a childhood pathology that is formed from the connective tissue of the follicle and is located on both jaws. Characterized by slow, asymptomatic growth. Rarely manifested by aching pain and inflammation in the affected area. Subtype – cementing fibroma.
Cementoma is a formation of connective tissue growing into the cementum of the tooth root. The tumor is localized on the lower jaw in the area of the molars. Asymptomatic.
- Underontogenic benign
There are bone- and cartilage-forming types and osteoblastoclastoma. The list of bone-forming substances includes: osteoma, exostosis, osteophyte, etc.
Osteoma is a dense formation of mature bone tissue. It can be asymptomatic or with pronounced manifestations: pain during chewing, facial asymmetry, mobility of units.
Chondroma is a cartilaginous type of tumor. Localized in HF. It is characterized by slow growth and painlessness.
Osteoblastoclastoma is diagnosed in people under 20 years of age. Patients note a gradual increase in pain in the jaw, asymmetry of facial features, hyperthermia, and the occurrence of fistulas. There is a risk of developing fractures of the lower jaw.
- Malignant neoplasms
They occur 4 times less frequently than benign pathologies. They are odontogenic and non-odontogenic. They are characterized by severe symptoms, an aggressive course and a danger to life.
Osteogenic sarcoma. An aggressive tumor with rapid growth, pronounced pain, radiating to neighboring organs. The symmetry of the face is disrupted, infiltration of soft tissues and metastases to other organs are observed.
Carcinoma. It develops on the HF, growing into the nasal cavity. Purulent rhinitis and nosebleeds develop. When it grows into the orbit, lacrimation, exophaltmus and other complications are noted.
Diagnostics
Late diagnosis of neoplasms is due to the asymptomatic course and low oncological alertness of patients and doctors.
Diagnostic methods used:
- interviewing the patient and collecting anamnesis;
- clinical examination;
- X-ray diagnostics;
- CT;
- scintography;
- infrared thermography;
- biopsy.
If necessary, the doctor prescribes highly specialized examinations.
Treatment algorithm
When jaw tumors are detected, surgical treatment is required. The tumor is excised along with part of the adjacent healthy tissue. This reduces the risk of relapse and malignancy.
In some cases, the use of curettage is allowed. Teeth located in the problem area are subject to extraction.
Osteoblastoclastoma - microscopic picture
Microscopically, in osteoblastoclastoma, a large number of small, slightly elongated cells with a rounded nucleus (such as osteoblasts) are distinguished, among which massive accumulations of giant multinucleated cells (osteoclasts) are identified. In mononuclear cells, mitoses are observed; in multinucleated cells, they are absent. The formed elements of the tumor are also represented by fibroblasts and xanthoma cells. Areas of hemorrhage undergo a macrophage reaction with the corresponding phagocytic cells. In some areas of the tumor, islands of osteoid tissue are found. The tumor is saturated with decayed red blood cells and is imbibed by the blood pigment - hemosiderin, which gives it a brown color. The presence of the latter and multiple hemorrhages, often in the form of blood cysts, is due to the peculiarity of blood flow in the tumor.
Blood in osteoblastoclastoma circulates outside the vascular bed through intertissue gaps. The absence of endothelium allows it to penetrate the tumor tissue and accumulate there. In this case, the formed elements of the blood are destroyed, forming an accumulation of hemosiderin. Sometimes an abundance of fibrous tissue may be found in the tumor.
Diagnosis
In the diagnosis of osteoblastoclastoma, great importance is attached to x-ray examination. X-ray, O.'s picture is typical in most cases. The tumor is solitary and, as a rule, initially has an eccentric location. According to the characteristics of the growth and localization of O., its structure on the radiograph can be different. There are cellular and osteolytic variants of the structure.
Rice. 2. Radiographs of the bones of the forearm (a, b) and lower leg (c) with osteoblastoclastoma: a - direct radiograph of the proximal forearm with the cellular version of osteoblastoclastoma; the epimetaphysis of the radius is sharply swollen, with a thinned cortical layer and cellular restructuring of the spongy substance; b — direct radiograph of the distal forearm with an osteolytic variant of osteoblastoclastoma; the epimetaphysis of the radius is sharply swollen, the cortical layer is thinned or completely absent, the cellular structure of the bone substance is not determined; c — direct radiograph of the knee joint and the proximal part of the leg bones with a marginal location of osteoblastoclastoma; eccentric swelling (indicated by arrows) of the epimetaphysis of the tibia, the cortical layer is thinned, but preserved throughout.
With the cellular (trabecular) variant, the most characteristic sign is swelling of the epimetaphysis with thinning, but preservation of the cortex (Fig. 2, a). The affected bone takes on a club-shaped form. At the same time, as a result of the osteoblastic function of the tumor, a coarse cellular restructuring of the spongy substance of the epimetaphysis is observed - the appearance of large and few septa, as well as a more delicate and dense mesh. In this case, it is sometimes possible to distinguish O. from an aneurysmal bone cyst only histologically. In the structure of the tumor, as a rule, there are no deposits of calcium salts, the contours of the swollen area of the bone are quite smooth, unlike enchondroma, the edges are often characterized by the presence of speckled shadows of calcification and the wavy contour of the affected area of the bone. The affected area is clearly delimited from the adjacent unchanged parts of the bone by a thin sclerotic border, which, together with the thinned cortex, forms a tumor capsule. When the tumor spreads towards the diaphysis, the so-called telescopic transition: the diaphysis is inserted, as it were, into the swollen epimetaphysis hanging over it. Often strips of ossifying periosteum are also identified here. The fragility of the cortical substance covering the tumor, in some cases, can cause the occurrence of pathological breaks with reparative, often fringed periostosis.
The osteolytic variant of the tumor structure is observed either primarily, from the very beginning of tumor growth, or secondarily, as a result of the transition from the cellular variant. The X-ray picture is somewhat reminiscent of osteolytic sarcoma. However, in contrast to it, thinning and swelling of the cortical substance covering the changed area of the bone is observed (Fig. 2, b). The cellular structure is completely or partially absent. The swollen and thinned cortical substance can undergo almost complete resorption, but at the base of the tumor, at the site of its transition into the unchanged bone, remnants of the expanded and thinned cortical substance are usually visible, which is usually absent in osteolytic sarcoma. So-called telescopic transition of the diaphysis into the tumor in this case rentgenol. The variant is observed even more often than with the cellular one.
Radiologically, centrally located and marginal tumors are distinguished. Regional tumors (Fig. 2, c) usually do not involve the central parts of the epimetaphysis. Diagnosing them is difficult, but it is quite possible on the basis of taking into account rentgenol, signs - swelling, cellularity, absence of a periosteal visor, etc.
Osteoblastoclastoma of short and flat bones can present significant difficulties for differential rentgenol. diagnostics, since an identical picture can be given by benign Chondroblastoma (see), enchondroma (see Chondroma), reticulosarcoma of bone in the initial phases of development (see Primary reticulosarcoma of bone), in the sacrum - chordoma (see) and some -ry metastatic tumors, primarily metastases of clear cell kidney cancer and thyroid cancer, local fibrous osteodystrophy (see) and bone dysplasia (see). O. in the initial phases of malignancy cannot be radiologically distinguished from its osteolytic variant. The possibility of O.'s malignancy is indicated by the rapid growth of the tumor and the disappearance of the cellular structure. Based on the complete destruction of the tumor capsule bordering the diaphysis, the appearance of a typical periosteal visor and metastases, it can be assumed that the tumor has transformed into sarcoma.
Clinic
GKO lesions can be not only solitary, but also multiple
The clinical course of cellular and lytic forms of benign GCT is not the same. Tumors of the first group are asymptomatic for a long time and in half of the cases are detected only when a pathological fracture appears.
Lytic GCT grows quickly, the first symptom of the disease is pain of varying intensity. When the tumor is localized in the long tubular bones, it often causes rapid fatigue of the limb and lameness; when the spine is affected, the pain is predominantly radiating. Radiologically, two phases (forms) of the course of GCT are distinguished: cellular trabecular and lytic.
CT with signs of GCT: damage to the epimetadiaphysis, expansion of the medullary canal with destruction of the endosteum, swelling of the cortical layer, shell-shaped periostosis, low level of mineralization. MRI is the best method for determining the extent of GCT. It is useful for early detection of local recurrences. The GCT usually has clear contours at the border with intact bone and is often surrounded by a hypointense rim.